Abstract
The purpose of the present study was to determine whether a correlation exits between the main trauma scoring systems and the activation of inflammatory cells and mediators such as interleukin-(IL-) 1β, IL-6, IL-8 and tumor necrosis factor alpha (TNF-α) after trauma, and moreover to assess if any of these can be used to predict the outcome in patients under care at a trauma center. Forty-seven children (37 boys, 10 girls) presenting with blunt trauma, were evaluated by an analysis of the relationship between overall mortality and potential risk factors. Admission data, including serum IL-1β, IL-6, IL-8, TNF-α, pediatric trauma score (PTS), and injury severity score (ISS), were collected and analyzed. In descriptive statistics for independent variables, some prognostic factors such as IL-8 (P = 0.04), and ISS (P = 0.004) were significant in their relationship to mortality. In the univariate statistical analysis some other risk factors such as IL-8 (P = 0.004), >20 TNF-α (P = 0.04), and ISS (P = 0.007) were significant in their relationship to mortality. The relative risk of developing mortality was higher than two for each of the following risk factors: >10 ages, >25 IL-6, 10–20 TNF-α, >20 TNF-α, PTS ≤ 8, and ISS > 15. There was a positive correlation between IL-8 (r = 0.31, P = 0.33), ISS (r = 0.31, P = 0.0001), and mortality. There was also a correlation with ISS and IL-8 (r = 0.32, P = 0.02). ISS, and the serum IL-8 level are the most important determinants of clinical outcome in critically injured patients. A correlation exits between IL-8 and mortality and between ISS and IL-8.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the advancement in therapeutic modalities and improvement in the intensive care units (ICUs), traumatic injuries are the cause of more than half the deaths among children aged 1–14 years and are the second leading cause of emergency room visits after infections [1, 2]. In order to define an accurate system for grading the severity of injury and to predict the individual victim’s outcome, many scoring systems have been devised for stratifying trauma patients [3–6]. However, all these scoring systems have some problems in predicting mortality and outcome in individual patients following trauma [7–10].
Primary host inflammatory response defined as systemic inflammatory response syndrome (SIRS) has been shown to be activated by injury, infection and major surgical interventions [11]. This exaggerated host inflammatory response may contribute to compensatory anti-inflammatory response syndrome (CARS) [12]. The early release of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 contribute to the development of multiple organ dysfunction/failure syndrome [13–15]. Experimental and clinical studies have shown the effects of agents such as that suppress the early inflammatory response [16]. However, understanding of many mediators in the induction or inhibition of immunosuppressive and inflammatory processes associated with injury is incomplete. In addition, very little is known whether there is a correlation between trauma scoring systems and these markers. The main purpose of this study, therefore, was to determine whether a correlation exists between the main scoring systems such as pediatric trauma score (PTS), injury severity score (ISS), and pro-inflammatory cytokines such as interleukin-(IL-) 1β, IL-6, IL-8, and tumor necrosis factor alpha (TNF-α) and also to assess if any of these can be used to predict the outcome in patients under care at a trauma center.
Materials and methods
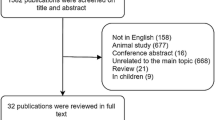
This study was a prospective collection of data on 47 children less than 15 years of age with blunt trauma, admitted to the Emergency Department between 2005 and 2006. All trauma patients were resuscitated and evaluated by the trauma team and management was uniform throughout the study period. The blood samples for cytokines analysis and routine laboratory analysis were taken just before resuscitation and PTS, ISS, systolic blood pressure and heart rate, were recorded at the Emergency Department. None of the patients were treated before hospitalization. Resuscitation was started by an emergency physician at the scene. After resuscitation, patients were admitted to the trauma center. On admission, cardiovascular and pulmonary function further stabilized using, central venous line and arterial line for monitoring, i.v. infusion via peripheral venous lines and mechanical ventilation in the appropriate patients. After complete diagnostics including all X-rays, abdominal ultrasound and CT scan, all patients were evaluated for age, sex, admission time, mechanism of injury, symptoms at admission, localization of intraabdominal organ injuries, associated injuries, treatment modalities, morbidity, and mortality rate. The solid organ injuries were identified by one or more of the following: abdominal paracenthesis, ultrasound (USG), intravenous pyelogram (IVP), computed tomography (CT).
Exclusion criteria for all patient groups were steroidal as well as nonsteroidal anti-inflammatory medication, any hormone therapy, and vascular obstruction (such as coronary heart disease, renal dysfunction, diabetes) and arrival time to hospital exceeding 12 h post traumatically. In addition, patients were subsequently excluded from this study, if they had suffered only head injury. Patient transportation times are very long in our study. Our university hospital is a referral hospital in our region and most trauma patients are first seen by state hospital physician and then are referred to our hospital if necessary and some of the patients are referred from rural areas and transportation takes time. Otherwise transport time for trauma patients in urban area is less than an hour. Our patients were not treated before arrival to our hospitalbecause we did not have enough prehospital pediatric surgeons; these patients are referred by other physicians and then most of them are referred to our center.
Each patient was evaluated according to several risk factors including age (under vs. above 10 years), interleukin-(IL-) 1β, IL-6, IL-8, and tumor necrosis factor alpha TNF-α. Data from each patient were also interpreted by the same surgeon (H.O.) in all patients with two different trauma severity indices: ISS and PTS. The ISS uses the AIS severity levels and tries to combine them into a single value that correlates with outcome. Each injury is assigned an AIS score and allocated to one of six body regions: head, face, chest, abdomen, extremities (including pelvis), and external. Only the highest AIS score in each body region is used for calculating the ISS. The three most severely injured body regions have their score squared and added to produce the ISS score. In case of a level 6 injury, the ISS is automatically set to 75. Thus the ISS ranges from 0 to 75, increasing with severity [17]. The separation of ISS between 15 or less for minor trauma and 16 or more for major trauma had been proposed as triage criteria [17]. The six variables of the PTS are: (1) weight; (2) airway; (3) SBP; (4) LOC; (5) open wounds; and (6) skeletal injuries. Each element is scored from +2 (normal) to −1 (the most severe injuries). A higher score on the PTS indicates a less injured patient. Patients scoring 8 or below are optimally treated at a level 1 pediatric trauma unit [18]. The relationship between overall mortality and the above-mentioned prognostic risk factors was also analyzed.
Assays
For the cytokine assays, blood samples of 10 ml arterial blood were drawn and immediately centrifuged for 10 min at 500g. The serum was centrifuged at 2,500 rpm and 4°C and then divided into three aliquots and stored at −80°C until further processing. Cytokine levels were evaluated with electroimmuno assay (EIA) (Biomedica Quantikine IL-8, Biomedica Immunotech EIA-IL-1, EIA-IL-6, EIA-TNF-α).
Statistical analysis
Data were entered and analyzed in a personal computer using SPSS version 10. Differences between survivors and nonsurvivors were analyzed by Student’s t-test and Mann–Whitney U-test, where applicable. Student’s t-test, one-way ANOVA, and Spearman’s Rho correlation were used as indicated. Univariate analysis was performed with Chi-square and Fisher’s exact test where appropriate. A P value of less than 0.05 was considered statistically significant.
Results
A total of 47 patients fulfilled the inclusion criteria. The demographics of patients are shown in Table 1. Of the 47 patients, 37 were boys and 10 were girls. The mean age was 8.2 ± 4.4 years (range 2–15 years). The mean transport time was 7.3 ± 4.8 h (range 2–12 h). The most common cause of trauma was fall (46%). All of the patients were treated conservatively. Patients were treated as follows; the hemodynamically stable patients with GI-II isolated abdominal organ injuries were monitored for 24 h following injury, the relatively unstable patients with ≥GIII isolated abdominal organ injuries were monitored for 72 h following injury. All of the six patients associated with thoracic injury were managed by means of tube thoracostomy.
The mortality rate for the series was 17%. Eight patients died; four due to cranial trauma and four due to multiple organ failure (MOF).
Descriptive statistics for independent variables are shown in Table 2. Prognostic factors such as IL-8 (P = 0.04), and ISS (P = 0.004) were significant in their relationship to mortality.
The univariate statistical analysis is outlined in Table 3. The following risk factors were analyzed to determine those that would predict the occurrence of mortality: age (≤10 years or >10 years), IL-1β (≤5 or >5), IL-6 (≤25 or >25), IL-8 (≤25 or >25), TNF-α (≤10, 10–20 or >20), ISS, and PTS. Some prognostic factors such as age, IL-1β, IL-6, PTS were not significantly correlated with mortality, whereas some other risk factors such as IL-8 (P = 0.004), >20 TNF-α (P = 0.04), and ISS (P = 0.007) were significant in their relationship to mortality. Chi-square and Fisher’s exact test were used for determining relative risk (Table 3). The relative risk of developing mortality was higher when two for each of the following risk factors were together: >10 ages, >25 IL-6, 10–20 TNF-α, >20 TNF-α, PTS ≤ 8, and ISS > 15.
There was a positive correlation between IL-8 and mortality (r = 0.31, P = 0.33), between ISS and mortality (r = 0.31, P = 0.0001) also, a positive correlation for mortality was present between ISS and IL-8 (r = 0.32, P = 0.02).
Discussion
Estimating the risk to life of injured patients is a key factor in setting priority for treatment and in quality control of treatment provided [19]. Mortality is related to at least four major variables: severity of the injury, host factors, quality of care, and time elapsed before definitive treatment. Pre-hospital trauma care could influence the survival rate of the trauma patients by reducing the transfer time to the hospital, improving skills available at the scene, and by making the optimal choice as to which hospital the patient is to be taken [20]. Trauma scoring systems have been proposed as a way to identify resources needed to provide medical care to victims of serious injury; they are designed to identify the characteristics of the injured population, clarify appropriate resources, and measure of risk-adjusted mortality [21]. In general, serum cytokine levels of multiple trauma patients are consistently increased during the first 3–5 days after trauma, and the principal role of cytokines in the development of organ failure is well documented. In addition, recently, it has also been proposed that the posttraumatic acute-phase response may be enhanced in case of a combined trauma, thus leading to increased mortality [22]. Therefore; the focus of this study was to determine whether a correlation exists between the main trauma-scoring systems and serum cytokine levels. Previous studies have demonstrated that neutrophil-mediated tissue injury is implicated in the pathogenesis of postinjury multiple organ failure [22]. The proinflammatory cytokines IL-6 and IL-8 contribute to this neutrophil-mediated tissue injury in vitro [23]. Partrick et al. [24] previously measured IL-6 and IL-8 in severely injured patients and found that elevated levels of these proinflammatory cytokines discriminate patients who ultimately develop postinjury multiple organ failure. In patients who had sustained a multiple trauma without any brain injury, the well-documented posttraumatic inflammatory response was noted, as reflected by increased cytokine serum levels (IL-6, IL-8) within the first 48 h after trauma [25]. Strecker et al. [26] demonstrated that IL-6, CK and, possibly, IL-8, may help to fill up the diagnostic gap we face in trying to estimate chest and soft tissue trauma in the early post-trauma state. Thus, early information on the extent of pulmonary trauma and soft tissue damage may influence the indications for early intubation and mechanical ventilation and may prevent pulmonary insufficiency and the development of acute respiratory distress syndrome (ARDS) and MOF [26–28]. In our study, the mean transport time for arrival to ED was about 7 h. This seems much longer than expected for an urban/tertiary center. However, this transport time reflects the time between the injury and arrival to our ED in which the time in other centers for referral patients is also included. In addition, none of the patients underwent laparotomy in our study. This may be due to the size of the study, which is relatively small. Our policy of treatment in this type of patients is usually non-operative approach, which may also have affected this result. In our study there was a positive correlation between IL-8 and mortality (r = 0.31, P = 0.33) and according to descriptive and univariate analysis, IL-8 was found to be significantly increased in nonsurviving patient and thus may act as markers as well as potential mediators of the postinjury response. In the present study, we observed that TNF-α and IL-1β were mildly elevated early following injury. Some of the previously published papers also showed increased levels of TNF-α and IL-1β early following injury [8, 10, 23, 24].
The PTS, which is a simple and quick anatomic and physiologic scoring system, is the only one designed specifically to be applied to children, and reported to be developed to predict the survival of injured children [18, 29]. Several reports have shown the validity of PTS to predict the severity of injury in those children in the most immediate danger of mortality [30, 31]. However, critics have also pointed out that the PTS suffers from scoring vagueness [18, 32]. For instance, the term “obtunded”, when used to describe a child, could be interpreted in a number of ways. Such vagueness lends itself to misinterpretation and inaccurate scoring [18, 32]. Our univariate statistical analysis showed that the relation between PTS and mortality was not significant. However, PTS < 8 was associated with a 3,300-times increased incidence of morbidity in comparison with PTS > 9.
While early mortality is dominated by severe head injury, later mortality may also be associated with severe thoracic and soft tissue injuries and involve different pathophysiological mechanisms. Whereas early mortality is the result of direct damage or acute haemorrhage, later mortality may be caused by an imbalance between the clearance capacity of the organism and the overall load of traumatic antigenic strain [26]. The ISS was first described by Susan Baker in 1974 [3]. It is an anatomical scoring system that provides an overall score for patients with multiple and complex injuries. Each injury is assigned an AIS score [3]. The ISS is widely used in trauma research to describe the severity of injury. In fact, it is well known that the ISS score is not useful as a triage tool and is known to be associated with risk of dying from injury [19]. The separation of ISS between 15 or less for minor trauma and 16 or more for major trauma was proposed as criteria [3]. The risk of complications developing was found to be higher in patients with an ISS ≥ 16 than in those with an ISS ≤ 15. The ISS correlates well with mortality and outcome. The mean ISS in our patients with nonsurvival was 22.87. The rate of mortality correlated well with the severity of injury as depicted by ISS (r = 0.31, P = 0.001). In present study, eight patients died. Four patients died due to serious cranial injuries and four patients died due to multiple injuries including cranial, thoracic, abdominal and extremity fractures. As a result, the present small-sized study showed a correlation between the admission blood IL-8 and the most commonly used scoring system ISS together with mortality.
References
Hall JR, Reyes HM, Meller JL, Loeff DS, Dembek R (1996) The outcome for children with blunt trauma is best at a pediatric trauma center. J Pediatr Surg 31:72–76
Aslar AK, Kuzu MA, Elhan AH, Tanik A, Hengirmen S (2004) Admission lactate level and the APACHE II score are the most useful predictors of prognosis following torso trauma. Injury 35:746–752
Baker SP, O’Neill B, Haddon W, Long WB (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
Champion HR, Sacco WJ, Carnazzo AJ, Copes W, Fouty WJ (1981) Trauma score. Crit Care Med 9:672–676
Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME (1989) A revision of the trauma score. J Trauma 29:623–629
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Cerra FB, Negro F, Abrams J (1990) APACHE II score does not predict multiple organ failure or mortality in postoperative surgical patients. Arch Surg 125:519–522
Collopy BT, Tulloh BR, Rennie GC, Fink RL, Rush JH, Trinca GW (1992) Correlation between injury severity scores and subjective ratings of injury severity: a basis for trauma audit. Injury 23:489–492
Deane SA, Gaudry PL, Roberts RF, Juul O, Little JM (1986) Trauma triage—a comparison of the trauma score and the vital signs score. Aust N Z J Surg 56:191–197
Eichelberger MR, Gotschall CS, Sacco WJ, Bowman LM, Mangubat EA, Lowenstein AD (1989) A comparison of the trauma score, the revised trauma score, and the pediatric trauma score. Ann Emerg Med 18:1053–1058
Baue AE, Durham R, Faist E (1998) Systemic inflammatory response syndrome (SIRS), multiple organ dysfunction syndrome (MODS), multiple organ failure (MOF): are we winning the battle? Shock 10:79–89
Bone RC, Newton Sir I (1996) Sepsis, SIRS, and CARS. Crit Care Med 24:1125–1128
Faist E (1996) The mechanisms of host defence dysfunction following shock and trauma. Curr Top Microbiol Immunol 216:259–274
Deitch EA (1992) Multiple organ failure: pathophysiology and potential future therapy. Ann Surg 216:117–134
Ayala A, Perrin MM, Wang P, Ertel W, Chaudry IH (1991) Hemorrhage induces enhanced Kupffer cell cytotoxicity while decreasing peritoneal or splenic macrophage capacity. Involvement of cell-associated tumor necrosis factor and reactive nitrogen. J Immunol 147:4147–54
Napolitano LM, Faist E, Wichmann MW, Coimbra R (1999) Immune dysfunction in trauma. Surg Clin North Am 79:1385–1416
Lefering R (2002) Trauma score systems for quality assessment. Eur J Trauma 28:52–63
Fani-Salek MH, Totten VY, Terezakis SA (1999) Trauma scoring systems explained. Emerg Med 11:155–166
Aharonson-Daniel L, Giveon A, Stein M, Israel Trauma Group (ITG), Peleg K (2006) Different AIS triplets: different mortality predictions in identical ISS and NISS. J Trauma 61:711–717
Vles WJ, Steyerberg EW, Meeuwis JD, Leenen LP (2004) Pre-hospital trauma care: a proposal for more efficient evaluation. Injury 35:725–733
Brink J A, Allen CF, Goslar PW, Barry MA (2001) Can we improve trauma mortality in a state with a voluntary trauma system. Am J Surg 182:738–742
Partrick DA, Moore FA, Moore EE, Barnett CC Jr, Silliman CC (1996) Neutrophil priming and activation in the pathogenesis of postinjury multiple organ failure. New Horiz 4:194–210
Biffl WL, Moore EE, Moore FA, Carl VS, Kim FJ, Franciose RJ (1994) Interleukin-6 potentiates neutrophil priming with platelet-activating factor. Arch Surg 129:1131–1136
Partrick DA, Moore FA, Moore EE, Biffl WL, Sauaia A, Barnett CC Jr (1996) Jack A Barney Resident Research Award winner. The inflammatory profile of interleukin-6, interleukin-8, and soluble intercellular adhesion molecule-1 in postinjury multiple organ failure Am J Surg 172:425–429 (discussed 429–431)
Seekamp A, van Griensven M, Lehmann U, Molituris U, Hildebrandt F, Pohlemann T (2002) Serum IL-6, IL-8 and IL-10 levels in multiple compared to traumatic brain injury and combined trauma. Eur J Trauma 28:183–189
Strecker W, Gebhard F, Perl M, Rager J, Buttenschon K, Kinzl L, Beck A (2003) Biochemical characterization of individual injury pattern and injury severity. Injury 34:879–887
Elmaraghy AW, Aksenov S, Byrick RJ, Richards RR, Schemitsch EH (1999) Pathophysiological effect of fat embolism in a canine model of pulmonary contusion. J Bone Joint Surg Am 81:1155–1164
Goris RJA, te Boekhorst TPA, Nuytink JKS, Gimbrere JSF (1985) Multiple-organ failure. Arch Surg 120:1109–15
Aprahamian C, Cattey RP, Walker AP, Gruchow HW, Seabrook G (1990) Pediatric trauma score. Predictor of hospital resource use? Arch Surg 125:1128–1131
Tepas JJ, Mollitt DL, Talbert JL, Bryant M (1987) The pediatric trauma score as a predictor of injury severity in the injured child. J Pediatr Surg 22:14–18
Ramenofsky ML, Ramenofsky MB, Jurkovich GJ, Threadgill D, Dierking BH, Powell RW (1988) The predictive validity of the pediatric trauma score. J Trauma 28:1038–1042
Reynolds EA (1992) Trauma scoring and pediatric patients. J Emerg Nurs 18:205–210
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ozturk, H., Yagmur, Y. & Ozturk, H. The prognostic importance of serum IL-1β, IL-6, IL-8 and TNF-α levels compared to trauma scoring systems for early mortality in children with blunt trauma. Pediatr Surg Int 24, 235–239 (2008). https://doi.org/10.1007/s00383-007-2083-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-007-2083-7