Abstract
It is controversial as to whether osteotomy, by restoring a more normal pelvic anatomy, might improve the final outcome of bladder exstrophy (BE) repairs. We compared the functional orthopaedic and urological outcomes in BE patients treated with and without osteotomy. Orthopaedic and urological outcomes were compared in eight BE patients treated with osteotomy and six BE patients treated without osteotomy. Orthopaedic evaluation included an assessment of pubic bones dissymmetry, bending of the spine, presence of Trendelenburg or Thomas sign, and presence of out-toeing. Pubic diastasis was ruled out on a plain X-ray of the pelvis. A Pediatric Orthopedic Society of North America (POSNA) questionnaire was administered to every child or his/her caregiver to assess functional outcome. Urological evaluation included an assessment of required continence surgeries and of contemporary continence status. All patients presented a pubic diastasis. This was in median 49 (24–66) mm in patients treated without osteotomy and 42 (25–101) mm in those treated with osteotomy (p = 0.3). There was no difference either in the orthopaedic outcome or in any features of the POSNA questionnaire between groups. Neither was there a difference in the final continence rate nor in the number of additional continence procedures required. Although osteotomy is an essential step in the treatment of many BE patients in order to achieve a tension-free closure of the abdominal wall and bladder, our preliminary results suggest that it does not improve the eventual orthopaedic or urological outcomes of BE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bladder exstrophy (BE) is a rare condition which occurs in 1 every 30,000 live births and 2 times more commonly in males than females.
Ideal management of the condition is still controversial. Particularly in males, some advocate a single stage repair in the neonatal period [1], whereas others prefer to limit neonatal surgery to bladder closure, deferring the epispadias repair to a later age, at some point between 6 months and 2 years [2].
Controversy also exists as to whether bladder closure should be combined with an osteotomy. The latter is usually considered obligatory if surgery is delayed until after 72 h of life or in case of re-operative closures, but some consider osteotomy beneficial also in primary procedures as it might improve the orthopaedic and urological outcomes. About the latter, osteotomy would allow for a reconfiguration of the pelvic floor muscles [3–5] and a dipper and more anatomically normal positioning of bladder, bladder-neck, and posterior urethra within the pelvis [6], thus enhancing the chances to eventually achieve urinary continence. Nevertheless, osteotomy is also a difficult undertaking, which exposes the patients to increased intra-operative blood loss, a longer post-operative course, and additional morbidity.
This study aimed to evaluate the difference in the orthopaedic and urological functional outcomes, also using a standardized questionnaire, in a selected group of patients undergoing BE repair either with or without osteotomy.
Materials and methods
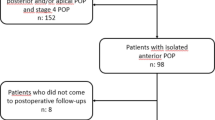
Between 2005 and 2006, 14 consecutive BE patients treated under the care of a single experienced paediatric urologist were enrolled in this study. Patients were divided into two groups, a group of eight cases that had undergone BE repair with osteotomy (osteotomy group), was compare with six cases managed without osteotomy (no osteotomy group). Osteotomy is not routinely included in the primary repair of BE at our centre, hence of the eight patients in the osteotomy group, five had had their osteotomy performed elsewhere before referral, while in the remaining three the osteotomy had been done at our institution after failure of primary closure (n = 2) or for delayed referral beyond 72 h of life (n = 1). Osteotomy had been performed soon after birth, simultaneously to primary bladder closure in five patients, whereas 2 months (n = 1) and 1 year (n = 2) after failure of an attempt to primary closure in the remainders. The type of osteotomy was ischio-pubic [7] in two, posterior vertical iliac [8] in three, and anterior and horizontal [9] in the remaining three treated at our institution.
For the purposes of this study, an orthopaedist and an urologist assessed the patients. Orthopaedic evaluation included an assessment of pubic bones dissymmetry, bending of the spine, presence of Trendelenburg or Thomas sign, and presence of out-toeing. Pubic diastasis was ruled out on a plain X-ray of the pelvis. A Pediatric Orthopedic Society of North America (POSNA) questionnaire was administered to every child or his/her caregiver. This questionnaire is designed to assess the real-life functional levels of patients aged 2–18 years, and includes four functional scores (upper extremity function, transfers and basic mobility, sports and physical function, comfort/pain) and a global function score. All scores can range between 0, the lowest score, and 100, the highest score. The questionnaire was validated on both patients with moderate to severe orthopaedic diagnoses and normal children, and can be administered to either patients or their caregivers with a good correlation in the scores between the two [10, 11].
Urological evaluation included a chart review to assess previous continence surgery (bladder-neck reconstruction, bladder augmentation, creation of a Mitrofanoff catheterizable conduit), and an evaluation of the contemporary continence status. Continence was defines as a dry interval longer than 2 h, with or without clean intermittent catheterization (CIC).
Results were expressed as median and range, but for the POSNA scores expressed as mean ± 2 standard deviations. Mann–Whitney U test was used to compare non-paired continuous values, T test was used to compare POSNA scores, and a Fisher’s exact test for categorical variables. A p value of ≤0.05 was considered significant.
Results
Median age at evaluation was 9.7 (3.1–17.8) years without difference between groups, 11.1 (5–17.8) versus 9.8 (3.1–14.9) years. The two groups were also sex-matched.
On the follow up plain X-ray of the pelvis, all patients presented a pubic diastasis. This was in median 49 (24–66) mm in patients treated without osteotomy and 42 (25–101) mm in those treated with osteotomy (p = 0.3).
Results of the orthopaedic evaluation are listed in Table 1. In the four patients presenting dissymmetry of the pubic bones, this was 1–1.5 cm.
Spine bending, present in four osteotomy patients, was always mild and did not require treatment.
Figure 1 depicts the results of the POSNA questionnaire. None of the features proved to be different between groups.
In terms of urinary continence, results between groups were not essentially different as shown in Table 2.
Discussion
Our preliminary results, in a small group of patients, suggest that osteotomy does not improve the eventual outcome, either urological or orthopaedic, in BE repairs.
Studies on the anatomy of the bony pelvis and the pelvic floor musculature in BE patients have shown that the pelvic ring is open and flat in these patients [12] and thereby the pelvic floor muscles, attached to the pubic rami, are laterally displaced instead being wrapped around the midline structures of the bladder, urethra, vagina, and rectum [3]. Furthermore, cases with greater continent intervals after surgery have anatomic parameters more similar to those of age-matched controls than incontinent cases [13]. It is controversial as to whether osteotomy might contribute to restore a more normal anatomy thus improving the orthopaedic outcome and enhancing the chances for eventual urinary continence [6, 12]. In fact no study has so far compared the pelvic floor anatomy in cases treated with and without osteotomy.
We compared the urological and orthopaedic outcomes in BE patients treated either with or without osteotomy a median time of almost 10 years after initial repair. The two groups were sex- and age-matched.
The first important finding was the presence of similar pelvic diastasis in both groups. The recurrence of diastasis after osteotomy is consistent with several previous reports [14–16]. Sponseller et al. [15] suggested two possible mechanisms accounting for it, either a partial derotation of the pelvis before the osteotomy site heals or the long-term undergrowth of the ischiopubic segment. Unfortunately, most of our osteotomy patients were secondary referrals, and therefore we could not define the cause of recurrence, which can be related to many factors [17]. Anyway, the similar diastasis between groups suggests that this is not a critical factor for the final outcome as it is also suggested by the three-dimensional magnetic resonance imaging study by Williams et al. [5].
Overall, the orthopaedic outcome did not present any difference of clinical relevance between the two groups in any respect. Spine bending was present only in patients treated with osteotomy, and this approached statistically significance, but was always mild and did not require any treatment. An association between scoliosis and BE is known [18]. Most of the patients, instead, presented an out-toeing irrespective of osteotomy. This was probably related to the similar pubic diastasis in both groups.
We administered a standardized questionnaire to assess self-appreciation of the orthopaedic functional outcome, which should be the true ultimate goal of any treatments [10, 11]. To our knowledge, this is the first time such a questionnaire to be used in BE patients. Again, even with this tool we could not find any difference between groups. Furthermore, the scores of BE patients compared favourably with those reported in normal children [11], suggesting, in keeping with previous studies [19], that the many orthopaedic abnormalities present in BE patients are seldom of clinical relevance, cause symptoms or require treatment.
We did not find any significant difference also in the urological outcome of our patients either in terms of number of additional continence surgeries required, or in the final continence rate with or without CIC. These findings are consistent with other data from the literature, which suggest that the major determinant of outcome in terms of continence in BE patients is the timing of bladder closure. The possibility to achieve urinary continence eventually is multifactorial but is critically related to bladder capacity, and the sooner normal bladder cycling is restored, the higher the chance for the bladder to grow [20]. In this respect, our groups were quite homogeneous as all the patients in the no osteotomy group and five out of eight in the osteotomy group were successful primary closures.
Major limitations of the current study are as follows: firstly, the small number of patients causes a significant risk of type II error. Given the rarity of the condition, however, only a multicentric study could probably allow for the collection of a significant number of cases. Secondly, since patients’ data were partially collected retrospectively and some patients were initially treated elsewhere, some data were missed such as the degree of pelvic diastasis before surgery, which is a potentially important prognostic factor [6]. Finally, a variety of osteotomy techniques were used in group B, with an expected variable impact on the pelvic functional anatomy. For instance, two patients underwent an ischio-pubic ramotomy [7], which only allows for an apposition of the rectus muscles over the bladder without a true reconfiguration of the pelvic ring. In this respect, our preferred osteotomy technique is the anterior horizontal pelvic osteotomy [8], which was adopted in all the three cases that underwent osteotomy at our institution. It can be performed through an anterior approach and does not affect the pelvic diameters and hence the final pelvic capacity. Gearhart et al. [21], however, proposed a combined vertical and horizontal pelvic osteotomy as the technique capable to restore the most normal anatomy.
The major strengths of the current study, instead, are that it is, to our knowledge, the first case control study on this controversial issue and the first adopting a standardized questionnaire to assess the orthopaedic functional outcome. Therefore, although we accept that our results are still very preliminary and require confirmation, in our opinion they offer insights of potential clinical relevance into the controversy concerning the role of osteotomy in BE treatment.
Finally, it is also our opinion that the absence of any difference between our groups does not mean that osteotomy has no role at all in the management of BE. It is indeed essential in re-operative closures after previous failures or in case of delayed closures due to either delayed presentation or inadequate bladder template [6, 17]. Although Kajbafzadeh et al. [22] proposed a modified technique to achieve a secure closure even in these scenarios without osteotomy, the latter remains the best established method to obtain a tension-free closure of abdominal wall and bladder. Baird et al. [6] suggested additional scenarios in which a judicious use of osteotomy might be appropriate such as in newborn patients with a diastasis >4 cm or in those with a non-malleable pelvis (i.e., a pelvis that does not allow easy apposition of the pubic bones under anaesthesia). In very selected cases osteotomy might even be considered to facilitate bladder-neck reconstruction [6].
In primary neonatal bladder closures, instead, the pelvis is generally malleable enough to allow successful closure of the abdominal wall, whereas a deep positioning of urethra, bladder-neck, and bladder can be achieved irrespective of osteotomy by sectioning the inter-symphyseal band and deepening the urethra in the anterior perineal diaphragm. The latter is indeed an essential step in many reconstructive procedures described for BE repair both in males and females [1, 20, 23], and may be further combined with a soft-tissues reconstruction to improve continence [24, 25].
In conclusion, although osteotomy is an essential step in the treatment of many BE patients, our preliminary results suggest that it does not improve the long-term orthopaedic or urological outcomes after BE repair. The criteria used in this study represent an easy and rational approach to address this controversial issue, but will need to be tested on a wider number of patients perhaps in a multicentric study.
References
Mitchell ME (2005) Bladder exstrophy repair: complete primary repair of exstrophy. Urology 65:5–8
Baird AD, Nelson CP, Gearhart JO (2006) Modern staged repair of bladder exstrophy: a contemporary series. J Pediatr Urol. doi: 10.1016/j.jpurol.2006.09.009
Stec AA, Pannu HK, Tadros YE et al (2001) Pelvic floor anatomy in classical bladder exstrophy using 3-dimensional computerized tomography: initial insights. J Urol 166:1444–1449
Halachmi S, Farhat W, Konen O et al (2003) Pelvic floor magnetic resonance after neonatal stage reconstruction in male patients with classic bladder exstrophy. J Urol 170:1505–1509
Williams AM, Solaiyappan M, Pannu HK et al (2004) 3-dimensional magnetic resonance imaging modelling of the pelvic floor musculature in classic bladder exstrophy before pelvic osteotomy. J Urol 172:1702–1705
Baird AD, Sponseller PD, Gearhart JO (2005) The place of pelvic osteotomy in the modern era of bladder exstrophy reconstruction. J Pediatr Urol 1:31–36
Frey P (1994) Bilateral anterior pubic osteotomy in bladder exstrophy closure. J Urol 151:812–815
Shultz WG (1958) Plastic repair of bladder combined with bilateral osteotomy of ilia. J Urol 79:453–458
Gibbon AJ, Maffulli N, Fixsen JA (1991) Horizontal pelvic osteotomies for bladder exstrophy. A preliminary report. J Bone Joint Surg 73:896–898
Lawren D, Matthew LH, Anne F et al (1998) The POSNA pediatric musculoskeletal functional health questionnaire: report on reliability, validity, and sensitivity to change. J Pediatr Orthop 18:561–571
Haynes RJ, Sullivan E (2001) The pediatric orthopaedic society of North America Pediatric Orthopaedic functional health questionnaire: an analysis of normals. J Pediatr Orthop 21:619–621
Stec AA, Pannu HK, Tadros YE et al (2001) Evaluation of the bonny pelvis in classic bladder exstrophy by using 3-D-CT: further insights. Urology 58:1030
Gargallo PC, Borer JG, etik AB et al (2005) Magnetic resonance imaging of pelvic musculoskeletal and genitourinary anatomy in patients before and after complete primary repair of bladder exstrophy. J Urol 174:1559–1566
Kantor R, Salai M, Ganel A (1997) Orthopaedic long term aspects of bladder exstrophy. Clin Orthop 335:240–245
Sponseller PD, Jani MM, Jeffs RD et al (2001) Anterior innominate osteotomy in repair of bladder exstrophy. J Bone Joint Surg Am 83A:184–193
Kaar SG, Cooperman DR, Blakemore LC et al (2002) Association of bladder exstrophy with congenital pathology of the hip and lumbosacral spine: a long-term follow-up study of 13 patients. J Pediatr Orthop 22:62–66
Meldrum KK, Baird AD, Gearhart JO (2003) Pelvic and extremity immobilization following bladder exstrophy closure: complications and impact on success. Urology 62:1109–1103
Loder R, Dayioglu M (1990) Association of congenital vertebral malformations with bladder and cloacal exstrophy. J Pediatr Orthop 10:389–393
Raabe I, Gobet R, Kellemberg C et al (2007) Is bladder exstrophy a risk factor for hip arthrosis? J Pediatr Urol 3:S16–5
Oesterling JE, Jeffs RD (1987) the importance of a successful initial bladder closure in the surgical management of classical bladder exstrophy: analysis of 144 patients treated at the Johns Hopkins Hospital between 1975 and 1985. J Urol 137:258–262
Gearhart JO, Forschner DC, Jeffs RD et al (1996) A combined vertical and horizontal pelvic osteotomy approach for primary and secondary repair of bladder exstrophy. J Urol 155:689–693
Kajbafzadeh AM, Tajik P (2006) A novel technique for approximation of the symphysis pubis in bladder exstrophy without pelvic osteotomy. J Urol 175:692–698
Kropp BP, Cheng EY (2000) Total urogenital complex mobilization in female patients with exstrophy. J Urol 164:1035–1039
Caione P, Capozza N, Lais A et al (2000) Periurethral muscle complex reassembly for exstrophye epispadias repair. J Urol 164:2062–2066
Desai D, Ryan K, Johal N et al (2007) Long term results of the Kelly soft tissue reconstruction for continence in classic bladder exstrophy. J Pediatr Urol 3:S820
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Castagnetti, M., Gigante, C., Perrone, G. et al. Comparison of musculoskeletal and urological functional outcomes in patients with bladder exstrophy undergoing repair with and without osteotomy. Pediatr Surg Int 24, 689–693 (2008). https://doi.org/10.1007/s00383-008-2132-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-008-2132-x