Abstract
Purpose
To conduct a systematic review and meta-analysis of studies comparing the perimeatal-based flap (PBF) and tubularized incised-plate (TIP) techniques for primary hypospadias repair and determine whether the two techniques had similar reported outcomes.
Methods
The PubMed, Embase and Cochrane databases were searched using the terms: hypospadias, Snodgrass, TIP*, tubularized incised plate, tubularized incised-plate, Mathieu*, perimeatal-based flap, perimeatal flap, meatal-based flap and meatal based flap. No other limits were used. Inclusion criteria included: primary hypospadias repair only; both including the PBF and TIP techniques; at least one of the quantitative outcomes obtainable from study; comparative studies.
Results
Twelve studies fulfilled the inclusion criteria and were included in the final analysis. Meta-analysis showed that there were no significant differences between the two techniques when comparing fistula (OR = 1.47; 95 % CI: 0.82–2.63; P = 0.20), meatal stenosis (OR = 0.53; 95 % CI: 0.24–1.16; P = 0.11), and wound dehiscence (OR = 0.82; 95 % CI: 0.24–2.84; P = 0.76). Both the studies which assessed cosmesis objectively showed a consistent better cosmetic result of the TIP technique (P < 0.05).
Conclusion
There were no significant differences of complication rates between the two techniques, and the TIP technique was usually of better cosmesis. Given the large clinical heterogeneity among studies, future more well-designed studies with full data and uniform criterion were awaited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are more than 300 surgical procedures for hypospadias repair, however, controversy continues over the ideal technique. Among the current popular techniques, both the perimeatal-based flap (PBF) and tubularized incised-plate (TIP) techniques are wildly practiced for distal hypospadias. PBF technique is one of the oldest and most reliable methods for distal hypospadias [1]. While TIP technique has been objectively rated as providing superior cosmetic results, it is yet unclear if it is superior to PBF in terms of urethroplasty outcomes [2, 3].
A previous systematic review of the postoperative complication rates following distal hypospadias surgery using the PBF and TIP techniques was published online by Wilkinson et al. [4] in December 2010. It represented a summary of all case series which published before December 2009. However, the levels of evidence included were very low (level 4) according to the Oxford Center for Evidence-Based Medicine [5], and the statistical method used was also limited because of using the Fisher’s exact test methodology and not considering the variability of each study [6]. This review concluded that both the two techniques had been shown to have low rates of postoperative complications, and there was no clear consensus on the ideal method of repair for distal hypospadias. Because of many confounding factors not adjusted, the authors determined strict inclusion and exclusion criteria and conducted subgroup analysis. Due to lack of data, however, it was difficult to make a sound explanation on the inconsistent results which derived from the subgroup analysis. All these limitations weakened the strength of the systematic review.
In the present study, we conducted a systematic review and meta-analysis of studies comparing the PBF and TIP techniques for primary hypospadias repair and determined whether the two techniques had similar reported outcomes.
Methods
The eligibility determination, quality assessment and data extraction for each study were conducted independently by two of the authors (FRW and YHX) and conflicts were resolved by a third author (HJZ).
The systematic search of the literature was performed using the electronic databases of PubMed (1950–), Embase (1988–) and Cochrane databases. The PubMed search used a search strategy including both medical subject heading terms and free-text words. The following terms were used: hypospadias, Snodgrass, TIP*, tubularized incised plate, tubularized incised-plate, Mathieu*, perimeatal-based flap, perimeatal flap, meatal-based flap and meatal based flap. No “language” or other limits were used. The searches on Embase and Cochrane Library used the same words (“Appendix”). Subsequently, the query results were pooled. All titles and abstracts were reviewed initially to select studies for full review if they contained results of primary hypospadias repair including both the PBF and TIP techniques. Where the relevance of a study was unclear a review of the full text was undertaken. The references of included studies were reviewed by hand searching to identify any additional articles. When multiple reports describing the same population were published, only the most recent or complete data were used. The last search was in October 2012.
Our inclusion criteria were as follows: primary hypospadias repair only; including both the PBF and TIP techniques; at least one of the outcomes obtainable from study; comparative studies. Editorials, letters, review articles, case reports, animal experimental studies and duplicate patient series were excluded.
The PBF and TIP techniques were carried out according to the description of Mathieu in 1932 [7] and Snodgrass in 1994 [8], respectively. The techniques in our study also included modified techniques because modification in general was made to improve the outcome of a certain technique and was a normal step of evolution. Dorsal plication or free tunica vaginalis patch grafts were used when severe ventral curvature was present.
We extracted data from each study using a predefined data extraction form. The variables assessed included first author, publication year and type, level of evidence, patient age and number, length of follow-up, patient characteristics, surgical techniques and details (coverage of the neo-urethra, suture material and fashion, urinary diversion), and postoperative outcomes (fistula, meatal stenosis, wound dehiscence and cosmesis). We tried to contact the corresponding authors when data were missing. Level of evidence and publication type was classified according to the Oxford Center for Evidence-Based Medicine [5]. The criteria for reporting postoperative outcomes were rarely defined and therefore accepted as per the authors’ description, in particular with the subjective outcomes (meatal stenosis and cosmesis). For example, meatal stenosis was considered as inability to pass a stent with a certain caliber (8F or 10F) at a certain age (1-year-old or 1 month after surgery).
We hypothesized a priori that the direction and magnitude of surgical outcomes among studies may differ depending on whether the studies had a type of RCT or cohort study, whether the surgeons used a standard or modified technique, and whether surgical techniques had different surgical details. Therefore, we sought to conduct a series of subgroup analysis to test the assumption: (1) the modified PBF technique might generate better surgical outcomes, (2) double-layer coverage of the neo-urethra and a thinner urethroplasty suture might be related to a lower fistula rate, (3) a stent with greater caliber might be related to a lower rate of meatal stenosis, (4) double-layer coverage and a thinner glansplasty suture might be related to a higher dehiscence rate.
The effect measures estimated were odds ratio (OR) for dichotomous data and weighted mean difference for continuous data, both reported with 95 % confidence interval (CI). Statistical heterogeneity was assessed using the Chi square test with significance set at P < 0.10 and the I 2 statistics [9]. Given the significant clinical heterogeneity between studies, the random-effects model was used for all comparisons. Evidence for publication bias was ascertained with funnel plot. All analyses were performed with software available from the Cochrane Initiative (Review Manager 5.2).
Results
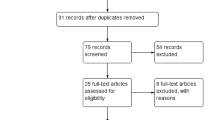
From the 94 citations initially identified, 12 studies [2, 3, 10–19] including 690 cases (338 cases for PBF and 352 cases for TIP) fulfilled the predefined inclusion criteria and were included in the final analysis (Fig. 1). The data extraction were displayed in Tables 1 and 2, respectively. Agreement between the two reviewers (FRW and YHX) was 97.4 %.
Study and patient characteristics
Among the included studies, there were seven RCTs [10–12, 15, 16, 18, 19] and five cohort studies [2, 3, 13, 14, 17], eleven studies [2, 3, 10–15, 17–19] published as full-text articles and one [16] as abstract, and nine studies [2, 3, 10, 12, 14, 15, 17–19] published in English and three [11, 13, 16] in other languages. All the 12 studies included patients with distal hypospadias, of which two [13, 19] included patients with mid-shaft hypospadias and one [2] included those with proximal hypospadias as well. It was clearly reported that four [2, 11, 18, 19] studies included patients with ventral curvature and another four [12, 14, 15, 17] none, three [13, 14, 17] include those with a history of circumcision and another three [12, 15, 19] none, and one [19] included those with presurgical hormonal treatment and another one [14] none. Three studies [14, 18, 19] clearly reported patients with healthy ventral penile skin, one [18] reported those with meatal stenosis, and one [19] reported those with shallow urethral groove. There were also some variations in the surgical procedures, as shown in Table 3.
Fistula
Ten studies [10–19] assessed fistula for the included 626 patients and showed a non-significant difference between the PBF and TIP techniques except for one [16] with a same fistula rate between them (20 %). Meta-analysis of the ten studies revealed that the fistula rate after PBF procedure did not significantly differ from that after TIP (OR = 1.47; 95 % CI: 0.82 to 2.63; P = 0.20), as shown in Fig. 2a.
Meatal stenosis
Ten studies [10–19] evaluated meatal stenosis of the PBF and TIP techniques, of which only three [15, 17, 18] clearly defined the meatal stenosis. Aminsharifi [15] regarded a narrow stenotic meatus as less than 10F. Yildiz [17] defined that the size of the sounds passing through the neo-urethra was less than 8F in 1-year-old children or 10F in those aged >1 year. Elganainy [18] considered that the neo-urethra was unable to pass an 8F catheter at 1 month after surgery.
Among the ten studies, two [14, 16] indicated that the stenosis rate of PBF was same with that of TIP (10 and 11.1 %, respectively), one [18] showed a lower rate of meatal stenosis with PBF than with TIP, and the others [10–13, 15, 17, 19] revealed a non-statistically significant difference between the two techniques. Pooling the data of the ten studies demonstrated that the meatal stenosis rate of PBF did not significantly differ from that of TIP (OR = 0.53; 95 % CI: 0.24 to 1.16; P = 0.11), as shown in Fig. 2b.
Wound dehiscence
Ten studies [10–19] reported wound dehiscence, of which four study [12, 15, 18, 19] showed no dehiscence existing in both the PBF and TIP groups, one study [14] revealed a same rate of wound dehiscence between them (2.2 %), while the rest five studies [10, 11, 13, 16, 17] provided a non-statistical difference for both techniques. The pooled data of the six studies [10, 11, 13, 14, 16, 17] indicated no significant difference between the PBF and TIP techniques (OR = 0.82; 95 % CI: 0.24 to 2.84; P = 0.76), as shown in Fig. 2c.
Cosmesis
Ten studies [2, 3, 10, 11, 14–19] evaluated the cosmetic result of the PBF and TIP techniques for at least one certain aspect of the penile appearance (meatus, glans, shaft or overall appearance).
Among these, three studies [11, 16, 19] evaluated cosmesis subjectively and showed a satisfactory overall cosmesis for both techniques. Another two studies [2, 3] evaluated cosmesis with an objective scoring system and showed a consistently higher score for the TIP technique (P < 0.05). Of these, one study [2] graded the penile appearance (meatus, glans, shaft or overall appearance) as poor, unsatisfactory, satisfactory or very good (points 1–4), and the other one [3] reported that the overall appearance was scored between 0 (the worst) and 10 (the best).
Six studies [10, 11, 14, 15, 18, 19] described the shape of urethral meatus and showed that all the meatus after the TIP and modified PBF techniques were slit-like while most meatus after the standard PBF technique was distorted, rounded, horizontal or oval. Two studies [17, 18] described the appearance of penile shaft, of which one study [18] found no deformities of the shaft while the other one [17] noted mild penile torsion in all the patients with single-layer coverage of the neo-urethra (PBF 16 and TIP 26, respectively) which was rotated laterally.
Subgroup analysis
To explore the effect of methodological quality and the variations in surgical procedures, subgroup analyses were conducted across publication type (RCT or cohort study), the PBF technique (standard or modified), coverage of the neo-urethra (single-layer or double-layer), suture for urethroplasty (6/0 or 7/0) and glansplasty (4/0, 6/0 or 7/0), and the stent for urinary diversion (6–8F or 8–10F), as shown in Table 4. Subgroup analyses showed a basically consistent result with the total effect except for the analysis of meatal stenosis. When restricted to RCTs and the studies with the modified PBF technique, it was noted that the rate of meatal stenosis after PBF was significant lower than that after TIP (P = 0.03 and P = 0.01, respectively).
The modified PBF technique generated a lower complication rate and a better cosmesis of meatus. Double-layer coverage of the neo-urethra and the 7/0 urethroplasty suture generated a lower fistula rate except for the 7/0 suture used in the PBF technique. An 8–10 F stent for urinary diversion resulted in a lower rate of meatal stenosis. Double-layer coverage of the neo-urethra and the 6/0 or 7/0 glansplasty suture resulted in a higher dehiscence rate, but not for the case of double-layer coverage in the TIP technique.
Publication bias
Possible publication bias was analyzed by generating funnel plots of the studies used for all of the evaluated comparisons of outcomes. Only one study [17] lied outside the 95 % CI and the funnel plots of fistula, meatal stenosis and wound dehiscence showed no obvious asymmetry, suggesting little evidence of publication bias, as shown in Fig. 3.
Discussion
This review identified seven RCTs and five cohort studies that compared the PBF and TIP techniques for primary repair of hypospadias. To the best of our knowledge, it was the first study that systematically reviewed and synthesized all relevant comparative studies. The level of evidence on which this review was based ranged from 2b to 1b. It showed that both the two techniques were effective for primary hypospadias repair, with low rates of postoperative complications. We found that there were no significant differences of the complication rates (fistula, P = 0.20; meatal stenosis, P = 0.11; wound dehiscence, P = 0.76), and the TIP technique was usually of better cosmesis.
There were many factors that might influence the repair of hypospadias. So, we attempted to conduct a comprehensive subgroup analysis. However, some critical factors (e.g. presence of the ventral curvature and previous penile surgery, quality of the penile skin, and configuration of the corpora) were rarely documented. Because of the inadequate adjustment for confounding factors, it was difficult to make any positive conclusions, in particular with that of meatal stenosis. The inconsistent result of meatal stenosis might be attributed to the random-effects model which was used in the total analysis, because the effect became significant when fixed-effects model was applied.
Fistula was the most common complication after hypospadias repairs. Our pooled analysis showed a fistula rate of 11.5 and 7.99 % for the PBF and TIP techniques, respectively. However, when we looked at a study of TIP repair on a large sample, the fistula rate was 1–2 % [20]. Therefore, what was happening in the current review did not present the surgeons who had large experience. So, we could not conclude that the PBF and TIP techniques had the same fistula rate. Many variables might be related to fistula. In this review, we were limited in our ability to take full account of them as they were rarely documented. Our subgroup analysis showed that the modified PBF technique and double-layer coverage of the neo-urethra might be associated with a lower fistula rate, but it was not the case for the urethroplasty suture.
Meatal stenosis was the second common complication after hypospadias surgery, with a rate of 2.88 and 7.67 % for the PBF and TIP techniques, respectively. It was reported [21] that an obstructive flow pattern was more common in patients undergoing TIP versus PBF. Our pooled estimates also showed a slightly higher rate of meatal stenosis for the TIP technique although there was no statistical significance in the present effects model. The causes for meatal stenosis were still unclear. It has been suggested that meatal stenosis most often indicated a technical error, including failure to incise the plate to near the corpora (resulting in an inadequate diameter) and tubularization of the urethral plate too far distally [20, 22]. Our subgroup analysis, however, with the limited data indicated that the modified PBF technique and a stent with a greater caliber for urinary diversion might be relevant to a lower rate of meatal stenosis.
We found the wound dehiscence to be reported in 1.6 and 2.56 % of patients for the PBF and TIP techniques, respectively, while the two large sample studies [23, 24] showed that the dehiscence occurred in 4–5 % of the patients after TIP repair. Therefore, wound dehiscence was not rare, as it might instead be an underreported complication. The study [23] using the simple and multiple logistic regressions indicated that anatomical and/or host factors (wound healing) were more important than age, type of suture or preoperative testosterone use in the development of dehiscence. Meta-analysis showed that there was no significant difference of dehiscence rate, which indicated that dehiscence was not related to the technique applied. Although our subgroup analysis demonstrated that dehiscence might be partially attributed to the modified PBF technique and glansplasty sutures, it was not always the case as the dehiscence rate of TIP was as low as that of PBF when stratified by the modified technique, and the 6/0 suture did not result in a lower rate by contrast to the 7/0 suture.
Cosmesis was a very important subjective outcome. All the three studies [11, 16, 19] which evaluated cosmesis subjectively showed a satisfactory overall cosmesis for both techniques. However, it was reported that there was a significant disparity of opinion between patients and surgeons [25]. Therefore, the objective scoring systems were attempted to assess the cosmesis, although there was yet no uniform criterion. Both the included studies [2, 3] which evaluated cosmesis objectively showed a consistent better cosmetic result of the TIP repair. Furthermore, we also found a better cosmesis of meatus after TIP as well as the modified PBF procedure. Accordingly, the superior cosmetic result provided by TIP technique was probably because it created a vertical slit-like meatus, which was also what the modified PBF technique aimed to. It had been claimed that modifications of the PBF repair, by incising the urethral plate, improved the cosmetic result and did not increase the incidence of stricture by a longer follow-up [26, 27]. The experience further supported the assumption that the modified PBF technique might generate better surgical outcomes.
Our study has several limitations. First, some critical data were rarely documented as described above, so we could not fully adjust the confounding factors. Given the significant clinical heterogeneity, we used random-effects model, and thus our conclusions were more conservative. Next, there was a lack of uniform criteria for reporting the subjective outcomes. Therefore, our analysis was based on an assumption that these criterions were similar enough to be assessed together. Nevertheless, the cosmetic result was still difficult to be merged into meta-analysis. Accordingly, future more well-designed studies with full data and uniform criterion are awaited.
Fortunately, this study still provided us with some valuable information. First, the level of evidence on which our review was based was relatively high, although our conclusion was not significantly different from that reached earlier [4]. Second, given the standard deviation of each study and the difference in sample sizes, we used the Review Manager software and the Mantel–Haenzel test. All these made our results more convincing. Furthermore, we provided the most up-to-date information in this area.
References
Yesildag E, Tekant G, Sarimurat N et al (2004) Do patch procedures prevent complications of the Mathieu technique? J Urol 171:2623–2625
Ververidis M, Dickson AP, Gough DC (2005) An objective assessment of the results of hypospadias surgery. BJU Int 96:135–139
Scarpa M, Castagnetti M, Musi L et al (2009) Is objective assessment of cosmetic results after distal hypospadias repair superior to subjective assessment? J Pediatr Urol 5:110–113
Wilkinson DJ, Farrelly P, Kenny SE (2012) Outcomes in distal hypospadias: a systematic review of the Mathieu and tubularized incised plate repairs. J Pediatr Urol 8:307–312
Oxford Centre for Evidence-based Medicine Levels of Evidence (2001) Centre for Evidence-Based Medicine Web site. http://www.pdptoolkit.co.uk/Files/ebm/cebm/Doing%20ebm/levelsofevidencetable.htm
Tuduri I (2012) Commentary to outcomes in distal hypospadias: a systematic review of the Mathieu and tubularized incised plate repairs’. J Pediatr Urol 8:313
Hadidi AT, Azmy AF (2004) Hypospadias surgery: an illustrated guide. Springer, Berlin
Snodgrass W (1994) Tubularized, incised plate urethroplasty for distal hypospadias. J Urol 151:464–465
Higgins JP, Thompson SG, Jj Deeks et al (2003) Measuring inconsistency in meta-analysis. BMJ 327:557–560
Oswald J, Körner I, Riccabona M (2000) Comparison of the perimeatal-based flap (Mathieu) and the tubularized incised-plate urethroplasty (Snodgrass) in primary distal hypospadias. BJU Int 85:725–727
Guo Y, Ma G, Ge Z (2004) Comparison of the Mathieu and the Snodgrass urethroplasty in distal hypospadias repair. Zhonghua Nan Ke Xue 10:916–918
Moradi M, Moradi A, Ghaderpanah F (2005) Comparison of Snodgrass and Mathieu surgical techniques in anterior distal shaft hypospadias repair. Urol J 2:28–31
Ugras MY, Ergin H, Kilic S et al (2006) Factors affecting success in surgery for mid- and distal penile hypospadias: a comparative study of Mathieu and TIPU techniques. Turk Uroloji Dergisi 32:375–380
Anwar-ul-haq, Akhter N, Nilofer et al (2006) Comparative study of Mathieu and Snodgrass repair for anterior hypospadias. J Ayub Med Coll Abbottabad 18:50–52
Aminsharifi A, Taddayun A, Assadolahpoor A et al (2008) Combined use of Mathieu procedure with plate incision for hypospadias repair: a randomized clinical trial. Urology 72:305–308
Samore MA, Malik MA, Iqbal Z (2006) Management of distal hypospadias: Mathieu’s repair versus tubularized incised plate urethroplasty. Pak J Surg 22:154–158
Yildiz A, Bakan V (2010) Comparison of perimeatal-based flap and tubularized incised plate urethroplasty combined with single- or double-layer dartos flap in distal hypospadias. Urol Int 84:265–268
Elganainy EO, Abdelsalam YM, Gadelmoula MM et al (2010) Combined Mathieu and Snodgrass urethroplasty for hypospadias repair: a prospective randomized study. Int J Urol 17:661–665
Nezami BG, Mahboubi AH, Tanhaeivash R et al (2010) Hypospadias repair and glans augmentation using a modified Mathieu technique. Pediatr Surg Int 26:299–303
Snodgrass WT, Bush N, Cost N (2010) Tubularized incised plate hypospadias repair for distal hypospadias. J Pediatr Urol 6:408–413
Scarpa MG, Castagnetti M, Berrettini A et al (2010) Urinary function after Snodgrass repair of distal hypospadias: comparison with the Mathieu repair. Pediatr Surg Int 26:519–522
Lorenzo AJ, Snodgrass WT (2002) Regular dilatation is unnecessary after tubularized incised-plate hypospadias repair. BJU Int 89:94–97
Snodgrass W, Cost N, Nakonezny PA et al (2011) Analysis of risk factors for glans dehiscence after tubularized incised plate hypospadias repair. J Urol 185:1845–1849
Eliçevik M, Tireli G, Sander S (2004) Tubularized incised plate urethroplasty: 5 years’ experience. Eur Urol 46:655–659
Mureau MA, Slijper FM, Slob AK et al (1996) Satisfaction with penile appearance after hypospadias surgery. The patient and the surgeon’s view. J Urol 155:703–706
Ali T, Porkolab Z (2002) Modified Snodgrass and Mathieu technique for treatment of hypospadias. BJU Int 89:75
Soliman SM (2002) A naturally appearing glanular meatus after a Mathieu procedure combined with Snodgrass incision/hinge of the plate. BJU Int 89:75
Acknowledgments
None.
Conflict of interest
The authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
F. Wang, Y. Xu and H. Zhong are joint first authors and contributed equally to the paper.
Appendix Search strategy used in the systematic search
Appendix Search strategy used in the systematic search
PubMed:
Hypospadias[mh] AND (Snodgrass OR TIP* OR “tubularized incised plate” OR “tubularized incised-plate”) AND (“perimeatal-based flap” OR Mathieu* OR “perimeatal flap” OR “meatal-based flap” OR “meatal based flap”).
EMBase:
‘Hypospadias’/exp AND (Snodgrass OR tip* OR ‘tubularized incised plate’ OR ‘tubularized incised-plate’) AND (‘perimeatal-based flap’ OR Mathieu OR ‘perimeatal flap’ OR ‘meatal-based flap’ OR ‘meatal based flap’).
Cochrane:
Hypospadias AND (Snodgrass OR TIP OR “tubularized incised plate” OR “tubularized incised-plate”) AND (“perimeatal-based flap” OR Mathieu OR “perimeatal flap” OR “meatal-based flap” OR “meatal based flap”).
Rights and permissions
About this article
Cite this article
Wang, F., Xu, Y. & Zhong, H. Systematic review and meta-analysis of studies comparing the perimeatal-based flap and tubularized incised-plate techniques for primary hypospadias repair. Pediatr Surg Int 29, 811–821 (2013). https://doi.org/10.1007/s00383-013-3335-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-013-3335-3