Abstract
Objectives
This study was conducted to investigate the pathological changes which occur in interstitial cells of Cajal (ICCs) and ganglion cells found in segments of resected bowel obtained from patients with Hirschsprung’s disease (HD), as well as to explore the benefits of using a contrast enema (CE) with 24-h delayed X-ray films to predict the length of resected bowel.
Methods
We performed a retrospective analysis of 58 children with HD who had undergone the pull-through procedure. After each operation, the ICCs and ganglion cells present in the proximal ends of the barium residue (Level A) and resected proximal bowel segment (Level B) were analyzed using immunohistochemical staining methods. Each patient was followed up for 1 year to record their stool frequency, defecation control ability, and post-surgical complications which may have occurred.
Results
Immunohistochemical staining detected fewer ICCs in Level A than in Level B (p < 0.05). However, the density of ganglion cells in the two levels was not significantly different (p > 0.05). One patient had anastomotic stricture, and five patients suffered from enterocolitis.
Conclusions
The density of ICCs was significantly lower in the bowel segments that displayed barium retention. A CE may be a valuable tool for predicting the length of bowel resection in patients with HD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hirschsprung’s disease (HD) is a common congenital gut motility disorder in children, and is characterized by a lack of ganglion cells in the myenteric and the submucosal plexuses of the distal colon [1, 2]. The length of aganglionic bowel present in HD patients can vary due to the development of an enteric nervous system and migration of neural crest-derived cells into the developing intestine during gestation. Surgical resection of the abnormal bowel segment and the pull-through procedure comprise the commonly accepted treatment for HD. When performing pull-through surgery, the aganglionic bowel segment should be completely removed; however, some patients continue to suffer from constipation after their operation due to insufficient resection of the proximal dysganglionic bowel segment [3, 4]. Previous studies have found that residual abnormal interstitial cells of Cajal (ICCs) in the bowel constitute another important reason for postoperative constipation in HD patients [5, 6]. However, it is difficult to accurately determine the length of a proximal bowel that needs to be resected when performing an operation. While preserving ICCs in an abnormal or dysganglion bowel may result in postoperative constipation, removing a section of normal innervated bowel may impair water absorption and stool control ability.
The level of colonic caliber change and transition zone as determined by a contrast enema can help predict the degree of aganglionosis and, therefore, the length of colonic segment to be resected [7, 8]. Furthermore, this information can also be used to predict whether laparoscopic assistance will be necessary during surgery or an open colectomy is indicated [7, 8]. A 24-h delayed film of a barium enema has been considered to be useful for diagnosing HD [9]. Our study was conducted to evaluate the value of determining barium residue levels in HD patients during their preoperative planning stage. Therefore, we investigated the value of using 24-h delayed X-ray results for predicting the length of proximal bowel to be resected in HD patients. We also analyzed the pathological changes of ICCs and ganglion cells in the segments of resected bowel.
Methods
Study design
This retrospective study was conducted at a single pediatric surgery center (Tongji Hospital, Wuhan, China), and enrolled 58 pediatric patients (52 males and 6 females; age range, 3 months to 6 years) who had been pathologically diagnosed as HD, and treated at our department between January 2013 and June 2015. The study protocol was approved by the Review Board of Tongji Hospital (protocol number, TJ-C20160621), and all study procedures complied with articles in the Declaration of Helsinki.
The study inclusion criteria consisted of having undergone preoperative testing with a 24-h delayed film of a barium enema, and prior experience being treated with the pull-through procedure. Although several of the patients had received conservative therapy (e.g., colonic irrigation, enema, or high doses of lactulose) for several months prior to surgical treatment, all of the enrolled patients ultimately received surgical treatment, and their final diagnosis was confirmed by a postoperative pathological examination.
When performing CE, barium is slowly injected into the colon through a soft catheter until the shape of the colon becomes clearly visible. During CE procedures, the dose of water-soluble barium varied from 50 to 100 mL, depending on the age and weight of the patient, all patients were re-examined 24 h later, and the colon morphology was analyzed on anteroposterior and lateral X-ray films. To decide the amount of barium retention levels, anatomic landmarks such as the rectosigmoid junction, sigmoid-descending colon junction, haustrum and caliber change were used. The barium retention levels were compared with the colonic morphology change during operation.
The transanal Soave pull-through procedure was used in patients with short segment HD, and the laparoscopic-assisted transanal endorectal pull-through procedure was used in patients with long segment HD. Intraoperatively obtained frozen sections were used to determine the boundaries of the aganglionic bowel segment, and 24-h delayed X-ray films were used to predict the length of the resected proximal bowel (Fig. 1). Based on our experience, if the intraoperative frozen section showed the presence of ganglion cells in barium retention level, the proximal bowel resection length was set at 5–10 cm proximal to the presence of barium residue; if the intraoperative frozen section showed that barium retention areas was absent in ganglion cells, the proximal bowel resection length was at least 5–10 cm proximal to the presence of ganglion-containing bowel tissue. For each resected specimen, two pieces of intestine were collected at the proximal ends of the barium residue level (Level A) and at the margin of the proximal resected bowel level (Level B). Each specimen consisted of full thickness bowel tissue. The bowel specimens were immediately placed into formaldehyde and fixed for 24 h.
Immunohistochemistry staining
Paraffin-embedded sections of bowel tissue were deparaffinized in xylene and rehydrated through a graded ethanol series; after which, microwave antigen retrieval with citric acid buffer was performed for 15 min. Nonspecific binding was blocked by incubating each tissue section with 5 % bovine serum albumin for 1 h at room temperature. The sections were incubated with either rabbit anti-c-kit antibody (1:200, Abcam; Cambridge, MA, USA) or mouse anti-NeuN antibody (1:100, Proteintech; Wuhan, China) at 4 °C overnight. Following incubation, the sections were washed three times in phosphate-buffered saline solution and then incubated with horseradish peroxidase-conjugated secondary antibody. Positive reactions were confirmed by staining with diaminobenzidine. Cell nuclei were stained with hematoxylin. The stained sections were examined with a Nikon E800 Microscope (Tokyo, Japan), and Image-Pro Plus 6.0 software (Media Cybernetics; Rockville, MD, USA) was used to quantify the integrated optical density of each image. Ganglion cells were counted by identifying strong nuclear and moderate cytoplasmic immunoreactivity for neuronal marker NeuN [10]. The interstitial cells of Cajal were indentified c-kit immunostained area in the muscle layers and myenteric plexuses and counted.
Statistical analyses
All results are presented as the mean ± standard deviation (SD). Statistical differences between two levels were calculated using the Student’s t test and Graph Pad Prism, version 5.0 software. p values <0.05 were considered statistically significant.
Results
CE and surgical findings
CE examinations with 24-h delayed X-ray films showed that all the patients displayed barium retention. In 35 cases (60.3 %), the barium residue was located in the rectosigmoid colon, and in 15 patients (25.9 %), barium residue was located in the sigmoid-descending colon. In the other 8 patients (13.8 %), the barium residue was located at or above the splenic flexure. Figure 2 shows 24-h delayed X-ray findings in an 8-month-old boy.
A transition zone was clearly observed in 44 patients (75.8 %), but was absent in the remaining 14 patients (24.2 %).The relationship between the caliber change and the proximal ends of the barium residue in CE was analyzed; there were 42 patients (72.4 %) whose proximal ends of the barium residue located more proximal side of the caliber change; the other 16 patients (27.6 %) had proximal ends of the barium residue located distal side of the caliber change. The intraoperative frozen section from 53 patients (91.4 %) displayed ganglion cells in Level A, while sections obtained from the remaining 5 patients (8.6 %) did not have ganglion cells in Level A. Among those five patients, three patients with barium residue located in the rectosigmoid colon lacked ganglion cells, and two patients with barium residue located in the splenic flexure colon lacked ganglion cells, thus the bowel resection length in those five patients extended 5–10 cm above the first appearance of ganglion cells in an intraoperative frozen section.
All 58 patients in the study were diagnosed as HD by a postoperative pathological examination. The mean bowel resection length in patients with barium residue located in the rectosigmoid colon was 21.4 ± 4.6 cm, compared to 27.5 ± 3.7 cm in patients with barium residue located in the sigmoid-descending colon. The mean bowel resection length in patients with barium residue located at the splenic or hepatic flexure was 44.3 ± 11.5 cm.
Immunohistochemistry staining for ICCs and ganglion cells
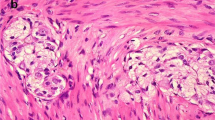
Results of c-kit immunohistochemical staining showed significantly fewer c-kit positive cells in Level A (Fig. 3a) when compared with Level B (p < 0.05) (Fig. 3b), and this finding was verified by calculating the mean optical density of c-kit positive cells in each level (Table 1). When barium residue was located in the rectosigmoid colon, the density of c-kit positive cells in Level A was lower than that in Level B; however, the difference was not statistically significant (p = 0.10). In contrast, when the barium residue was located in the sigmoid-descending colon and at the splenic or hepatic flexure, the difference in c-kit staining density between the two levels was statistically significant (p < 0.05).
c-kit immunohistochemistry results for the colon wall of the boy described in Fig. 1 (×200 magnification). a c-kit expression in Level A. b c-kit expression in Level B. Quantitative analysis of c-kit expression levels revealed that the mean optical density in Level A (0.373) was significantly less than that in Level B (0.470; p < 0.05)
NeuN immunohistochemistry staining was used to detect ganglion cells. The staining results showed that NeuN-positive cells were present at both Levels A and B within the myenteric plexus (Fig. 4). The two levels of myenteric plexus showed no difference in their intensities of NeuN expression (Table 1).
NeuN immunohistochemistry results for the colon wall of the boy described in Fig. 1 (×200 magnification). a NeuN expression in Level A. b NeuN expression in Level B. Quantitative analysis of NeuN expression levels revealed that the difference between Level A (0.485) and Level B (0.493) was not statistically significant (p > 0.05)
Follow-up results
Most children defecated once a day and had good ability of defecation control, except 1 patient had anastomotic stricture 4 months after operation, this patient was resolved by 3 months’ anus dilatation. For complications, five patients developed Hirschsprung’s-associated enterocolitis (HAEC). Among them, two patients presented with mild explosive diarrhea 1–2 months postoperatively; one patient had moderate abdominal distension associated with moderate fever 2 weeks after operation, the other two patients suffered from fever and vomiting 2–4 weeks after operation. All of them were hospitalized and recovered after conservative treatment. Moreover, there were one patient with anastomotic stricture and three patients had HAEC in the group whose proximal ends of the barium residue located more proximal side of the caliber change, the other two patients with HAEC in the group whose proximal ends of the barium residue located distal side of the caliber change.
Discussion
Coordinated gastrointestinal motility is dependent on interactions which occur between the enteric nervous system and ICCs. In the current study, we examined the pathological changes which occurred in segments of bowel resected from patients with Hirschsprung’s disease. While ganglion cells displayed similar levels of distribution in the specimens of barium retention bowel and more proximal bowel walls, lower density of ICCs was found in the specimens of barium retention bowel when compared with their density in the margin of the proximal resected bowel.
Although CE has lower levels of sensitivity and specificity (70 and 83 %, respectively) than rectal suction biopsy (93 and 98 %, respectively) and anorectal manometry (91 and 94 %, respectively) when used for preoperative work-up of HD patients, CE is the test most often used to screen children with suspected HD [11]. Morphological changes in the colon can be clearly seen by a contrast barium enema, and a patient’s intestinal emptying function can be evaluated by examining 24-h delayed X-ray films [11]. Moreover, our own prior study confirmed that barium should be completely drained within 24 h in healthy children [12]. If 24-h delayed X-ray films show barium retention in the intestine, poor intestinal peristalsis should be suspected.
While most patients did well after a one-stage repair operation, a small number of patients suffered from postoperative complications. Several studies have shown that the presence of residual bowel tissue containing abnormal ICCs can result in functional motility disorder and postoperative constipation in HD patients [5, 13–16]. The pathological changes of ICCs include reduced numbers of myenteric ICCs and disrupted myenteric ICC networks in segments of aganglionic bowel and the transition zone; moreover, the numbers of ICCs in the bowel muscular layer are markedly reduced [13, 14]. Puri [14, 15] found that some HD patients had reduced numbers of ICCs in their proximal ganglionic bowel, and that insufficient resection of such bowel may be a cause of motility disturbances and recurrent constipation.
An ability to precisely examine the areas of proximal bowel is very important for preventing postoperative complications. The presence of a radiographic transition zone is the most reliable radiological sign of HD, and its location is highly correlated with the level of aganglionosis [17, 18]. Furthermore, the location of the transition zone provides valuable information for preoperative planning [17]. If the transition zone is at the level of the mid-sigmoid colon or more distal, a transanal pull procedure is usually performed [17]. If the transition zone has a higher location or is absent, the laparoscopic-assisted pull-through procedure should be the first choice of treatment [17]. Additional studies have confirmed that the correlation between the transition zone seen on a barium enema and the pathological transition zone can reach 85.7 % [9]. While the location of the transition zone can be used for predicting the length of resected bowel in HD patients, the transition zone is not symmetrical, and a biopsy taken at one point may not really reflect the numbers and quality of ganglion cells throughout the bowel circumference [19]. Detail analyses of the transition zone suggest that abnormalities may exist at locations up to 10–15 cm proximal to the first appearance of ganglion cells [3].
The intraoperative frozen section biopsy is a fundamental surgical procedure performed when there is a need to examine ganglion cells. To better examine a dysfunctional bowel, Bettolli [20] developed a rapid tissue fixation and immunostaining protocol for use in the operating room. That procedure used c-kit staining to identify ICCs and NF68 peptide staining to identify neurons. However, the time span required for immunoprocessing was 1–3 h, which is longer than the amount of time needed to examine a standard intraoperative frozen section.
We predicted bowel morphology and function by performing a CE procedure with 24-h delayed X-ray films and examining intraoperatively obtained frozen sections of bowel tissue. During surgery, the extent of aganglionic bowel was determined by examining an intraoperative frozen section, and the length of proximal bowel to be resected was determined by examining 24-h delayed X-ray films. Our results indicated that if barium retention occurred in the sigmoid colon or rectum 24 h after its administration, mega-rectosigmoid resection was feasible. If 24-h delayed X-ray films indicated obvious dilation of the more proximal colon, and barium was retained in the descending colon or at the splenic flexure, a subtotal colectomy should be considered. The length of bowel resected was generally 5–10 cm beyond the proximal levels of barium residue or the point at which ganglion cells were first identified in the intraoperative frozen section.
We analyzed the c-kit positive ICCs and ganglion cells found in the sections of resected bowel. Abundant myenteric plexus ICCs surrounded by plexuses were found in the margins of proximal resected bowel, but these structures were rarely found in specimens of barium retention bowel. Furthermore, the density of ICCs in specimens of barium retention bowel was significantly lower than the density of ICCs in specimens of resected proximal bowel (Fig. 2, Table 1). It should be noted that when barium retention occurred in the rectosigmoid region, the density of c-kit positive cells in samples of barium retention bowel was lower than that in samples of resected proximal bowel, but the difference was not statistically significant. This was partly due to the short course of the disease or limited aganglionosis in the short segment of HD. We also analyzed the ganglion cells present in resected proximal bowel and barium retention bowel, and found no obvious differences. These results are consistent with previous findings which indicated an abnormal distribution of ICCs in the ganglion bowel of HD patients [5, 16]. Moreover, the mean bowel resection length in our study was in close agreement with the recommended range of 10–15 cm above a normal biopsy specimen [21]. In this study, we did not compare the density of ICCs and ganglion cells in HD patients with those in normal children, as there was no suitable specimen for making the comparison. Furthermore, there were more patients with complications whose proximal ends of the barium residue located more proximal side of the caliber change, which may indicate that potential reduction of the ICCs in normoganglionoic segment may be associated with the post-surgical complications.
A 24-h delayed film of a barium enema is helpful for diagnosing HD, and patients who display contrast reagent being retained up to the cecum in a 24-h delayed film image have a high incidence of HD [9]. We studied the pathological changes which occurred in samples of resected bowel tissue, and found an abnormal distribution of ICCs in barium retention bowel. This discovery may explain why barium retention in the bowel is indicative of poor intestinal peristalsis.
Conclusion
The 24-h delayed X-ray films in conjunction with results from a histologic examination of an intraoperative frozen tissue section were helpful for surgical planning. These results encourage radiologists and pediatric surgeons to obtain and examine 24-h delayed X-ray films for purposes of improving the accuracy of HD diagnosis and predicting the length of abnormal bowel during a surgical planning process.
References
Haricharan RN, Georgeson KE (2008) Hirschsprung disease. Semin Pediatr Surg 17(4):266–275
Langer JC (2013) Hirschsprung disease. Curr Opin Pediatr 25(3):368–374
Coe A, Collins MH, Lawal T et al (2012) Reoperation for Hirschsprung disease: pathology of the resected problematic distal pull-through. Pediatr Dev Pathol 15(1):30–38
Friedmacher F, Puri P (2011) Residual aganglionosis after pull-through operation for Hirschsprung’s disease: a systematic review and meta-analysis. Pediatr Surg Int 27(10):1053–1057
Gfroerer S, Rolle U (2013) Interstitial cells of Cajal in the normal human gut and in Hirschsprung disease. Pediatr Surg Int 29(9):889–897
Wang H, Zhang Y, Liu W et al (2009) Interstitial cells of Cajal reduce in number in recto-sigmoid Hirschsprung’s disease and total colonic aganglionosis. Neurosci Lett 451(3):208–211
Frongia G, Günther P, Schenk JP et al (2016) Contrast Enema for Hirschsprung disease investigation: diagnostic accuracy and validity for subsequent diagnostic and surgical planning. Eur J Pediatr Surg 26(2):207–214
Pratap A, Gupta DK, Tiwari A et al (2007) Application of a plain abdominal radiograph transition zone (PARTZ) in Hirschsprung’s disease. BMC Pediatr 7:5
Wong CW, Lau CT, Chung PH et al (2015) The value of the 24-h delayed abdominal radiograph of barium enema in the diagnosis of Hirschsprung’s disease. Pediatr Surg Int 31(1):11–15
Yang S, Donner LR (2002) Detection of ganglion cells in the colonic plexuses by immunostaining forneuron-specific marker NeuN: an aid for the diagnosis of Hirschsprung disease. Appl Immunohistochem Mol Morphol 10:218–220
de Lorijn F, Kremer LC, Reitsma JB, Benninga MA (2006) Diagnostic tests in Hirschsprung disease: a systematic review. J Pediatr Gastroenterol Nutr 42(5):496–505
Zhang HY, Feng JX, Huang L et al (2008) Diagnosis and surgical treatment of isolated hypoganglionosis. World J Pediatr 4(4):295–300
Yamataka A, Kato Y, Tibboel D et al (1995) A lack of intestinal pacemaker (c-kit) in aganglionic bowel of patients with Hirschsprung’s disease. J Pediatr Surg 30(3):441–444
Rolle U, Piotrowska AP, Nemeth L, Puri P (2002) Altered distribution of interstitial cells of Cajal in Hirschsprung disease. Arch Pathol Lab Med 126(8):928–933
Rolle U, Piaseczna-Piotrowska A, Puri P (2007) Interstitial cells of Cajal in the normal gut and in intestinal motility disorders of childhood. Pediatr Surg Int 23(12):1139–1152
Vanderwinden JM, Rumessen JJ, Liu H et al (1996) Interstitial cells of Cajal in human colon and in Hirschsprung’s disease. Gastroenterology 111(4):901–910
Proctor ML, Traubici J, Langer JC et al (2003) Correlation between radiographic transition zone and level of aganglionosis in Hirschsprung’s disease: implications for surgical approach. J Pediatr Surg 38(5):775–778
Kapur RP, Kennedy AJ (2012) Transitional zone pull through: surgical pathology considerations. Semin Pediatr Surg 21(4):291–301
Langer JC (2012) Laparoscopic and transanal pull-through for Hirschsprung disease. Semin Pediatr Surg 21(4):283–290
Bettolli M, Rubin SZ, Staines W et al (2006) The use of rapid assessment of enteric ICC and neuronal morphology may improve patient management in pediatric surgery: a new clinical pathological protocol. Pediatr Surg Int 22(1):78–83
Langer J, Caty M, de la Torre-Mondragon L et al (2007) IPEG colorectal panel. J Laparoendosc Adv Surg Tech A 17(1):77–100
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (No. 81270441).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Rights and permissions
About this article
Cite this article
Chen, X., Zhang, H., Li, N. et al. Pathological changes of interstitial cells of Cajal and ganglion cells in the segment of resected bowel in Hirschsprung’s disease. Pediatr Surg Int 32, 1019–1024 (2016). https://doi.org/10.1007/s00383-016-3961-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3961-7