Abstract
Purpose
Breast masses in children and adolescents are uncommon and the vast majority are benign. There are currently limited analyses of breast masses in this population and clinical management is highly variable between institutions and providers. The purpose of our study is to analyze the demographics, pathology and management of 119 pediatric patients with breast masses; one of the largest studies to date.
Methods
We performed a retrospective review of patients who underwent excision of a breast mass at a single pediatric center from June 2009 to November 2013. Demographics, imaging, pathology and management were reviewed.
Results
Average patient age was 15.3 years, average mass size was 3.15 cm and 20.3 % had a family history of breast cancer. 68 % of patients had pre-operative ultrasound, and 31.9 % underwent a period of observation. The most common indication for resection was patient and family anxiety. All masses were benign, with fibroadenoma being the most common histopathology (75.2 %).
Conclusions
In our cohort there were no cases of malignancy. Only 31.9 % of patients underwent some form of observation and patient or family anxiety was the most common indication for proceeding with surgery. This suggests that patient anxiety may result in unnecessary operation. Our data may help reassure patients, families and providers that the risk of malignancy is low and could help develop more optimal management strategies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast masses are rare in children and adolescents, with an estimated incidence of 3.25 % [1]. Malignant breast masses are even less common, with breast carcinoma representing less than 1 % of all childhood cancers and less than 0.1 % of all breast cancers [2–4]. The differential diagnosis for a pediatric breast mass is broad. Fibroadenomas represent the most common breast pathology in adolescence, constituting 30–50 % of masses in medical series and 44–94 % of masses in surgical series [5, 6]. Fibroadenomas tend to be slow growing and regress with age in up to 10–40 % of patients [1, 5, 6]. They are also almost always benign, with a documented malignant transformation rate of less than 0.3 % [5, 7]. Juvenille fibroadenomas are defined as rapidly growing fibroadenomas in the adolescent population. Phyllodes tumors are closely related to fibroadenomas; however, they may be locally destructive and have the potential to be malignant [5]. While there are some clinical and imaging characteristics, such as size and rapid growth, that may distinguish phyllodes tumors from fibroadenomas, definitive diagnosis can only be obtained from histology [3–5].
In contrast to the management of breast masses in adults, there is currently a wide variation in the treatment protocols for pediatric breast masses. Given the low rate of malignancy, guidelines for management of pediatric breast lesions typically recommend a conservative approach [1, 3, 5, 8]. Masses without alarming clinical or radiographic characteristics can be observed for several months for spontaneous regression. In addition to concerns about malignancy, excision may be warranted in cases of rapidly growing masses, as these may distort developing breast architecture [5]. Recommended indications for surgical excision include rapid growth, diameter greater than 5 cm, persistence without regression, systemic symptoms, personal history of malignancy or radiation and concerning features on imaging [3, 5]. However, in the wake of increasing public awareness of breast cancer in adults, patients and families may experience significant anxiety, and often prefer operative management for definitive diagnosis.
Methods
A retrospective review of all pediatric breast masses surgically excised from June 2009 to November 2013 at a single tertiary children’s hospital was performed. Data was collected from the electronic medical record in compliance with IRB approval and recorded in Microsoft Excel. Demographic data collected included patient age at surgery, gender, past medical history, body mass index, family history of breast disease, size of mass and symptoms. Data on clinical course were also collected, including imaging studies, biopsy results, clinical care plan, indication for surgery and specimen pathology.
Results
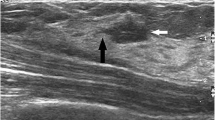
A total of 135 masses removed from 119 patients were reviewed. 117 (98.3 %) of the patients were female and only 2 (1.7 %) of the patients were male (Table 1A). The pathology of the breast masses in the 2 male patients demonstrated one case of galactocele and one case of ductal ectasia. The average age was 15.3 years with a range of 1.17–19 years. On average patients presented after 25.7 weeks of symptoms; however, this was highly variable (Table 1B). Mass size ranged between 0.8 and 13.2 cm with an average size of 3.2 cm. 58 % of patients underwent documented diagnostic ultrasound (Table 1B). The percent of patients receiving pre-operative ultrasound did not change significantly over time from 2010 to 2013 (data not shown). We have published a detailed analysis of the ultrasound results of this population separately [9].
Overall, 48.4 % of patients received some form of initial work-up by their primary physician, including ultrasound imaging and/or biopsy (Fig. 1a). Only two patients underwent imaging other than ultrasound. One patient had a PET/CT due to a personal history of cancer and one patient had a mammogram ordered at an outside hospital. The percentage of patients undergoing an initial work-up prior to referral to surgery remained relatively constant throughout the study period. Only 31.9 % of patients underwent some period of observation ordered by either their primary medical doctor (PMD) or by their surgeon. This number did increase over the time period of the study with 66.7 % of patients receiving some period of observation in 2013 (Fig. 1b).
Evaluation and management of breast lesions. a Percentage of patients who underwent work-up by their primary medical doctor (PMD) prior to surgical evaluation. Work-up includes any imaging (ultrasound, mammogram, PET/CT) and any biopsy. b Percentage of patients who underwent a period of observation prior to surgery. Observation was ordered by PMD (white), or by surgeon (black)
We also analyzed the indications for surgical excision documented for each operative encounter. Indications included abnormal imaging results, continued growth of mass, pain, size and patient anxiety. The most common indication for excision was anxiety, with 23.5 % of patients and families requesting excisional biopsy. This trend was more apparent in the later years of the study (Fig. 2).
We next analyzed the pathology of the surgical specimens. In our series all masses were benign. The most common pathologic diagnosis was, as expected, fibroadenoma constituting 75.2 % of masses (Table 2). Other common diagnoses included juvenile fibroadenoma, tubular adenoma, pseudoangiomatous stromal hyperplasia (PASH), supernumerary nipple, benign cyst and fibrocystic changes.
Discussion
Pediatric breast masses are very rare and the vast majority are benign. While the general recommendation is observation of non-suspicious lesions, practice habits vary widely. Here we examined 119 patients from a single tertiary center who underwent surgical excision of breast masses during a 4.5-year period. Demographic analysis of our population revealed a similar profile to other studies [10–14], with the majority of patients being females in mid-adolescence. Multiple studies have shown that higher body mass index (BMI) in adolescence has a protective effect on both benign and malignant breast disease [15–17]. Consistent with previous reports, the patients in our series had an average BMI of 22.4, within the normal range. Ultrasound is the most common modality of evaluating breast masses in the pediatric population and 58 % of our study population underwent pre-operative ultrasound.
In our series only 31.9 % of patients underwent some period of observation, either recommended by their primary medical doctor (PMD) or by their surgeon. While this percentage is low, the overall rates of conservative management increased from 6.7 % in 2009 to 40 % in 2013. In addition, the most common documented indication for surgical excision was patient and family anxiety. The histologic analysis of surgical specimens demonstrated that all lesions excised in this population were benign.
Taken together, these data suggest that the wide variation in clinical practice in the treatment of pediatric breast masses may be leading to unnecessary operations. A common indication for surgical excision was patient and family anxiety, which is not unexpected given the current level of awareness of adult breast cancer.
A standardized approach for management of breast masses is well established in adults. However, there is no standard protocol for evaluation or management of breast masses in children and adolescents. Ultrasound is the imaging modality of choice given dense breast tissue in pediatric patients and the desire to minimize radiation exposure. In adults, the American College of Radiology Breast Imaging Reporting and Data System (BI-RADS) classification is used to stratify risk of malignancy and guide management [18]. However, in both our series and others the BI-RADS system has not shown good concordance between imaging characteristics and mass pathology [9, 11]. This indicates that a new imaging classification may be necessary in children and that observation may be the optimal management, even in patients with BI-RADS 4 imaging findings. Cytologic examination by fine needle aspiration or core biopsy is rarely used in an effort to avoid repeated invasive procedures in children [19, 20]. Recommended observation periods of pediatric breast masses vary from one to four menstrual cycles [1, 3, 21] with no standard guideline.
While surgical excision is necessary in certain clinical scenarios, encouraging initial periods of observation may prevent unnecessary surgeries. This can be approached by both the PMD and by the surgeon. Focusing on allaying patient and family concerns about malignancy may also decrease the number of patients requesting excisional biopsy.
References
Neinstein LS, Atkinson J, Diament M (1993) Prevalence and longitudinal study of breast masses in adolescents. J Adolesc Health 13:277–281
Kaneda HK, Mack J, Kasales CJ, Schetter S (2013) Pediatric and adolescent breast masses: a review of pathophysiology, imaging, diagnosis and treatment. Am J Roentgenol 200:W204–W212
Fallat ME, Ignacio RC (2008) Breast disorders in children and adolescents. J Pediatr Adolesc Gynecol 21:311–316
Gutierrez JC, Housri N, Koniaris LG, Fischer AC, Sola JE (2008) Malignant breast cancer in children: a review of 75 patients. J Surg Res 147:182–188
Jayasinghe Y, Simmons PS (2009) Fibroadenomas in adolescence. Curr Opin Obstet Gynecol 21:402–406
De Silva NK, Brandt ML (2006) Disorders of the breast in children and adolescents, part 2: breast masses. J Pediatr Adolesc Gynecol 19:415–418
Sklair-Levy M, Sella T, Alweiss T, Cracium I, Libson E, Mally B (2008) Incidence and management of complex fibroadenomas. AJR Am J Roentgenol 190(1):214–218
Greenberg R, Skornick Y, Kaplan O (1998) Management of breast fibroadenomas. J Gen Intern Med 13:640–645
Koning JL, Davenport KP, Poole PS, Kruk PG, Grabowski JE (2015) Breast imaging-reporting and data system (BI-RADS) classification in 51 excised palpable pediatric breast masses. J Pediatr Surg 50(10):1746–1750
West KW, Rescorla FJ, Scherer LR, Grosfeld JL (1995) Diagnosis and treatment of symptomatic breast masses in the pediatric population. J Pediatr Surg 30:182–187
Bock K, Duda VF, Hadji P, Ramaswamy A, Schulz-Wendtland R, Klose KJ, Wagner U (2005) Pathologic breast conditions in childhood and adolescence: evaluation by sonographic diagnosis. J Ultrasound Med 24:1347–1354
Tea MKM, Asseryanis E, Kroiss R, Kubista E, Wagner T (2009) Surgical breast lesions in adolescent females. Pediatr Surg Int 25:73–75
Ezer SS, Oguzkurt P, Ince E, Temiz A, Bolat FA, Hicsonmez A (2013) Surgical treatment of the solid breast masses in female adolescents. J Pediatr Adolesc Gynecol 26:31–35
Vargas HI, Vargas MP, Eldrageely K, Gonzalez KD, Burla ML, Venegas R, Khalkhali I (2005) Outcomes of surgical and sonographic assessment of breast masses in women younger than 30. Am Surg 71:716–719
Frazier AL, Rosenberg SM (2013) Preadolescent and adolescent risk factors for benign breast disease. J Adolesc Health 52:S36–S40
Ahlgren M, Melbye M, Wohlfahrt J, Sorensen TIA (2004) Growth patterns and the risk of breast cancer in women. N Engl J Med 351:1619–1626
Berkey CS, Willett WC, Frazier AL, Rosner B, Tamimi RM, Colditz GA (2011) Prospective study of growth and development in older girls and risk of benign breast disease in young women. Cancer 8:1612–1620
D’Orsi CJ, Bassett WA et al (2003) Mammography. Breast imaging reporting and data system (BI-RADS), 4th edn. American College of Radiology, Restona, pp 1–259
Kennedy RD, Boughey JC (2013) Management of pediatric and adolescent breast masses. Semin Plast Surg 27:19–22
Michala L, Tsigginou A, Zacharakis D, Dimitrakakis C (2015) Breast disorders in girls and adolescents. Is there a need for a specialized service? J Pediatr Adolesc Gynecol 28:91–94
Vade A, Lafita VS, Ward KA, Lim-Dunham JE, Bova D (2008) Role of breast sonography in imaging of adolescents with palpable solid breast masses. AJR Am J Roentgenol 191:659–663
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Knell, J., Koning, J.L. & Grabowski, J.E. Analysis of surgically excised breast masses in 119 pediatric patients. Pediatr Surg Int 32, 93–96 (2016). https://doi.org/10.1007/s00383-015-3818-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3818-5