Abstract
Purpose
Recognition of physical child abuse is imperative for ensuring children’s safety. Screening tools (ST) may increase identification of physical abuse; however, the extent of their use is unknown. This study assessed use of STs for physical abuse in children’s hospitals and determined attitudes regarding STs.
Methods
A web-based survey was sent to child abuse program contacts at 103 children’s hospitals. The survey assessed institutional use of a ST for physical abuse and characteristics of the ST used. Respondents were asked to identify benefits and liabilities of STs used or barriers to ST use.
Results
Seventy-two respondents (70 %) completed the survey; most (64 %) were child abuse pediatricians. Nine (13 %) respondents reported using a ST for physical abuse; STs varied in length, population, administration, and outcomes of a positive screen. Most respondents (86 %) using a ST felt that it increased detection of abuse. Barriers noted included lack of time for development and provider completion of a ST.
Conclusions
While few respondents endorsed use of a ST for physical abuse, most believed that it increased detection of abuse. Future research should focus on development of a brief, uniform ST for physical abuse which may increase detection in at-risk children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An estimated 3.6 million reports of possible child abuse or neglect involving approximately 6.6 million children were made to child protective services (CPS) in the United States in 2014 [1]. Of these reports, roughly 60 % were investigated by CPS. Approximately 702,000 children were determined to be the victims of abuse or neglect, of which 119,517 (17 %) were the victims of physical abuse. In 2014, 1580 children died as a result of child abuse or neglect [1].
The actual number of children who are victims of physical abuse and neglect is estimated to be much higher, as it is believed that many cases of physical abuse are unrecognized and, therefore, unreported due to lack of physician knowledge and skills to recognize, diagnose, and report injuries suspicious for physical abuse [2]. Sheets et al. found that 27.5 % of infants with abusive head trauma had sustained a previous sentinel injury that was concerning for abuse, as compared to a control group of non-abused infants in which none of the children sustained a previous sentinel injury [3]. These findings suggest that these injuries are an opportunity for healthcare providers to intervene and prevent additional harm.
Many children who are the victims of child abuse present initially to the Emergency Department (ED); therefore, the ED plays a critical role in identifying and further evaluating children whose injuries are concerning for physical abuse. Several screening tools have been proposed to increase detection of physical child abuse in EDs, both in the US and abroad [4–9]. The most common format is a checklist designed to help establish the level of concern for physical abuse. A systematic review of this type of screening tool showed that it increased the rate of detection of suspected cases of physical abuse, improved documentation in the patient’s medical record, and raised awareness of abuse among ED staff [10]. In addition to enabling earlier detection of abuse, the use of a screening tool may also help to reduce bias in identifying potential victims of abuse. For example, children of minority race or lower socioeconomic status (SES) are more likely to undergo evaluation for physical abuse [11–13]; a standardized screening tool could help ensure that these factors do not drive decision-making. At this time, there is not a validated screening tool for child physical abuse in the US.
While it is likely that many children’s hospitals are using some type of screening protocol for physical abuse, there is little research on this topic and certainly no consensus on the best screening method. There are many challenges to systematic screening for physical abuse in EDs, including a lack of time for thorough evaluation and questioning, a lack of understanding and/or awareness of child abuse by ED staff, difficulty in communicating with parents/caregivers in the case of suspected abuse, a lack of a hospital-wide screening policy, high turnover of ED staff, and a lack of availability of a child abuse pediatrician or team [14]. Despite these challenges, it remains critical to detect child abuse early, while maintaining as low a false positive rate as possible. The goal of this study is to assess the use and characteristics of screening protocols for physical abuse in children’s hospitals and to determine attitudes regarding the use of such tools.
Materials and methods
A web-based survey was sent via electronic mail to child abuse program contacts at 103 children’s hospitals. Contacts were identified through collaboration with the National Association of Children’s Hospital and Related Institutions and included clinicians, social workers, and administrators who worked with their hospital child protection team. Study data were managed using REDCap (Research Electronic Data Capture) hosted at Nationwide Children’s Hospital [15].
The self-administered survey was developed by a working group of child abuse pediatricians, pediatric trauma surgeons, and research scientists. The survey was piloted among a group of physicians at Nationwide Children’s Hospital for feedback on content and clarity. This feedback guided revisions to the final version of the survey, which is shown in Online Resource 1.
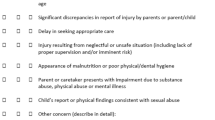
Respondents were asked about their position at their institution and the presence of an individual or team that specializes in evaluating children for concerns of child abuse at their institution. The survey then assessed the institutional use of a screening tool for physical abuse and characteristics of the screening tools being utilized, including which patients are screened, who performs the screening, and the response to a positive screen. Respondents who endorsed the use of a screening tool were asked to identify the perceived benefits and liabilities of the tool. Respondents who denied using a screening tool were asked to identify perceived barriers to using such a tool.
Descriptive statistical analyses were performed, with frequencies and percentages used to describe categorical responses. All analyses were performed in SAS v9.3 (SAS Institute, Cary, NC, USA).
Results
Seventy-two respondents (70 %) completed the survey. The majority of the respondents (n = 46, 64 %) identified themselves as child abuse pediatricians (Table 1). All respondents reported having an individual or team at their institution that specializes in child abuse pediatrics. Respondents represented 36 states and the District of Columbia; six respondents (8 %) did not indicate their state. There was no significant difference between respondents and non-respondents with regard to their occupation, type of facility (pediatric program versus children’s hospital within a hospital versus freestanding children’s hospital), size of the hospital, or region of the country.
Nine (13 %) respondents reported using a standardized tool to screen for concerns of child abuse. Five of the respondents provided the length of the screening tool with two tools consisting of one question and one tool each consisting of three, twelve, and fifteen questions. The majority of respondents with a tool identified that the screening was done by a nurse (n = 8, 89 %). Participants also identified that screening may be done by social workers (n = 4, 44 %) and healthcare providers (physician, nurse practitioner, or physician assistant) (n = 4, 44 %). One respondent (11 %) reported that the screening tool was self-administered by the patient/parent.
The majority of respondents who endorsed use of a screening tool (n = 7, 78 %) reported that children of all ages are included in the screening, one respondent (11 %) reported that children under 5 years old are included, and one respondent (11 %) reported that age of children included in the screen varied depending on the presence of a suspicious injury. The populations of children targeted by the screening tool also varied with five respondents (56 %) reporting that all children seen in the ED are screened, five (56 %) reporting that all children admitted to the hospital are screened, and one (11 %) reporting all children seen in outpatient clinics are screened.
A positive screening tool resulted in consultation of a child abuse pediatrician or team at six (75 %) of respondents’ institutions (Table 2). Other possible outcomes of a positive tool included a consult to social work, report to CPS, additional lab work or imaging, or further questioning of the family. Respondents that endorsed use of a screening tool reported that they felt it increased detection of abuse (n = 6, 86 %), decreased bias in considering abuse (n = 5, 71 %), and decreased risk of liability to the institution (n = 5, 71 %). Perceived liabilities of the screening tool by this group included decreased patient satisfaction (n = 3, 75 %), increased length of hospital stay (n = 1, 25 %), increased burden on CPS (n = 1, 25 %), and increased burden on child abuse pediatricians (n = 1, 25 %).
Among the 63 (88 %) respondents who reported that their institution does not use a standardized tool to screen for concerns of child physical abuse, 15 (24 %) reported lack of time for developing a screening policy as a perceived barrier to the use of such a tool (Table 3). Other barriers identified included the respondent does not feel such a tool is necessary, lack of time for completion of a screening tool, lack of support from managers and/or hospital board, lack of understanding and/or awareness of child abuse, lack of community resources, and difficulty communicating with caregivers in the case of suspected abuse.
Respondents were given the opportunity to describe additional barriers to implementation of a tool for screening for child physical abuse. The most common barrier (38 %, n = 14) noted was lack of a validated, effective screening technique for abuse.
Discussion
Of the 72 children’s hospitals included in this survey, only 13 % identified that a standardized screening tool is being used for detection of child physical abuse. The tools in use vary substantially in content, administration, and outcome of a positive screen, as would be expected as there are no screening tools that have been validated in the US reported in the literature. Regardless of these variations, the majority of respondents who endorsed use of a screening tool felt that it improved detection of child physical abuse and decreased bias in considering abuse.
Of the respondents who denied using a standardized screening tool for abuse, the most common barrier identified was lack of time for the development of a screening policy. Many of the respondents who did not endorse use of a screening tool reported that they did not use such a tool because no validated, evidence-based screening tool for physical abuse exists, which is consistent with similar research in the United Kingdom and the Netherlands [10, 14, 16–18]. This group also reported that while they may not use a specific screening tool, their institutions have implemented educational efforts and various forms of protocols for the evaluation of concerns of abuse. This study highlights the need for the development of a brief, uniform screening tool for child physical abuse which can potentially increase abuse detection and decrease bias in evaluating at-risk children.
In the Netherlands, Louwers and colleagues developed a 6-item checklist to screen for child abuse in all children less than 18 years of age seen in three EDs [17, 18]. In a prospective cohort study, they found that the checklist was completed on 48 % of patients (n = 18,275) with a positive screen on 2.3 % of checklists [17]. The overall sensitivity of the checklist was 0.80 and specificity was 0.98. They also found potential child abuse cases were more likely to screen positive on at least one question of the checklist. In a separate cohort study of the same checklist, Louwers and colleagues found that the detection rate of children screened for child abuse was higher than those children who were not screened [18]. Both of these studies were limited in that fewer than half of patients presenting to EDs were screened using the checklist; furthermore, this study was conducted in the Netherlands where EDs are now legally required to screen every child for child abuse. With further study in broader settings, use of such checklists may be helpful in identifying children at risk for abuse.
This study has several limitations. Variation may exist in how respondents interpreted the questions and answer choices. Specifically, an explicit definition of “standardized screening tool” was not provided in the survey. In addition, respondents were limited in how they could respond to many of the questions. Furthermore, this study is specific to the responses of child abuse contacts at children’s hospitals.
In summary, few children’s hospitals are utilizing a standardized tool for screening for child physical abuse. Use of such a tool could improve detection of abuse and reduce the risk of further harm to at-risk children. In the development of protocols to screen for child physical abuse, it is important to consider that children who are ultimately victims of abuse may initially present with a variety of complaints that may be non-specific, i.e. “fussiness”, and it is important to keep child maltreatment of all forms in the differential diagnosis. Future research needs to focus on development and validation of a brief screening tool for child physical abuse.
References
US Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth, and Families, Children’s Bureau (2016) Child Maltreatment 2014. http://www.acf.hhs.gov/programs/cb/research-data-technology/statistics-research/child-maltreatment. Accessed 21 Mar 2016
Flaherty EG, Sege RD, Griffith J et al (2008) From suspicion of physical child abuse to reporting: primary care clinician decision-making. Pediatrics 122:611–619
Sheets LK, Leach ME, Koszewskim IJ et al (2013) Sentinel injuries in infants evaluated for child abuse. Pediatrics 131:701–707
Sittig JS, Uiterwaal CSPM, Moons KGM, Nieuwenhuis EES, van de Putte EM (2011) Child abuse inventory at emergency rooms: CHAIN-ER rationale and design. BMC Pediatr 11:91
Benger JR, Pearce V (2002) Simple intervention to improve detection of child abuse in emergency departments. Brit Med J 324:780–782
Chang DC, Knight VM, Ziegfeld S, Haider A, Paidas C (2005) The multi-institutional validation of the new screening index for physical child abuse. J Pediatr Surg 40:114–119
Clark KD, Tepper D, Jenny C (1997) Effect of a screening profile on the diagnosis of nonaccidental burns in children. Pediatr Emerg Care 13:259–261
Louwers ECFM, Korfage IJ, Affourtit MJ et al (2012) Effects of systematic screening and detection of child abuse in emergency departments. Pediatrics 130:457–464
Escobar MA, Pflugeisen BM, Duralde Y et al (2016) Development of a systematic protocol to identify victims of non-accidental trauma. Pediatr Surg Int 32:377–386
Louwers ECFM, Affourtit MJ, Moll HA, de Koning HJ, Korfage IJ (2010) Screening for child abuse at emergency departments: a systematic review. Arch Dis Child 95:214–218
Lane WG, Dubowitz H (2007) What factors affect the identification and reporting of child abuse-related fractures? Clin Orthop Relat R 461:219–225
Lane WG, Rubin DM, Monteith R, Christian CW (2002) Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA J Am Med Assoc 288:1603–1609
Laskey AL, Stump TE, Perkins SM, Zimet GD, Sherman SJ, Downs SM (2012) Influence of race and socioeconomic status on the diagnosis of child abuse: a randomized study. J Pediatr 160:1003–1008
Louwers EC, Korfage IJ, Affourtit MJ, Koning HJ, Moll HA (2012) Facilitators and barriers to screening for child abuse in the emergency department. BMC Pediatr 12:167
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Hoytema van Konijnenburg EMM, Teeuw AH, Zwaard SA et al (2014) Screening methods to detect child maltreatment: high variability in Dutch emergency departments. Emerg Med J 31:196–200
Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE (2008) Performance of screening test for child physical abuse in accidental and emergency departments. Health Technol Asses 12(33)
Louwers ECFM, Kourfage IJ, Affourtit MJ et al (2014) Accuracy of a screening instrument to identify potential child abuse in emergency departments. Child Abuse Neglect 38:1275–1281
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Crichton, K.G., Cooper, J.N., Minneci, P.C. et al. A national survey on the use of screening tools to detect physical child abuse. Pediatr Surg Int 32, 815–818 (2016). https://doi.org/10.1007/s00383-016-3916-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3916-z