Abstract
In trisomy 9 mosaicism, plexus hypertrophy has been described as a phenotypical feature and cause of hydrocephalus. We report on a 15-month-old child with hydrocephalus and trisomy 9 mosaicism primarily diagnosed in amniocentesis. After implantation of a ventriculoperitoneal shunt and subsequent revision, he presented with an exhaustion of peritoneal absorption leading to massive ascites. The implantation of a peritoneal drainage offered the unique opportunity to monitor cerebrospinal fluid (CSF) production indirectly via abdominal CSF drainage. In an individual trial, we performed endoscopic choroid plexus cauterization to reduce cerebrospinal fluid production, which failed to reduce excessive CSF production. In a second procedure, a ventriculoatrial shunt was implanted and succeeded to treat persistent hydrocephalus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trisomy 9 mostly leads to death in early fetal stages. However, affected individuals with genetic mosaicism can develop a variety of phenotypical manifestations. In a variety of cases of choroid plexus hypertrophy, genetic mutations of chromosome 9p have been described [1, 6]. Due to excessive cerebrospinal fluid (CSF) production, hydrocephalus is common and primarily treated via implantation of a ventriculoperitoneal shunt (VPS). Besides infection, dislocation or valve dysfunction exhaustion of peritoneal CSF resorption is a well-known feature [4]. The amount of secreted CSF can exceed 2 L per day. Therefore, patients undergo optional treatment patterns, such as conversion to ventriculoatrial shunting (VAS). Choroid plexus coagulation (CPC) has also been discussed before for malresorptive or hypersecretory hydrocephalus (HCP) [2,3,4]. Due to varying success rates, it remains controversial [5]. Here, we report a case of a 15-month-old boy treated with CPC, after VPS failed several months after implantation. Finally, due to insufficient decrease of CSF production after CPC, a VAS was implanted with satisfying results.
Case presentation
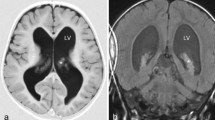
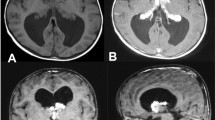
The 15-month-old child was diagnosed before with macrocephaly and retardation as phenotypic expression of a trisomy 9 mosaicism. A hydrocephalic configuration had been found and the suspected CSF overproduction had been treated with a VPS 9 months prior at another facility (Burr Hole, OSV II-valve, Integra LifeSciences, NJ, USA). Persistent percentile-crossing head growth, sun-down phenomenon and irritability, and persistent ventricular enlargement in MRI prompted a valve replacement with a programmable valve (Miethke proGAV 2.0, Miethke, Potsdam, Germany), which was performed 2 days prior to re-admission. Valve dysfunction or more likely excess of the OSV-II draining capacity is a possible reason for insufficient CSF drainage. Re-admission then occurred due to abdominal distension and poor general health. Clinical examination revealed 77.0-cm body length (percentile 3.3), 8.57 kg weight (percentile 2.4), head perimeter 52.0 cm (percentile 99.8), retained head veins, a taut frontal fontanelle, no distortion of pupil movement, and no dawn phenomenon. Ultrasound of head and abdomen demonstrated a stable intracranial status without progressive ventricle size but massive ascites (Fig. 1c). A peritoneal drainage was implanted to remove intra-abdominal fluid in assumption of a gastro-intestinal origin of the ascites. Drained volumes are depicted in Fig. 2. A cranial MRI (Fig. 1a, b) confirmed a stable hydrocephalus with enlargement of internal and external CSF spaces as well as a hypertrophy of choroid plexus. It was postulated that the excessive CSF hypersecretion caused the pronounced ascites. To avoid another invasive procedure, a pharmaceutical therapy with acetazolamide was started as an individual treatment trial, which lead to an immediate decrease in abdominal CSF drainage (Fig. 2). Due to metabolic acidosis and increasing base excess in blood gas analysis, this treatment had to be abandoned. After laboratory tests confirmed the suggested ascites being CSF, CPC was suggested as individual treatment trial after parents’ consent. CPC was performed via bi-occipital burr holes using a rigid endoscope (Little Lotta, Karl Storz GmbH, Tuttlingen, Germany) (Fig. 3). Here, the massively enlarged, hypertrophic, and hyperperfused choroid plexus was reduced in volume from 15.5 to 12.5 ml (20% reduction, Fig. 1e, f). It is to state that the coagulation was performed superficially to disrupt CSF production in the ependyma. Post-operatively, peritoneal catheter volumes decreased rapidly from 1.2 l per day to 400 ml per day. During the following 3 days, pre-CPC drainage volumes were reached again so that shunt conversion to VAS was indicated and finally performed 13 days after admission to our department. As presented in Fig. 2, external peritoneal drainage was sufficiently reduced and the peritoneal catheter could be removed completely 2 days after VAS implantation. The subsequent clinical course was uneventful and the child could be released the twelfth day after second surgery. Follow-up examinations revealed no newly acquired neurological deficits and regular VAS function without new signs of ascites (Fig. 1d).
Left: T2 weighed pre-operative cranial magnetic resonance imaging in axial (a) and sagittal (b) orientation; middle: abdominal ultrasound before intervention presenting massive ascites (c) and follow-up examination 5 weeks after ventriculoatrial shunting (d); right: volumetric analysis (via segmentation) of choroid plexus before (e) and after (f) choroid plexus coagulation. (A) = ascites, (L) = liver. The volume of the choroid plexus decreased about 20%
Conclusion
Trisomy 9 mosaicism is a rare but well-known condition. Choroid plexus hypertrophy with associated hypersecretory hydrocephalus can be a clinical feature in these patients. In this specific constellation of hydrocephalus, neither pharmacological treatment with acetazolamide as well as endoscopic CPC nor VPS has been a sufficient treatment option. A primary VA shunt treatment seems to be the treatment of choice for future cases.
References
Boxill M, Becher N, Sunde L, Thelle T (2018) Choroid plexus hyperplasia and chromosome 9p gains. Am J Med Genet A 176(6):1416–1422. https://doi.org/10.1002/ajmg.a.38697
Dezena RA (2016) Neuroendoscopic choroid plexus coagulation in the current pediatric neurosurgery. J Neurosurg Sci 60(3):287–288
Okano A, Ogiwara H (2018) Long-term follow-up for patients with infantile hydrocephalus treated by choroid plexus coagulation. J Neurosurg Pediatrics 22(6):638–645. https://doi.org/10.3171/2018.6.PEDS1840
Puerta-Roldan P et al (2017) Hidrocefalia por hiperplasia de plexos coroideos en un paciente con mosaicismo de trisomia 9. Un verdadero reto diagnostico y terapeutico. Rev Neurol 65(3):112–116
Sardana H, Kedia S (2019) Letter to the editor. infantile hydrocephalus treated by choroid plexus coagulation. J Neurosurg Pediatrics:1–2. https://doi.org/10.3171/2019.3.PEDS19130
Tonni G, Grisolia G (2013) Ultrasound diagnosis of central nervous system anomalies (bifid choroid plexus, ventriculomegaly, Dandy-Walker malformation) associated with multicystic dysplastic kidney disease in a trisomy 9 fetus: case report with literature review. J Clin Ultrasound 41(7):441–447. https://doi.org/10.1002/jcu.21999
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors I declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kasper, J., Krause, M., Siekmeyer, M. et al. Choroid plexus coagulation in trisomy 9 mosaic–related hydrocephalus—a case report. Childs Nerv Syst 36, 1803–1805 (2020). https://doi.org/10.1007/s00381-020-04643-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04643-1