Abstract
The aim of this study was to evaluate role of anorectal manometry (ARM) and anal endosonography (ES) in assessment of the internal anal sphincter (IAS) quality on continence outcome following repair of anorectal anomalies (ARA). We devised a scoring system to evaluate the quality of the IAS based on ARM and ES and correlated the scores with clinical outcome, using a modified Wingfield score (MWS) for faecal continence. We also assessed the implication of megarectum and neuropathy on faecal continence. Of 54 children studied, 34 had high ARA and 20 had low ARA. Children with high ARA had poor sphincters on ES and ARM, and also poor faecal continence compared to those with low ARA. The presence of megarectum and neuropathy was associated with uniformly poor outcome irrespective of the IAS quality. The correlations between MWS on one hand, and ES and ARM scores for IAS on the other hand were weak in the whole study group, ES r = 0.27, P < 0.04, and ARM r = 0.39, P < 0.004. However, the correlations were strong in those who had isolated ARA without megarectum or neuropathy, ES r = 0.51, P < 0.02 and ARM r = 0.55, P < 0.01, respectively. In conclusion, the ARM and ES are valuable in evaluation of continence outcome in children after surgery for ARA and those with good quality IAS had better faecal continence. The IAS is a vital component in functional outcome in absence of neuropathy and megarectum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Our colorectal paediatric unit receives referrals for constipation and faecal incontinence for a wide variety of causes. As such, we have attempted to rationalise our management of children with anorectal anomalies (ARA). Several factors may contribute to the morbidity of ARA ranging from the severity of the anomaly to associated neuropathy and megarectum. Identification of specific causes of dysfunction should enable accurate evaluation of prognosis and effective management.
There are number of ways to assess dysfunction of the anorectum. We have used anorectal manometry (ARM) under ketamine anaesthesia and endoanal magnetic resonance imaging (EMRI) in children to investigate the causes of dysfunction, but neither is generally available [1, 2]. The EMRI in particular, has proven to be both costly and time consuming [3, 4]. The qualities of the internal anal sphincter (IAS) assessed by manometry and the presence of megarectum were found to be important determinants of outcome supporting the concept that the IAS is important factor affecting continence and that it is critical to preserve it at the time of reconstructive surgery [2, 5–7]. Our previously published study was limited by a complicated scoring system and having a small sample size making it impossible to assess the impact of neuropathy on outcome [2].
Scoring systems are necessary to render the observations suitable for statistical analysis and if adopted widely enable comparison between studies. However, EMRI scoring system did not perform well because it assessed the length and symmetry of the sphincter complex rather than its integrity in the transverse plane. Additionally, the scoring system was qualitative, making it difficult to compare results with other series.
Anal endosonography (ES) has been used to assess the anatomy of the pelvic floor and anal sphincters and it has been validated by electromyography, anorectal manometry and histological examination of the sphincters [3, 5, 8–12]. ES is easily performed and is of great value for recording sphincter defects in patients with anal fistulas and abscesses, muscular dystrophy, idiopathic faecal incontinence and ARA [8, 13–15]. The ES is a validated technique that can be applied with confidence to children with repaired ARA. The features on ES that have indicated disrupted sphincters, in women who have sustained injuries related to childbirth and in men who have undergone anal dilatation or surgery to the anal canal, have correlated strongly with anal dysfunction [16]. ES can only evaluate the anatomical integrity of the sphincters and does not distinguish between the smooth muscle of IAS and the circular muscle of rectum. However, ARM differentiates between the function of the IAS and the rectal muscle by rectoanal inhibitory reflex (RAIR) and it gives additional information about pressure profiles, size and compliance of rectum, anorectal sensation, and motor function of the external anal sphincter (EAS) muscle. As such the ARM is complementary to ES for investigation of faecal incontinence.
Neuropathy and megarectum are likely to impact adversely on the functional outcome even in the presence of a good sphincter [2, 17–20]. The indicators of neuropathy in the context of ARA are unclear, but we consider that neuropathy affecting the bladder is one of the best indicators because of similar embryological origin of hindgut and bladder [20, 21]. Morbidity related to neuropathy may be associated with the original ARA or acquired during reconstruction of anorectal and cloacal malformations [18, 19, 21]. Thus, urodynamic assessment may be necessary to detect bladder dysfunction in these patients. The presence of somatic neuropathy and sacral dysgenesis is likely to impact on the EAS function, which is also hypoplastic in this context. By inference, those children with neuropathic features can be expected to have impaired EAS function and altered levels of sensation but these features can only be evaluated in the awake and compliant child.
The aim of this study was to evaluate outcome of ARA for faecal continence by using a simple scoring system based on ARM and ES, which relates to function and integrity of the IAS following surgical repair. We also assessed the relative importance of neuropathy and megarectum on functional outcomes.
Patients and methods
We studied 62 consecutive children retrospectively who were referred from a number of centres for investigation and treatment of intractable constipation and faecal incontinence after repair of ARA between January 1991 and January 2005. As such, this is a clinical descriptive study of our practice. We excluded 8 children from the study, because of incomplete ARM or ES data and 54 are subject of this report. Patients had undergone various repairs of their ARA including posterior sagital anorectoplasty (PSARP) 24, abdominoperineal pull through 8, Stephens 2, Mollard 1, Durham Smith 3, anal transposition 7 and anoplasty 9. We did not attempt to compare the outcome of different surgical techniques because of difficulties to standardise various repairs done by different surgeons and the limited number of patients in this series.
We classified the patients broadly into two groups of ARA based on location of fistula at birth. Children without a perineal opening who required formation of a stoma as a neonate were labelled as high ARA and those with a perineal opening as low ARA. The low ARA group included anal stenosis and anterior ectopic anus 12, perineal fistula 8, and the high ARA group included rectovestibular fistula 12, rectovesical 2, cloacal malformation 1, rectoprostatic urethral fistula 19. We recognise that there is a problem with this classification, as patients with rectovestibular fistula who are in high ARA group, would have been classified in intermediate group according to the Wingspread classification because they carry a better prognosis [22]. We, therefore, included 12 girls with rectovestibular fistula in high ARA group and there was no boy with rectobulbar urethral fistula.
The ARM was done by a method based on a balloon system under ketamine anaesthesia and patient was lying in left lateral position as described previously [8]. We used the anorectal manometry analyser software, AMA version 3.11, developed by author (Keshtgar) [23]. ARM under ketamine anesthesia enables young and incompliant children to be studied without affecting activities of the IAS, but voluntary contraction of the external sphincter and sensation cannot be evaluated [24]. We had studied 144 children with chronic idiopathic constipation and reported a median resting anal sphincter pressure of 54 mmHg (range 19–107) on ARM [8]. We judged the resting anal sphincter pressure in excess of 30 mmHg as good and less than 30 mmHg as poor indicator of IAS function based on reports of lower limit of normal resting sphincter pressure in healthy children being 33 mmHg and also role of the IAS as the main contributor of resting anal pressure and faecal continence [25–29]. RAIR was defined as the smallest volume of rectal balloon distension required to produce an inhibitory relaxation of the IAS and fall of the anal resting pressure of at least 5 mmHg or more [30].
We used our scoring system based on function and integrity of the IAS on ARM and ES to evaluate the faecal continence outcome, which was reported recently [17]. The internal and external anal sphincters are anatomically and functionally discrete. The IAS is an involuntary smooth muscle that contributes to 50–85% of anal resting pressure and the EAS is a voluntary striated muscle, which contributes to 25–30% of the anal pressure tone [8–10, 25–29]. The ARM scoring system derived from resting sphincter pressure and rectoanal inhibitory reflex (RAIR) on a scale of 0–4, Table 1, Figs. 1a, 2a. The pressure profiles produced by our microballoons ARM system are comparable to the pressure profiles produced by water perfusion systems in children [7, 30, 31]. Essential features of manometry in children with ARA were compared to those with idiopathic constipation reported by us and healthy control children in the literature.
a Anorectal manometry trace of a 3.8-year-old girl done under ketamine anaesthesia after repair of low anorectal anomaly. Resting anal sphincter pressure (RP) was adequate, 38 mmHg, and minimum sphincter pressure (MSP) was 10 mmHg at complete reflex inhibition of the internal anal sphincter (IAS). Balloon inflation (Bal) in the rectum with increments of 10–25 ml of air resulted in rectoanal inhibitory reflex (RAIR) relaxation of the IAS. She was continent of stool and had constipation symptom. b Anal endosonography scan of patient in (a). The IAS was intact and appeared as a complete dark hypoechoic ring marked between the callipers. The external anal sphincter (EAS) appeared as mixed bright echogenic ring surrounding the IAS with a defect between 4 and 6 O’clock
a Anorectal manometry trace of a 9.5-year-old boy done under ketamine anaesthesia after repair of high anorectal anomaly. Resting anal sphincter pressure (RP) was 9 mmHg and rectoanal inhibitory reflex (RAIR) was absent at maximum rectal balloon (Bal) volume of 110 ml. The minimum sphincter pressure (MSP) was 6 mmHg at complete reflex inhibition of the internal anal sphincter (IAS). b Anal endosonography scan of patient in (a). The IAS is fragmented and scarred marked by crossed callipers. There is a defect extending through the IAS and the external anal sphincter (EAS) between 3 and 6 O’clock marked by diamond shaped callipers. The patient had an associated megarectum and was incontinent of faeces
We used Bruer and Krajer ultrasound system (B&K, Gentofte, Denmark) for ES with a 360° rotating 10 MHz transducer with patient lying in left lateral position as described previously [8]. On ES, the smooth muscle of the IAS was visualised as a dark homogenous hypoechoic ring surrounding the inner hyperechogenic ring of subepithelial tissue and the striated muscle of the EAS was seen as a bright ring of mixed echogenic pattern surrounding the IAS. The defects in anal sphincters appeared as breaks in the continuity of the muscle ring as amorphous areas of varying echogenicity. A defect in the IAS appeared as a hyperechogenic area and disruption of the EAS as a hypoechoic area. We did not attempt to score the EAS defects because of minimal contribution of the EAS in maintaining the resting anal pressure and continence and difficulty to distinguish its boundaries on ES [32]. The ES score assessed the presence of scarring and the integrity of the IAS in the transverse plane on a scale of 0–3, Table 2, Figs. 1b, 2b.
The presence of neuropathy was determined by sever neurosacral dysgenesis and abnormalities on magnetic resonance imaging of the back and symptoms of urinary incontinence associated with urodynamic findings of a neuropathic bladder including detrusor hyperreflexia and detrusor sphincter dyssynergia [18–21]. The presence of megarectum was determined by consistent evidence of distal evacuatory disorder refractory to treatment, or extreme megarectum on presentation by finding of a palpable or radiologically evident rectum extending to umbilicus or above [17]. The rectal volume and compliance was not always possible to assess on ARM because of absence of a RAIR due to deficient IAS in some children. Features of rectal physiology such as compliance and sensation are better evaluated by barometry, which is done by using a compliant low pressure balloon.
Clinical outcome with regard to faecal continence was assessed by using modified Wingfield score (MWS). The MWS included scores of 0 for normal function, 1 for constipation, 2 for intermittent soiling more than three episodes per week and 3 for continual soiling every day [2, 17]. This is a simple scoring system, which can be applied over a wide range of age including the young children. We defined constipation as difficult passage of hard stool with frequency of less than three per week and a palpable abdominal or rectal faecal impaction with or without soiling [32].
We used Spearman’s rho test for correlation analysis, chi square test for estimates of best fit and Mann–Whitney U test for non-parametrical analysis between the two groups of ARA. Results were expressed as median and range, and p value of less than 0.05 was considered significant.
Results
We studied 54 children with median age of 10 years (range 3.8–21.8). There were 34 children including 15 girls with high ARA; and 20 including 12 girls, with low ARA. A variety of techniques were used to perform reconstruction of the anomalies by a number of surgeons from differing centres. At presentation 11 children had symptoms of constipation, 9 in low ARA and 2 in high ARA groups and the remaining 43 patients were incontinent of stool. Clinical outcome was correlated to the grade of anomalies as those with high ARA had higher incidence of faecal incontinence and other malformations including megarectum and neuropathy, Table 3. The integrity of the IAS and its function were poorer in high than low ARA with respective median scores of 2 versus 0, P < 0.0001 on ARM and 2 versus 1, P < 0.006 on ES, Table 4. The median faecal continence score was also poorer in the high than low ARA group, 3 versus 2.5, respectively, P < 0.001. The median anal resting sphincter pressure in children with high ARA was 24 mmHg (range 9–45), which was lower compared to those with low ARA who had a resting sphincter pressure of 44 mmHg (31–72) and a better faecal continence (Figs. 1a, 2a). The resting sphincter pressure of children in low ARA group was comparable to the pressure of those with chronic IC, 54 mmHg (range 19–107) studied by us and to healthy children, 55 mmHg (SD ± 16), reported in the literature [8, 30, 31].
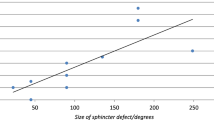
If all 54 children including those with associated megarectum and neuropathy are analysed together there is a weak but significant correlation between MWS for faecal continence and IAS scores by ES r = 0.27, P < 0.04, and ARM r = 0.39, P < 0.004. If 19 children who had isolated ARA and did not suffer the negative impact of megarectum and neuropathy are analysed separately the correlations of MWS for faecal continence are significantly better with ES score r = 0.52, P < 0.02 and ARM score r = 0.55, P < 0.01 and improves further with combination of ARM and ES scores, r = 0.7, P < 0.001. Of these 19 children, 9 had low anomalies (1 faecal incontinence) and 10 had high anomalies (8 faecal incontinence). The remaining 35 children were affected by megarectum and/or neuropathy and either of these features, alone or in combination, had a serious negative impact on faecal continence independent of sphincter quality, which was comparable to those with isolated ARA, Table 4. The MWS for faecal continence was significantly worse in the former group with respective scores of 3 versus 1, P < 0.0001.
If the MWS for faecal continence and the ES and ARM scores for IAS quality are classified into good or bad categories, there is a significant association between MWS and ES scores, P < 0.02; but not with ARM score which approaches significance, P < 0.07. The concordance between ES and ARM scores in these children is good in that there is agreement between both methods in 12 of the 19 children. The difference in 3 of the 7 children, where there is discordance but a good continence function, is accounted by the absence of a RAIR. This resulted in them scoring poorly on ARM although they had good resting sphincter pressure. If the resting sphincter pressure score on ARM is analysed in isolation and ignoring the RAIR score, the results of ARM and ES scores are identical in that there is a similar concordance between the scores from both techniques and MWS in 15 of 19 patients.
We excised the megarectum in 16 children in this series after failure of treatment with laxative or ACE wash out for intractable constipation and faecal incontinence, which were reported recently (17).
Discussion
This study included a population of children referred for assessment of their difficulties with faecal continence and constipation following repair of ARA. They may differ from an unselected group of such children in that they may represent those who are doing badly, particularly those with low ARA and those with associated megarectum and neuropathy. In this study, we found that ARM and ES findings of the IAS correlated with faecal continence in isolated ARA but the presence of megarectum and neuropathy was associated with uniformly poor functional outcome irrespective of the IAS quality. To the best of our knowledge this has not been reported previously.
The main purpose of ARM and ES is to identify the specific features of anorectal dysfunction and morphological abnormalities that are responsible for constipation and faecal incontinence. In normal subjects, faecal continence is achieved by an adequate anal sphincter pressure, a compliant low pressure rectum and an effective colorectal peristalsis along with intact sensory and motor neurological functions. However, in children born with ARA these arbiters of faecal continence may be impaired because of deficient IAS, hypoplastic EAS muscle complex, poor motility of associated megarectum and neuropathy caused by impaired congenital or acquired sensory/motor neurological functions [2, 17–19, 21, 34, 35].
Embryological and histological studies in animal models and humans have indicated that the IAS is present in ARA at the site of fistula, hence the term ectopic anus designated to the fistulae in anorectal malformations [36, 37]. Other investigators have also reported presence of IAS at the site of fistulae and highlighted the functional importance of this structure, which is sometimes not preserved during surgical repair of ARA [38–42]. Furthermore, clinical studies following repair of ARA have shown better faecal continence in children who had sphincter saving repair [22, 42]. However, there is lack of information in the literature about detailed investigations related to the morphology and function of anal sphincters and its relation with clinical outcome.
In this series, results of ARM and ES investigations indicate that integrity of the IAS is vital for a good functional outcome and faecal continence following repair of ARA. In particular, an adequate resting sphincter pressure is necessary, which is largely dependent on the integrity of the IAS. We consider an adequate function of IAS on ARM by combination of a resting sphincter pressure of 30 mmHg or more; and a RAIR with fall of the resting pressure of at least 5 mmHg [8, 17, 30]. RAIR indicates normal relaxation of the IAS in response to rectal distension. An absence of RAIR may indicate deficiency or scaring of the IAS despite a recordable resting pressure or it may represent aganglionosis as we observed in one patient who had Hirschsprung disease.
We found that quality of the IAS and faecal continence was better in children with low ARA who had a higher resting sphincter pressure of 44 mmHg, which was comparable to those with chronic idiopathic constipation and healthy children [8, 30, 31]. RAIR was seen in 80% of children with low ARA and 18% of those with high ARA, which is in keeping with findings of other investigators [40]. There was an association between presence of a good quality IAS on ARM and ES, and achieving a faecal continence in those with isolated ARA. However, presence of megarectum and/or neuropathy in children with ARA outweighed the benefit of good IAS as they were incontinent of faeces despite having an IAS quality comparable to those with isolated ARA. This is not surprising in that either may result in constipation and faecal incontinence outside the context of ARA [8, 43–45]. The combination of the relatively narrow and incompliant sphincter, which often results from repair of ARA and presence of megarectum and neuropathy, are particularly unfavourable. We hypothesis that faecal incontinence in children with megarectum and neuropathy is explained by poor compliance and activity of the rectum and also high ratio of rectal/sphincter pressure based on our observations in children with Hirschsprung disease [45]. We have recently reported our experience with excision of megarectum in 16 children with ARA and faecal incontinence who are included in this series [17]. Excision of megarectum in these children resulted in faecal continence in presence of a good IAS and absence of neuropathy. However, those who either had poor IAS or neuropathy often required artificial means of faecal continence like formation of an ACE stoma. This indicates the importance of preserving the IAS at the time of repair of ARA and highlights the prognostic value of ARM and ES with regard to outcome and achieving faecal continence.
In children who have ARA and neuropathy, faecal incontinence is caused by low resting anal sphincter pressure and impaired motor and sensory neurological function of rectum. The detrimental effect of neuropathy on bowel and bladder function has been investigated by ARM and urodynamic studies in children with spinal cord lesions who have morphologically intact anal sphincters [33, 46, 47]. Agnarsson and others reported a reduced mean anal resting sphincter pressure, a short functional anal canal, impaired sensory/motor activities of the rectum and abnormal RAIR in neuropathic children with myelomeningocele compared to age-matched controls [46, 47]. This is analogous to children born with ARA who have sacral dysgenesis and neuropathy, whose motor and sensory neurological impairment predominantly affect the pelvic floor and EAS muscles and contribute to faecal incontinence [46, 48]. Our study is limited by the fact that ARM has been carried out in most children under ketamine anaesthesia, which does not affect the IAS function, but it does not enable the EAS function and sensation to be assessed meaningfully. Emblem et al. have reported the role of ES and anatomical integrity of anal sphincters for achieving faecal continence after repair of ARA [15]. Indeed their scoring systems should be reproducible and suitable for the overall evaluation of the anatomical qualities of anorectal reconstructions. In accordance with our results there was a positive correlation between the IAS defects, diminished resting sphincter pressure and faecal incontinence. However, we stress the importance of IAS for faecal continence because in normal individuals it accounts for up to 85% of the resting anal sphincter pressure and the EAS contributes to less than 30% of the pressure, which is hypoplastic in the context of ARA [25–29]. The EAS along with pelvic floor muscles contribute to maintaining the urge faecal continence. ES may not reliably show the defects of EAS, which may be better defined by MRI and CT scan [1, 33, 49]. Our results indicate the necessity to preserve the IAS at operations for anorectal and cloacal anomalies, which has been recommended by some authors but it is still not generally heeded [37–40, 42]. In respect of this, there may be a role for laparoscopic assisted pull through reconstruction of high ARA through a minimal perineal dissection because it avoids division of anal sphincter muscle complex [50]. Laparoscopic approach preserves the distal rectum and IAS, which is placed accurately within the sphincter complex, and it reduces the risk of pelvic nerve injury through superior visualisation [50, 51]. However, the long-term results for faecal continence are not available at present.
The main purpose of our study was to recognise the causes of bowel dysfunction and where possible to correct them. Our results indicate that ARM and ES are instrumental to evaluate the morphology and function of IAS and the findings correlate well with outcome of faecal continence. The function of IAS in maintaining the resting sphincter pressure and faecal continence is the major determinant of outcome in children born with ARA, who do not have neuropathy and megarectum. Our study will form the basis for the construction of a clinical care pathway with guided management of the causes of dysfunction in infancy and preschool years so that the appropriate measures can be implemented at early stage. Knowledge gained should be used to feed back the techniques adopted in anorectal reconstruction at the outset with particular attention for preserving the IAS wherever possible and avoiding iatrogenic neuropathy at the time of anorectoplasty in order to improve the prospect of gaining faecal continence. But perhaps the final status of the patient can only be assessed in adulthood, when a full appraisal of social, sexual, bowel and bladder function can be made.
References
de Souza NM, Ward HC, Williams AD, Battin M, Harris DN, McIver DK (1999) Transanal MR imaging after repair of anorectal anomalies in children: appearances in pull-through versus posterior sagital reconstructions. Am J Roentgenol 173:723–728
Hettiarachchi M, Garcea G, de Souza NM, Williams AD, Clayden GS, Ward HC (2002) Evaluation of dysfunction following reconstruction of an anorectal anomaly. Pediatr Surg Int 18:405–409
Schafer A, Enck P, Furst G, Kahn T, Frieling T, Lubke HJ (1994) Anatomy of the anal sphincters. Comparison of anal endosonography to magnetic resonance imaging. Dis Colon Rectum 37:777–781
Briel JW, Stoker J, Rociu E, Lameris JS, Hop WCJ, Schouten WR (1999) External sphincter atrophy on endoanal magnetic resonance imaging adversely affects continence after sphincteroplasty. Br J Surg 86:1322–1327
Fukata R, Iwai N, Yanagihara J, Iwata G, Kubota Y (1997) A comparison of anal endosonography with electromyography and manometry in high and intermediate anorectal anomalies. J Pediatr Surg 32:839–842
Lambrecht W, Lierse W (1987) The internal sphincter in anorectal malformations: morphologic investigation in neonatal pigs. J Pediatr Surg 12:1160–1168
Emblem R, Diseth T, Mørkrid L (1997) Anorectal anomalies: anorectal manometric function and endosonography in relation to functional outcome. Pediatr Surg Int 29:447–451
Keshtgar AS, Ward HC, Clayden GS, Sanei A (2004) Thickening of the internal anal sphincter in idiopathic constipation in children. Pediatr Surg Int 20:817–823
Law PJ, Kamm MA, Bartram CI (1990) A comparison between electromyography and anal endosonography in mapping external anal sphincter defects. Dis Colon Rectum 33:370–373
Sultan AH, Kamm MA, Talbot IC, Nicholls RJ, Bartram CI (1994) Anal endosonography for identifying external sphincter defects confirmed histologically. Br J Surg 81(3):463–465
Keshtgar AS, Ward HC, Clayden GS, Sanei A (2005) Role of anal dilatation in treatment of idiopathic constipation in children: long-term follow-up of a double blind randomized controlled study. Pediatr Surg Int 21:100–105
Keshtgar AS, Ward HC, Sanei A, Clayden GS (2007) Botulinum toxin, a new treatment modality for chronic idiopathic constipation in children: long-term follow up of a double blind randomized trial. J Pediatr Surg 42(4):672–680
Law PJ, Talbot RW, Bartram CI, Northover JM (1989) Anal endosonography in the evaluation of perianal sepsis and fistula in ano. Br J Surg 76:752–755
Eckardt VF, Nix W (1991) The anal sphincter in patients with myotonic muscular dystrophy. Gastroenterology 100:424–430
Emblem R, Mørkrid L, Bjørnland K (2007) Anal endosonography is useful for postoperative assessment of anorectal malformations. J Pediatr Surg 42(9):1549–1554
Lunniss PJ, Gladman MA, Hetzer FH, Williams NS, Scott SM (2004) Risk factors in acquired faecal incontinence. J R Soc Med 97:111–116
Keshtgar AS, Ward HC, Richards C, Clayden GS (2007) Outcome of excision of megarectum in children with anorectal malformation. J Pediatr Surg 42:227–233
Levitt MA, Patel M, Rodriguez G, Gaylin DS, Penã A (1997) The tethered cord in patients with anorectal malformations. J Pediatr Surg 32:462–468
Warne SA, Godley ML, Wilcox DT (2004) Surgical reconstruction of cloacal malformation can alter bladder function: A comparative study with anorectal anomalies. J Urol 172:2377–2381
Keshtgar AS, Rickwood AM (1998) Urological consequences of incomplete cord lesions in patients with myelomeningocele. Br J Urol 82(2):258–260
Boemers TML, Beek FJA, van Gool JD, de Jong TPVM, Bax KMA (1996) Urologic problems in anorectal malformations. Part 1: urodynamic findings and significance of sacral anomalies. J Pediatr Surg 31:407–410
Stephens FD, Smith ED (1986) Classification, identification and assessment of surgical treatment of anorectal anomalies. Pediatr Surg Int 1:200–205
Keshtgar AS, Sanei A, Ward H C. Manometry data analyser for Windows in clinical practice. Presented in the 15th International Research Symposium in Paediatric Surgery, Marseille, 3–4 October 2003
Paskins JR, Lawson JON, Clayden GS (1984) The effect of ketamine anesthesia on anorectal manometry. J Pediatr Surg 19:289–291
Lesta B, Penninckx F, Kerremans R (1989) The composition of anal basal pressure. An in vivo and in vitro study in man. Int J Colorectal Dis 4:118–122
Schweiger M (1979) Method for determining individual contributions of voluntary and involuntary anal sphincters to resting tone. Dis Colon Rectum 22:415–416
Frenckner B, Euler CH (1975) Influence of pudendal block on the function of the anal sphincters. Gut 16:482–489
Duthie HI, Watts JM (1965) Contribution of the external anal sphincter to the pressure zone in the anal canal. Gut 6:64–68
Gibbons CP, Trowbridge EA, Bannister JJ, Read NW (1986) Role of anal cushions in maintaining continence. Lancet 1:886–887
Benninga MA, Wijers OB, Van der Hoeven CW (1994) Profilometry and endosonography: normal physiology and anatomy of the anal canal in healthy children. J Pediatr Gastroenterol Nutr 18:68–77
Loening-Baucke VA (1984) Abnormal rectoanal function in children recovered from chronic constipation and encopresis. Gastroenterology; 87(6):1299–1304
Loening-Baucke V, Yamada T (1995) Is the afferent pathway from the rectum impaired in children with chronic constipation and encopresis. Gastroenterology 109:397–403
West RL, Dwarkasing S, Briel JW, Hansen BE, Hussain SM, Schouten WR, Kuipers EJ (2005) Can three-dimensional endoanal ultrasonography detect external anal sphincter atrophy? A comparison with endoanal magnetic resonance imaging. Int J Colorectal Dis 20(4):328–333 Epub 20 Aug 2004
Boemers TML, Bax KMA, Rövekamp MH, van Gool JD (1995) The effect of posterior sagital anorectoplasty and its variants on lower urinary tract function in children with anorectal malformations. J Urol 153(1):191–193
Penã A (1995) Anorectal malformations. Semin Pediatr Surg 4:35–47
Bill AH, Johnson RJ (1958) Failure of migration of the rectal opening as a cause for most cases of imperforate anus. Surg Gynecol Obstet 106:643–648
Gans SL, Friedman NB (1961) Some new concepts in the embryology, anatomy, physiology and surgical correction of imperforate anus. West J Surg Obstet Gynecol 69:34–37
Frenckner B (1985) Use of the recto-urethral fistula for reconstruction of the anal canal in high anal atresia. Z Zinderchir 40:312–314
Penninckx FMA, Kerremans RPJ (1986) Internal sphincter saving in imperforate anus with or without fistula. Int J Colorect Dis 1:28–32
Ito Y, Yokoyama J, Hayashi A, Ihara N, Katsumata K (1981) Reappraisal of anorectal pull-through procedure I Anorectal malformations. J Pediatr Surg 16(4):476–483
Hedlund H, Penã A (1990) Does the distal rectal muscle in anorectal malformations have the functional properties of a sphincter? J Pediatr Surg 25:985–989
Rintala RJ, Lindahl H (1995) Is normal bowel function possible after repair of intermediate and high anorectal malformations? J Pediatr Surg 30:491–494
van der Plas RN, Benninga MA, Staalman CR, Ackkermans LMA, Redekop WK et al (2000) Megarectum in constipation. Arch Dis Child 83:52–58
Callaghan RP, Nixon HH (1964) Megarectum: physiological observations. Arch Dis Child 39:153–157
Keshtgar AS, Ward HC, Clayden GS, de Sousa NM (2003) Investigations for incontinence and constipation after surgery for Hirschsprung’s disease in children. Pediatr Surg Int 19(1–2):4–8
Agnarsson U, Warde C, McCarthy G, Clayden GS, Evans N (1993) Anorectal function of children with neurological problems. I: Spina bifida. Dev Med Child Neurol. 35(10):893–902
Marte A, Cotrufo AM, Di Iorio G, De Pasquale M (2001) Electromyographic and manometric anorectal evaluation in children affected by neuropathic bladder secondary to myelomeningocele. Minerva Pediatr 53(3):171–176
Ikeda T, Tomita R, Koshinaga T (2005) Anal mucosal electric sensation in postoperative patients with anorectal malformations. J Pediatr Surg 40(7):1146–1150
Ikawa H, Yokoyama J, Sanbonmatsu T, Hagane K, Endo M, Katsumata K, Kohda E (1985) The use of computerized tomography to evaluate anorectal anomalies. J Pediatr Surg 20:640–644
Georgeson KE, Inge TH, Albanese CT (2000) Laparoscopically assisted anorectal pull-through for high imperforate anus—a new technique. J Pediatr Surg 35(6):927–930
Wong KK, Khong PL, Lin SC, Lam WW, Lan LC, Tam PK (2005) Post-operative magnetic resonance evaluation of children after laparoscopic anorectoplasty for imperforate anus. Int J Colorectal Dis 20(1):33–37 Epub 20 Aug 2004
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keshtgar, A.S., Athanasakos, E., Clayden, G.S. et al. Evaluation of outcome of anorectal anomaly in childhood: the role of anorectal manometry and endosonography. Pediatr Surg Int 24, 885–892 (2008). https://doi.org/10.1007/s00383-008-2181-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-008-2181-1