Abstract
Purpose
The correlation between radiographic transition zone on contrast enema in Hirschsprung’s disease and the total length of aganglionosis is known to be inaccurate. The aim of our study was to analyse this correlation more precisely to improve preoperative planning of the corrective surgery.
Methods
From 1998 to 2009, 79 patients were operated on for Hirschsprung’s disease. All available preoperative contrast enemas (n = 61) had been single blind reviewed by the same radiologist who defined the radiographic transition zone when present in vertebral level. Four groups were determined (rectal, rectosigmoid, long segment, and absence of transition zone) and by Kappa coefficient of agreement correlated to the length of aganglionosis in the pathological report.
Results
Radiological findings were concordant with the specimen in pathology in 8 cases of 19 in rectal form (42 %), in 20 cases of 35 in rectosigmoid form (57 %), in all 6 cases of long-segment form (100 %), in the 2 cases of total colonic form (100 %) with a global agreement of 58.1 %, κ = 0.39 CI [0.24; 0.57].
Conclusion
Correlation between level of radiographic transition zone on contrast enema and length of aganglionosis remains low. Systematic preoperative biopsy by coelioscopy or ombilical incision is mandatory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diagnosis of Hirschprung’s disease (HD) relies on a pathological proof by preoperative rectal succion biopsy now considered as gold standard [1], and may be completed in some cases by rectal manometry [2].
Contrast enema (CE) previously used for diagnosis is now employed to evaluate the extent of HD [3]. Till now, this is the only non-invasive exploration in routine at the surgeon’s disposal to assess the level of aganglionosis and plan the corrective surgery: single-stage transanal pull-through for rectosigmoid disease (RSHD), and laparoscopic techniques for long-segment disease (LSHD) requiring more proximal colon mobilization [4, 5].
Radiographic transition zone (RTZ) is known to be the most reliable radiological sign to evaluate the level of aganglionosis [6], but with partial matching results with the real length of aganglionosis in previous studies [3, 4].
The aim of our study was to try to correlate more precisely radiological and pathological findings to improve preoperative planning of the corrective surgery using a standardized method.
Patients and methods
Demographic data
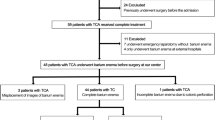
We retrospectively reviewed all patients operated on for HD from 1998 to 2009. Among 79 patients, 61 were identified with both CE available and pathology report defining the total length of aganglionosis after surgery. Eighteen CE were unavailable for review because of 8 derivations at birth (2 ileostomy and 6 colostomy), and the remaining 10 CE were performed out of our center, and these films were not available for review.
There were 23 girls (29 %) and 56 boys (71 %), operated with a mean age at surgery of 17 days (range 6–4,080). Patients’ characteristics are detailed in Table 1.
Radiological analysis
All CE (n = 61) were single blind reviewed by the same radiologist who was aware of the clinical presentation but not of the specimens’ results.
Therefore, twenty CE performed in patients <2 years old with no HD, were added to the study, so the radiologist had to perform the analysis of the CE totally blindly regarding the eventual diagnosis of HD. First, the radiologist had to determine the quality of the CE performance: positioning of the canula, filling of rectum and colon.
Second, he noted the presence or absence of RTZ on the lateral X-ray view in exoneration and defined it in vertebral level. Four groups of RTZ were arbitrarily determined with corresponding vertebral levels: rectal, rectosigmoid, long segment, and absence of RTZ. Radiological and anatomical correspondance are shown in Table 2.
These results were compared to the initial radiological reports; the results of which were recorded in three groups: rectosigmoid, long segment, and absence of RTZ. The rectal and rectosigmoid groups of the blind review were considered to belong to the same entity for a preliminate interobservator Kappa study between the initial radiological report and the single-blind secondary analysis.
Confidence interval of Kappa coefficient was estimated by bootstrap method. Acceptable values of Kappa for comparison of two groups are [7]:
0–0.20: very low agreement
0.21–0.40: low
0.41–0.60: moderate
0.61–0.80: full
0.81–1: almost perfect
Pathological analysis
The pathological report defining the total length of aganglionosis was considered as the gold standard. Pathological analysis was preformed in all cases on fresh surgical pieces. Four groups were also determined: rectal, rectosigmoid, long segment and total colonic HD. The superior limit for the rectal group was 7 cm for patients under the age of 2 years, 11.5 cm for patients above the age of 2 years, on the basis of anatomic data about the length of the rectum in children [7]. The superior limit for the rectosigmoid groups was 20 cm for all ages. Radiological and pathological correspondance are shown in Table 2.
Concordance study
The radio-pathological concordance between the four groups was studied by Kappa coefficient. Confidence interval of Kappa coefficient was estimated by bootstrap method. Absence of RTZ was considered as concordant for the cases of total colonic HD. Acceptable values of Kappa for comparison of two groups are [8]:
0–0.20: very low agreement
0.21–0.40: low
0.41–0.60: moderate
0.61–0.80: full
0.81–1: almost perfect
Examples of concordance are shown in Figs. 1 and 2.
Results
Radiological analysis
We first verified the validity of the contrast enema based on the results of single-blind review. The total number of contrast enemas was 81:61 patients with HD, 20 patients with no HD. We found a sensibility of 72.1 % and a specificity of 90 % in diagnosis of a RTZ in patients with HD (false negative = 17/81, false positive = 2/81).
The radiological technique was good in 81 % of the contrast enemas reviewed, intermediate in 16 %, of poor quality in 3 %.
Second, the single-blind review of the 61 contrast enemas was compared to the initial report with inter-observator Kappa study and concerned 3 groups: no RTZ, rectosigmoid RTZ, long-segment RTZ, as shown in Table 3.
We find 85.2 % of agreement with a Kappa value of 0.63 IC [0.38; 0.82], p value 9.8e−0 which corresponds to a full agreement between the initial report and the single-blind review. Any further analysis in this study will be based on the results of the single-blind review.
Pathological study
The repartition of pathological results in four groups was based on anatomical data about the length of the rectum in children according to their age: before 2 years, the rectum measures 7 cm maximum, and after 2 years minimum 11.5 cm.
The rectal group for neonates included the patients under the age of 2 with <7 cm of aganglionosis length (21 patients).
The rectal group for children included the patients older than 2 years old with <11.5 cm of aganglionis length (1 patient).
The rectosigmoid group included the patients between 7 and 20 cm of aganglionosis under the age of 2, and 11.5 and 20 cm after 2-year old (43 patients).
The long-segment group included the patients with more than 20 cm of aganglionosis (7 patients).
The total colonic HD group included 2 patients.
Concordance study
The results of the concordance study are shown in Table 4.
The CE showed no RTZ in 6/19 cases in RHD (31 %), in 8/34 cases in RSHD (23.5 %), in 0/6 cases in LSHD (0 %).
In the 2 cases of total colonic HD no RTZ was found; this result was considered as concordant.
It was concordant in 8/19 cases in RHD (42 %), in 20/34 in RSHD (58.8 %), in all 6 cases of LSHD (100 %).
If CE without RTZ is excluded, 61.5 % of the RHD, 77 % of RSHD, and 100 % LSHD were concordant, with a global percentage of agreement of 76.6 %.
Including CE without RTZ, we found 59 % of global agreement which corresponds to a Kappa value of 0.40 IC [0.24; 0.57], p value = 1.95e−08, equivalent of moderate agreement between pathological report and radiologic analysis.
Discussion
The correlation between CE findings in terms of localisation of the RTZ and the pathological results showed only moderate agreement in our study.
Our purpose was not to study the CE as a diagnosis test of HD as it would have been done in the past, but to try to precise the level of HD because of its surgical consequences: the choice of the corrective surgery, by transanal pull-through for RSHD or coelioscopic techniques for LSHD [5].
Critical analysis of methodology
Our radiological analysis showed sensibility (72.1 %) and specificity (90 %) rates concordant with the literature [3]. Despite the variety of radiologists performing the 61 CE available for review, 81 % was of good quality according to our senior radiologist performing the single-blind review.
Indeed, the localisation of the RTZ requires a lateral X-ray in exoneration, associated with a good positioning of the canula allowing satisfactory filling of the rectum, sigmoid and proximal colon.
Furthermore, the inter-observator study showed a Kappa value of 0.63 which corresponds to full agreement between the single-blind review and the different radiologists performing the initial analysis of CE. This satisfying result allowed us to base any further statistical analysis on the results of the single-blind review.
The choice of the radiologist to estimate the level of RTZ in vertebral level is based on the impossibility to measure the length of the digestive tube below the RTZ in centimeters, which would have been far too inaccurate for several reasons: different ages of the children, the absence of inferior limit (anal canal not filled because of the positionning of the canula), heterogeneity of the radiological techniques employed, with 19 % of intermediate and poor results.
However, this choice is not supported by other reports on the subject, which are scarce, but presents the advantages of taking into account the age of the child and of being easily reproducible.
The statistical challenge in this study was then to compare a quantitative variable: the exact length of aganglionosis on pathological report, and a qualitative variable: the vertebral level of the RTZ on radiological analysis.
This fact leads us to define four groups to perform a concordance study with Kappa coefficient: rectal group, rectosigmoid group, long-segment group and total colonic group. In literature, a Canadian study performed a concordance study with single-blind review of CE, but with only concordance percentages between radiological and pathological reports, and with no exact length of aganglionic bowel [4]. Another study performed a Kappa coefficient concordance test and found a Kappa value 0.0159, which corresponds to very low agreement, but with no single-blind review of the CE [9].
The vertebral RTZ repartition within the four groups was arbitrary, mostly difficult to establish for the inferior limit between rectal and rectosigmoid forms.
Since the rectosigmoid form is the most frequent form of HD, we attributed to that group the widest range of vertebra: from S2/S3 disk to L5.
We attributed then the lowest vertebra (S3 and S4) to the rectal forms, and the highest (L4/L5 disk and more) to the long-segment forms. No RTZ on CE was considered as concordant in the two cases of total colonic forms. Radiologic findings in this form of HD are known to be various and numerous [10], and these results in only two cases of total colonic form may not be considered as statistically significant.
The repartition of pathological results in four groups was based on anatomical data [7] about the length of the rectum in children according to their age. There too, the literature on the subject was scarce, and our repartition, based on only one reference in the literature, would require confirmation.
Critical analysis of results
The concordance study showed a global rate of agreement of 59 % (κ = 0.40), which corresponds to moderate agreement between radiologic and pathological findings.
This result was better than the spanish concordance study [9] probably due to the single-blind review and the definition of the exact length of aganglionosis.
Our results were slightly lower to those of the Canadian study, which found a global concordance rate of 88 % against 76.6 % in our study, when RTZ was present on CE.
This percentage was obviously lower when the statistics included the absence of RTZ on CE, which means that surgeons can more easily rely on radiologic results when RTZ is present on CE.
Our results were lower in RSHD (77 % of agreement) and better in LSHD (100 %) than in other studies [3, 4, 6], where the lack of accuracy of CE concerned especially LSHD. However, our study reported only six cases of LSHD which is too small to firmly conclude. The difference between RHD and RSHD showed lower rate of agreement in RHD: 42 % when CE without RTZ was included, 61.5 % when excluded. We can conclude that CE results do not allow accurate preoperative evaluation of short-segment HD.
All these results would lead us to advocate systematic preoperative biopsy, by ombilical incision when transanal pull-through is planned, or by coelioscopy for LSHD.
Colonic RMI may show better results in defining a radiological transition zone corresponding to aganglionosis. There are no data in literature about the evaluation of HD by RMI. This could be very informative and help to plan the corrective surgery. A prospective study could be realised to evaluate the accuracy of RMI in diagnosis of the level aganglionosis in HD.
Conclusion
Correlation between level of radiological transition zone on contrast enema and length of aganglionosis remains low, despite our efforts to improve characterization. Planning of surgery must be optimized with systematic preoperative biopsy by coelioscopy or ombilical incision depending on the chosen surgical technique.
References
Rahman N, Chouhan J, Gould S et al (2010) Rectal biopsy for Hirschsprung’s disease—are we performing too many? Eur J Pediatr Surg 20:95–97
Huang Y, Zheng S, Xiao X (2009) Preliminary evaluation of anorectal manometry in diagnosing Hirschsprung’s disease in neonates. Pediatr Surg Int 25:41–45
Jamieson DH, Dundas SE, Belushi SA et al (2004) Does the transition zone reliably delineate aganglionic bowel in Hirschsprung’s disease? Pediatr Radiol 34:811–815
Proctor ML, Traubici J, Langer JC et al (2003) Correlation between radiographic transition zone and level of aganglionosis in Hirschsprung’s disease: implications for surgical approach. J Pediatr Surg 38:775–778
Bonnard A, de Lagausie P, Leclair MD et al (2001) Definitive treatment of extended Hirschsprung’s disease or total colonic form. Surg Endosc 15:1301–1304
Rosenfield NS, Ablow RC, Markowitz RI et al (1984) Hirschsprung disease: accuracy of the barium enema examination. Radiology 150:393–400
Hobbs CJ, Hanks HGI, Wynne JM (1999) Child abuse and neglect: a clinician’s handbook, vol 682. Elsevier Health Sciences, Family & Relationships, New York
Seigel DG, Podgor MJ, Remaley NA (1992) Acceptable values of kappa for comparison of two groups. Am J Epidemiol 135:571–578
Granero Cendón R, Moya Jiménez MJ, Cabrera García R et al (2010) Relationship between the radiological length of the opaque enema and the aganglionic length of the segment in Hirschsprung’s disease. Cir Pediatr 23:53–56
Stranzinger E, DiPietro MA, Teitelbaum DH et al (2008) Imaging of total colonic Hirschsprung disease. Pediatr Radiol 38:1162–1170
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muller, C.O., Mignot, C., Belarbi, N. et al. Does the radiographic transition zone correlate with the level of aganglionosis on the specimen in Hirschsprung’s disease?. Pediatr Surg Int 28, 597–601 (2012). https://doi.org/10.1007/s00383-012-3094-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-012-3094-6