Abstract
Central venous access is frequently used in infants and children with a wide variety of conditions. This report evaluates our experience and the complications from central venous catheters (CVC) placed percutaneously in children at a public hospital of a developing country—Brazil. To identify associated complications, data were collected prospectively and 155 consecutive catheterizations in children at a public hospital over a nearly 8-month period were analyzed. Data collected included sex, age, weight, primary diagnosis, indication for placement, presence of blood coagulation disturbance, hospital department for procedure, type of anesthesia, type of catheter (diameter, lumen number, material), site of catheterization, number of attempts, number of puncture sites, complications during puncture, the time catheter remained in place, later complications (mechanical, infectious) and reason for catheter removal. A total of 155 catheters were placed in 127 patients. There were 130 neck lines and 25 groin lines. The success rate was 81.9% at the initially chosen puncture site and rose to 100% with the inclusion of the second site. Perioperative complications occurred in nine (5.8%) cases, including six (3.9%) hematomas and three (1.9%) arterial puncture. There was no pneumothorax, hemothorax or hydrothorax. During the time the catheter remained in place, there were 51 (32.9%) complications, of which 33 (21.3%) were mechanical and 18 (11.6%) suspected catheter-related infection. These complications were responsible for the removal of the catheter. Despite the relatively high complication rate there were no catheter-related deaths. Body weight was significantly lower for children who underwent more than one puncture site (P=0.01). Age, sex, type of catheter and primary diagnosis were not associated with complications. Knowledge of anatomy and familiarity with the Seldinger technique highly increase the catheterization success rate, with few surgical complications. A better nursing care of CVC is emphasized. The available modern venous catheters at a public hospital in Brazil have contributed to improve the quality of pediatric medical care. Nowadays, the percutaneous CVC is the preferred method in pediatric patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Central venous catheterization (CVC) is necessary for a great number of inpatients, particularly children. Though indispensable, CVC is not without risk. The use of central venous catheters may be associated with adverse events, originated during or after insertion of the catheter [1, 2].
The literature shows that the venous catheter inserted through a wide bore needle (Intracath®) is still widely used [3–5]; however, this technique and the venous dissection are associated with high morbidity, particularly among pediatric patients [6]. Traditionally, anatomic landmarks have been used to locate the central veins for catheterization. However, this technique can be difficult in small children, infants and, specially, neonates, leading to higher failure rates and complications.
The use of ultrasound guidance reduces the number of mechanical complications, the number of catheter placement failures and the time required for insertion [7, 8]. However, the equipment needed for this technique is expensive and may be cumbersome for routine practice.
Central venous catheterization by the Seldinger technique, although involving a slightly higher cost, is a lower risk procedure and very important for pediatric patients. In spite of substantial evidence of its practicality in daily use, the consensus in relation to CVC is not unanimous, because of associated complications.
We performed a prospective study to evaluate our experience and the complications from CVC placed percutaneously in children at a public hospital of a developing country—Brazil.
Methods
The study was approved by the institutional ethical review board. A descriptive study of CVC was undertaken by the Seldinger technique in subjects, aged less than 18 years, of the Federal University of Minas Gerais/University Hospital (HC/UFMG), during the period January–September 2003.
A standardized protocol for data collection containing identification information and the following variables: gender, age, weight, primary diagnosis, indication for placement, presence of blood coagulation disturbance, hospital unit location for procedure, type of anesthesia, type of catheter (diameter, lumen number, material), site of catheterization, number of attempts, number of puncture sites, complications during puncture, the time catheter remained in place, later complications (mechanical, infectious) and reason for catheter removal.
Coagulograms (prothrombin activity, partial thromboplastin time) and platelet counts were the pre-operative routine laboratory exams undertaken. Pre-existing blood coagulation disturbances were corrected before procedures. Children undergoing more than one catheter placement during the period of hospitalization were considered as new cases. Cardiac catheters, hemodialysis catheters, catheters of long term (Hickman and Broviac) and peripherally inserted central catheters (PICC) were excluded from the analysis.
Surgical technique
Central venous catheterizations were performed by the author (when he was a pediatric surgical resident), with the assistance of a professor of pediatric surgery, under local or general anesthesia [with or without orotracheal intubation (OTI)]. All catheters were composed of polyurethane. Subclavian, internal jugular, external jugular or femoral veins were punctured. All lines were placed percutaneously using the Seldinger technique. The blind puncture based in anatomic landmarks was used because Doppler ultrasound guidance was not available.
After each procedure, chest or abdominal X-rays were obtained to check adequate position of the catheter tip (superior or inferior vena cava) and the diagnosis of possible complications secondary to the puncture, like pneumothorax, hemothorax or hydrothorax. In cases in which it was not possible to identify the catheter in the radiograph, another radiograph was taken, with non-ionic iodinated contrast medium injected into the catheter. Incorrectly positioned catheters were rapidly repositioned.
The catheters were maintained for the necessary therapeutic time, and children were monitored for the period the catheter remained in situ. The reasons for catheter removal were: (a) disappearance of the reason for CVC, (b) suspected catheter-related sepsis, (c) irreversible obstruction. Daily care, including monitoring and dressing changes, was undertaken by the nursing team. Transparent dressings were used, after cleaning the catheter insertion site with saline solution. Antibiotic dressings were not used, and dressings changed as needed.
Catheter removal and catheter-related infection
Patients were carefully monitored for signs of suspected catheter-related bloodstream infection. When signs of systemic infection appeared, cultures were done on the peripheral blood and catheter blood. Central venous catheter removal was the treatment of choice for the suspicion of catheter-related infection. Catheter-related sepsis was defined as a catheter tip or blood culture yielding the same organism as the peripheral blood culture and the existence of clinical symptoms of sepsis for which no anatomical focus other than the catheter could be identified. Colonization was defined as no clinical signs of sepsis but positive catheter tip culture.
Statistical analysis
For statistical analysis, means (x), standard deviation (SD) and distribution frequency (%) were calculated. The Student t test was used for comparison between averages and Fisher’s exact test for comparison between the frequencies of the analyzed variables. The level of significance was established at P≤0.05.
Results
During the study period, 155 central venous catheters were inserted into 127 patients (58.7% male and 41.3% female). Descriptive characteristics of CVC placement are presented in Table 1.
The mean age was 4.0±4.0 years, ranging from 1 day to 17 years. Concerning the age group, 48.4% of catheter placements were made in newborns and infants (<2 years). The mean weight was 14.4±11.6 kg ranging from 1.6 to 58.0 kg. Only 20.7% of CVCs were in children, over 20.0 kg-weight. Neoplasms, congenital malformations and renal disease represented more than half (51.6%) the diagnoses at the time of venous puncture. The main indication for CVC placement was antibiotic therapy for periods over 7 days (47.7%) and 49 of the 155 catheters (31.6%) had more than one function. Twenty-eight catheters were placed in children diagnosed with blood coagulation alterations, without any additional complication.
The majority of catheters (81.9%) were placed in the operation room and the pediatric intensive care unit. With respect to anesthesia, the majority of placements (89.0%) were undertaken under general anesthesia with OTI.
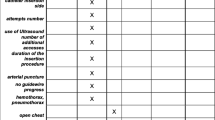
Table 2 shows the characteristics of venous puncture undertaken in each procedure.
The sites chosen initially for puncture were the internal jugular vein, followed by the external jugular vein, subclavian vein and femoral vein, respectively. There was no preference of side to access the superior vena cava; however, the approach to access the inferior vena cava was the right side, selected in 92% of cases.
All CVC attempts were successful. Of the 155 CVC attempts, 127 (81.9%) were placed at the site initially chosen by the surgeon and 114 (73.5%) were inserted with only one puncture. In the 28 cases (18.1%) in which the initially chosen site was not successful, another site for a new puncture and catheter insertion was necessary. This occurred due to difficulties with the progression of the wire-guide and/or the catheter in 21, hematoma in 4 and failure to puncture the vein in 3. The external jugular vein was responsible for 52.4% of the site changes due to the difficulties in progressing with the wire-guide. In 16 children (13.2%) more than one CVC was necessary during the period of hospitalization.
There were significant differences between the number of sites used and the weight of children (P=0.01). The mean weight of children that required more than one site (10.2±8.8 kg) for successful catheter placement was lower than for children requiring only a single venous site for placement (15.4±11.9 kg).
The correct positioning of the catheter tip was achieved in 144 (92.9%) placements. Conventional radiography was sufficient (thorax or abdomen X-ray) to identify the catheter in 137 (88.4%) cases. Iodinated contrast medium injection through the catheter and further radiography were necessary for the identification of the catheter in only 18 (11.6%) of the CVC placements. There was no statistically significant difference between the frequencies of catheters incorrectly positioned and the site of puncture (P=0.12).
The mean catheter duration was 16±13 days (range 1–75).
In the majority of cases (146 out of 155; 94.2%) there were no complications during venous puncture and catheter placement. In the remaining nine (5.8%) cases, hematoma and accidental arterial puncture occurred with no clinical repercussions. There were no cases of pneumothorax or hemothorax.
Statistical analysis revealed no significant correlation between the number of complications and the patient age group (P=0.08) or sex (male vs. female). We found no difference in the incidence of complications by catheter type or primary disease.
Catheter no longer required (55%) was the main indication for removal. Among the removed catheters, 33 were due to mechanical problems and 18 due to suspected catheter-related infection. The majority (78.7%) did not present any mechanical problem. Accidental loss (21/33) and obstruction (10/33) of the catheter were the main reasons for interruption of catheterization (Table 3). Catheter-related sepsis rate was 1.3%. In these cases, Staphylococcus aureus and Klebsiela pneumoniae were isolated from the peripheral blood and catheter tip cultures.
Discussion
The availability of CVC percutaneously has significantly improved the care of pediatric patients. The pediatric catheterization is technically more difficult and associated with more complications than in adult patients [9, 10].
This study is unique in which four different sites—internal jugular, external jugular, subclavian and femoral veins—were evaluated. There are larger case series but they are retrospective, including long-term catheters [1, 2].
The overall success rate found in the present study (100%) corroborates other published studies (59–100%), which characterize the pediatric application of the Seldinger technique as safe and with low morbidity (5.8%) [11–20]. The profile of this case series does not differ from other studies [1, 16, 18, 21]. The mean age of 4 years is similar to the majority of reports in the literature. Although age and weight were reported previously as factors associated with lower rates of success by some authors [7, 13, 17, 19, 20], these factors did not influence our global success rate. However, we observed that in children with a lower body weight a change of puncture site for CVC was statistically significant (P<0.05).
The majority of the procedures were undertaken with general anesthesia, in the operating room, which probably contributed to the good results obtained, as advocated in some publications [13, 22]. Our study supports the idea that children present no increased risk when the procedure is performed under controlled conditions.
In this series, the internal jugular vein was preferably used for the primary puncture. However, individual anatomical aspects must be taken into account, as well as pre-operative laboratories exams, the clinical condition of the patient and the physician’s experience. In cases with blood coagulation disorders, the external jugular vein and femoral vein are excellent alternatives, due to the low risk of complications originating from the arterial puncture and bleeding.
The low success rate of the external jugular vein for CVC is due to its tortuous path and the presence of valves, which can prevent the progress of the guide-wire into the thorax. However, during this study, we showed that placing the guide-wire in a central position is not essential for the success of catheterization. In the present study, even without the prior introduction of the guide-wire into the thorax, the flexibility of the catheter allowed its progression within the vein until the junction of the superior vena cava with the right atrium. A success rate of 72.5% was obtained in CVC by the external jugular vein, the largest one described in children in the literature. We attribute this success to this small modification of the Seldinger technique for insertion of the catheter.
Several studies have examined the morbidity and mortality associated with central venous catheterization in children, reporting complication rates of 0.7–23% [13–27]. The most common complications, such as arterial puncture, hematoma and pneumothorax, varied according to the puncture site [1, 24]. In this study, the incidence of immediate complications was 5.8%, all considered minor, and did not require any surgical intervention. The use of ultrasound (US) guidance has been promoted as a method for reducing the risk of complications during central venous catheterization. In hospitals where ultrasound equipment is available and physicians have adequate training, the use of US guidance should be routinely considered for cases in which internal jugular venous catheterization will be attempted [7, 8].
In an analysis of complications during CVC, we agree that the physician’s experience is an important factor, although controversy exists in this respect. While some authors consider it of crucial importance [13, 16, 21, 25], others have demonstrated no association [1, 7]. The association between the need for another site of CVC placement and the incidence of complications as described by some authors [1, 18] was not observed in our study.
Radiographical confirmation of successful catheter placement is regarded as fundamental by several authors. Catheter misplacements were also associated with a significant increase in complications [12–14, 16, 20, 21]. Intraoperative fluoroscopy during CVC placement provides the benefit of placement verification with immediate repositioning possible. Once placement is confirmed with fluoroscopy, the routine postprocedure chest X-ray appears to be unnecessary [26].
There are few publications that investigate the long-term complications of CVC [13, 15, 21]. In our case series, 32.9% of catheters, while in situ, developed a problem (mechanical or infectious). Accidental loss was the main mechanical complication (21/33) which directs our attention to the fundamental question related to CVC, which is the importance of a trained team—doctors and nurses—for successful handling and care during and after catheterization. Almost all mechanical complications can be prevented or minimized.
The incidence of catheter-related sepsis in large pediatric series varies from 1.4 to 5.8% [2, 5]. A careful assessment of suspected catheter-related infection is important since this was responsible for the removal of 11.6% of catheters in our case series, while in only 2 (1.3%) of these cases catheter-related sepsis was confirmed by cultures. Such studies may be helpful in identifying a specific patient population at high risk for catheter-related infection.
The incidence of thrombotic complications during CVC placement will be the subject of another study in our institution. Some authors have reported that thrombosis related to CVC placement is often undiagnosed since it is asymptomatic in the majority of children. Probably larger case series will be able to identify factors related to the success of CVC placement and complications in children, according to each puncture site.
In summary, we found central venous catheterization in children to be a relatively safe procedure, with a 5.8% associated morbidity and no mortality in this series. Our overall primary success rate was 81.9% but may be improved by the use of US guidance.
In our institution, the pediatric venous dissection (flebotomies) is a procedure increasingly less used. The recent acquisition and subsequent availability of these venous catheters inserted by Seldinger technique show our commitment to improve the quality of our pediatric care, despite the difficulties common to a developing country, such as Brazil.
References
Johnson EM, Saltzman DA, Suh G, Dahms RA, Leonard AS (1998) Complications and risks of central venous catheter placement in children. Surgery 124:911–916
Stenzel JP, Green TP, Fuhrman BP, Carlson PE, Marchessault RP (1989) Percutaneous central venous catheterization in a pediatric intensive care unit: a survival analysis of complications. Crit Care Med 17(10):984–988
Prince SR, Sullivan RL, Hackel A (1976) Percutaneous catheterization of internal jugular vein in infants and children. Anesthesiology 44(2):170–174
Hall DMB, Geefhuysen J (1977) Percutaneous catheterization of the internal jugular vein in infants and children. J Pediatr Surg 12:719–722
Eichelberger MR, Rous PG, Hoelzer DJ, Garcia VF, Koop CE (1981) Percutaneous subclavian venous catheters in neonates and children. J Pediatr Surg 16(4):547–553
Newman BM, Jewett TC Jr, Karp MP, Cooney DR (1986) Percutaneous central venous catheterization in children: first line choice for venous access. J Pediatr Surg 21(8):685–688
McGee DC, Gould MK (2003) Preventing complications of central venous catheterization. N Engl J Med 348(12):1123–1133
Randolph AG, Deborah JC, Gonzales CA, Prible CG (1996) Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med 24:2053–2058
Cobb LM, Vinocur CD, Wagner CW, Weintraub WH (1987) The central venous anatomy in infants. Surg Gynecol Obstet 165:230–234
Steinberg C, Weinstock DJ, Gold JP, Notterman DA (1992) Measurements of central blood vessels in infants and children: normal values. Cathet Cardiovasc Diagn 27:197–201
Venkataraman ST, Orr RA, Thompson AE (1988) Percutaneous infraclavicular subclavian vein catheterization in critically ill infants and children. J Pediatr 113(3):480–485
Pybus DA, Poole JL, Crawford MC (1982) Subclavian venous catheterization in small children using the Seldinger technique. Anaesthesia 37:451–453
Hüttel MS, Christensen P, Olesen AS (1985) Subclavian venous catheterization in children. Acta Anaesthesiol Scand 29:733–735
Coté JC, Jobes DR, Schwartz AJ, Ellison N (1979) Two approaches to cannulation of a child’s internal jugular vein. Anesthesiology 50:371–373
Kanter RK, Gorton JM, Kathy Palmieri RVT, Tompkins JM, Smith F (1989) Anatomy of femoral vessels in infants and guidelines for venous catheterization. Pediatrics 83(6):1020–1022
Humphrey MJ, Blitt CD (1982) Central venous access in children via the external jugular vein. Anesthesiology 57:50–51
Taylor EA, Mowbray MJ, McLellan I (1992) Central venous access in children via the external jugular vein. Anaesthesia 47(3):265–266
Bonventre EV, Lally KP, Chwals WJ, Salem W, Hardin WD Jr, Atkinson JB (1989) Percutaneous insertion of subclavian venous catheters in infants and children. Surg Gynecol Obstet 169:203–205
Çitak A, Karaböcüoğlu M, Üçsel R, Uzel N (2002) Central venous catheters in pediatric patients—subclavian venous approach as the first choice. Pediatr Int 44(1):83–86
Belani KG, Buckley JJ, Gordon JR, Castaneda W (1980) Percutaneous cervical central venous line placement: a comparison of the internal and external jugular vein routes. Anesth Analg 59(1):40–44
Chen KB (2001) Clinical experience of percutaneous femoral venous catheterization in critically ill preterm infants less than 1.000 grams. Anesthesiology 95(3):637–639
Postel JP, Quintard JM, Richard J, Delaplace R, Bernard F, Canarelli JP (1990) Development of a safe technique for central venous access in pediatrics. Our experience with 700 percutaneous central catheters. Chir Pediatr 31(4–5):219–222
Hayashi Y, Uchida O, Takaki O, Ohnishi Y, Nakajima T, Kataoka H et al (1992) Internal jugular vein catheterization in infants undergoing cardiovascular surgery: an analysis of the factors influencing successful catheterization. Anesth Analg 74:688–693
Goni Orayen C, Perez Martinez A, Ruiz Cano R, Carrascosa Romero MC, Vazquez Garcia MS, Martinez Gutierrez A (1999) Central venous access by Seldinger technic in neonatology. Cir Pediatr 12(4):165–167
Kron IL, Rheuban K, Miller ED, Lake CL, Nolan SP (1985) Subclavian vein catheterization for central line placement in children under 2 years of age. Am Surg 5:272–273
Janik JE, Cothren CC, Janik JS, Hendrickson RJ, Bensard DD, Patrick DA et al (2003) Is a routine chest x-ray necessary for children after fluoroscopically assisted central venous access. J Pediatr Surg 38(8):1199–1202
Jung C, Bahk J, Kim M, Lee K, Ko K (2002) Head position for facilitating the vena caval placement of catheters during right subclavian approach in children. Crit Care Med 30(2):297–299
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cruzeiro, P.C.F., Camargos, P.A.M. & Miranda, M.E. Central venous catheter placement in children: a prospective study of complications in a Brazilian public hospital. Ped Surgery Int 22, 536–540 (2006). https://doi.org/10.1007/s00383-006-1671-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-006-1671-2