Abstract
Background
Tumors within the pineal region represent 1.5 to 8.5% of the pediatric brain tumors and 1.2% of all brain tumors. A management algorithm has been proposed in several publications. The algorithm includes endoscopic third ventriculostomy (ETV) and biopsy in cases presenting with hydrocephalus. In this series, we are presenting the efficacy of a single-trajectory approach for both ETV and biopsy.
Methods
Eleven cases were admitted to Alexandria main university hospital from 2013 to 2016 presenting with pineal region tumors and hydrocephalus. Mean age at diagnosis was 11 years (1–27 years). All cases had ETV and biopsy using rigid ventriculoscope through a single trajectory from a burr hole planned on preoperative imaging. Follow-up period was 7–48 months.
Results
All 11 cases presented with hydrocephalus and increased intracranial pressure manifestations. Histopathological diagnosis was successful in 9 out of 11 cases (81.8%). Three cases were germ-cell tumors, two cases were pineoblastomas, two cases were pilocytic astrocytomas, and two cases were grade 2 tectal gliomas. Five of the ETV cases (45.5%) failed and required VPS later on. Other complications of ETV included one case of intraventricular hemorrhage and a case with tumor disseminated to the basal cisterns.
Conclusion
In our series, we were able to achieve ETV and biopsy through a single trajectory and a rigid endoscope with results comparable to other studies in the literature.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tumors within the pineal region represent 1.5 to 8.5% of the pediatric brain tumors and 1.2% of all central nervous system tumors [14, 42, 50, 53, 57]. Although many of the published articles regarding tumors arising in this area have suggested almost a unified management scheme, the optimal management is still controversial especially as regards to certain histopathologies [6, 26, 33, 57]. In patients who present with mass in the pineal region, the following should be taken into consideration: Is the tumor arising from the pineal gland or a neighboring structure? Is it unifocal or is it involving other areas such as the suprasellar region? Is it localized to the quadrigeminal cistern or has it already disseminated? Does the diagnosis need histological proof or CSF tumor markers are enough especially in germ cell tumors? If biopsy is needed, can it be achieved together with the endoscopic third ventriculostomy (ETV), stereotactic biopsy, or through an open surgical approach? [18, 57].
Biopsy can be acquired from a pineal region mass, either during ETV or via stereotactic biopsy. Although the later may provide more diagnostic tissue [6], in this study, we preferred acquiring the biopsy through ETV for the following reasons: it allows the treatment of hydrocephalus through opening the floor of the third ventricle to the interpeduncular cistern, it avoids injury of the deep venous system, it allows the exploration of the ventricles and discovery of metastasis, and it allows hemostasis. It also allows the evacuation of associated cysts that aid in the relief of hydrocephalus and allows CSF sampling. Furthermore, it allows the visualization of different parts of the tumors and the avoidance of biopsy acquisition from vascularized areas [39]. On contrary, stereotactic biopsy is associated with relatively higher risk of hemorrhage in pineal region tumors [16].
The efficacy of ETV and biopsy has been reviewed several times in the literature [4, 5, 55]. A complete success is recognized when the ETV remains patent even after open surgical approach and the harvested biopsy is diagnostic. The procedure has been described to be done using both flexible and rigid endoscope, through single trajectory and through two burr holes. In this series, we are reporting our experience using a rigid endoscope through a single trajectory and the outcome in comparison with previous reports.
Methods
Patients
After approval of the local ethics committee of Alexandria University and checking the presence of the appropriate formal consents according to the committee’s standards, we have reviewed the records of 13 consecutive cases that were admitted to Alexandria main university hospital from 2013 to 2016 presenting with pineal region tumors and hydrocephalus (Table 1). There were 10 males and 1 female. Mean age at diagnosis was 11 years (1–17 years). Written informed consent was obtained from the parents of cases 1, 2, and 3 for publication of this case series and any accompanying images.
Preoperative data
The clinical presentation of all cases is summarized in Table 1. All cases had magnetic resonance imaging (MRI) with contrast enhancement before the procedure.
The decision to proceed with ETV and biopsy was taken as the initial step of the management algorithm protocol for such cases in our university hospital (Fig. 1). Only one case had emergency external ventricular drain placement before ETV. Follow-up period was 7–48 months. One case has died 7 months after the procedure due disease progression.
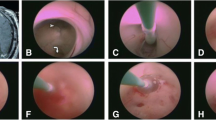
Endoscopic technique
All cases that had ETV were done using Gaab™ ventriculoscope system by Karl Storz®. The system includes a biopsy forceps that was used for sampling tissue. Some authors advised the acquisition of 8 to 12 samples [8]; in this study, six to eight biopsies were harvested for histopathological examination. However, in some cases, the biopsies were limited in tumors showing moderate to high vascularity for fear of uncontrollable bleeding. Cases were positioned supine with the head slightly flexed as usual for ETV. A right frontal inverted U-shaped incision anterior to the coronal suture was used in all cases. Burr hole was done using Hudson’s perforator, 1–2.5 cm anterior to the coronal suture and 1.5 to 3 cm lateral to the midline. The precise position was planned on individual basis on the sagittal and coronal series of the preoperative MRI. The trajectory planned on the imaging was intended to allow visualization of the posterior wall of the third ventricle without unintended injury to the boundaries of the foramen of Monroe. In all cases, ETV was done before biopsy acquisition when the vision is clear as sampling may lead to bleeding and obscuration of the field. Columns of the fornix were visualized at the end of each procedure.
CSF samples for tumor markers were acquired during the procedure for CSF diversion. Due to logistic/economic issues, we were not able to have the results intraoperatively; therefore, an attempt for harvesting a biopsy was planned in all cases.
Only one case required the insertion of an external ventricular drain (EVD) after imperfect bleeding control after biopsy acquisition.
Results
All 11 cases presented with hydrocephalus and increased ICP manifestations. One case had Parinaud syndrome at presentation, three cases had abducent palsy, and one case presented to the ED with disturbed level of consciousness. There was also a 1-year-old infant who presented with increased head circumference.
Elevated CSF markers were found in the three cases (Table 1). Histopathological diagnosis was successful in 9 out of 11 cases (81.8%). Out of the diagnosed nine cases, two cases were germinomas, one case was an endodermal sinus tumor, two cases were pineoblastomas, two cases were pilocytic astrocytomas, and two cases were grade 2 tectal gliomas. We did not find a relationship between the sample size in this study and failure to achieve histopathological diagnosis.
The ETV was successful in six patients (54.5%) of the cases with resolution of hydrocephalus. Five of the ETV cases (45.5%) failed and required VPS later on. Failure was attributed to massive IVH in one case and was unknown in the other four cases; however, it could be related to minimal bleeding that usually occurs after sampling. The median duration between ETV and VPS insertion was 20 days (12–39 days). We did not encounter any visible forniceal injury after the procedure. Only one case was obtunded in the ICU for 2 days post-operatively (case no. 5); this case was comatosed on admission, which explains the delayed post-operative recovery.
Complications of VPS insertion after ETV and biopsy included obstruction and infection in two cases and overdrainage and subdural collection in one case. The later occurred after both surgical resection and VPS insertion.
Further management included open surgical resection through supracerebellar infratentorial approach for five cases. These cases included a pineoblastoma and a pilocytic astrocytoma. It also included a pure germinoma that had normal tumor markers and the biopsy acquired endoscopically was not diagnostic; the second one was mixed germ-cell tumor that was diagnosed by both tumor markers and endoscopic biopsy. However, the disease did not show adequate response to adjuvant treatment. It also included an endodermal sinus tumor that showed progression after adjuvant treatment. The later died from extensive disease dissemination even after surgery.
Illustrative cases
Case 1
Eight-year-old male patient presented to the emergency department with disturbed level of consciousness, abducent palsy, and grade 3 papilloedema. The patient had increased blood AFP. The patient MRI revealed a posterior third ventricular mass extending to the pineal region and hydrocephalus (Fig. 2a). Third ventriculostomy and biopsy were done. The biopsy revealed germ cell tumor consistent with endodermal sinus tumor. The patient has received chemotherapy for 3 months with no significant response. Further surgery was done thorough anterior transcallosal approach. Partial resection was achieved. The patient started another cycle of chemotherapy in addition to craniospinal irradiation. The patient presented 2 months after the surgery with disturbed level of consciousness. CT brain revealed aggressive recurrence with multiple brain deposits (Fig. 2b, c). The patient died 2 days later.
Case 2
Fourteen-year-old male patient presented to the emergency department with pineal region mass and hydrocephalus (Fig. 3a). The patient had immediate endoscopic third ventriculostomy and biopsy. CSF samples that were collected for tumor markers showed elevation of the AFP. Endoscopic biopsy was showing germinoma. The patient had post-operative chemotherapy and radiotherapy. Complete response was achieved using adjuvant therapy alone (Fig. 3b).
Case 3:
Thirteen-year-old male patient presented to the outpatient clinic with headache and blurring of vision. Fundus examination was showing grade 1 papilloedema of the optic disk. MRI brain was showing a posterior third ventricular mass extending posteriorly to the pineal region (Fig. 3). Endoscopic third ventriculostomy and biopsy were done. The pathology came out to be pilocytic astrocytoma. After thorough discussion with the family, they decided not to operate on him at the time being until the tumor shows significant progression (Fig. 4).
Discussion
The description for third ventriculostomy and biopsy for pineal region tumor was initially described in the 1970s. However, there was always fear of uncontrollable bleeding [19]. The efficacy of endoscopic management as an initial step for pineal region tumors presenting with hydrocephalus has been mentioned in several instances in the literature. The goals of endoscopic management are both CSF diversion and tissue diagnosis for further management.
In 2010, ETV success score (ETVSS) has been developed by Kulkarni et al. to estimate the prognosis of ETV [29] (Table 2). It is based on three parameters: the age of the patient, cause of hydrocephalus, and history of VPS. The patients were stratified according to the ETVSS in to high, moderate, and low ETVSS. The former showed a 3-year success rate of 72%, while moderate ETVSS showed a success rate of 52%. This has been validated in several pediatric articles; however, Labidi et al. have validated it in 2015 including adults’ age group [12, 30, 32, 46, 51].
The success score of patients with pineal region tumors in our series was from 80 to 90. This means that all cases were good candidates for initial ETV for the management of hydrocephalus. In our study, 6 out of 11 cases (54.5%) had successful ETV while the other 5 required VPS on their course of treatment despite having high ETVSS. In several other studies, the success rate of relief of hydrocephalus in cases where both ETV and biopsy were done ranged from 64 to 83%. However, Yamini et al. described that four out of six patients who had ETV required VPS later on. The authors stated that the reason for the high failure rate could be related to the presence of debris after biopsy acquisition [2, 11, 35, 55].
Recently, Gianaris et al. did a retrospective study in order to study causes of failure in cases with high ETVSS [23]. Fifty percent of cases in that study were either pineal tumors or tectal gliomas. He concluded from his series in patients with high ETVSS that the greater transependymal permeation and the smaller size of the third ventricle are related to better ETV outcome [23].
In our series, all 11 cases that had ETV had endoscopic biopsy, 2 of which had non-diagnostic tissue (18.2%). These cases included an anaplastic ependymoma, a pineoblastoma, and a germinoma. Yamini et al. in 2004 has analyzed 11 case series on 54 patients including his own series. In addition to the high failure rate of ETV when combined with biopsy, he stated that 89% of all cases had definitive histopathological diagnosis. His own series showed successful diagnosis in 67% of his cases [55]. In 2013, a review of the literature by Mottolese et al. stated that the accuracy of biopsy during ETV ranges between 61 and 100% [39]. Table 3 is showing a summary of all publications in the last 20 years related to ETV and biopsy.
The ETV failure rate in these studies ranged from 0 to 50%. The biopsy later failure rate was related either to technical difficulties while acquiring the biopsy or due to acquisition of insufficient or normal tissue. The biopsy failure rate range in these studies lies between 0 and 33%.
The most important possible complication from ETV is the injury to the basilar artery or its branches [1, 27, 36, 44, 49]. For this reason, some surgeons prefer to avoid ETV in cases that have diminished prepontine cistern [31]. However, some experienced neurosurgeons described that the size of the prepontine cistern should not be a contraindication, especially that up till now, no relationship has been established between the size of the prepontine cistern and the functionality of the ETV [48]. Apart from the failure of the ventriculostomy, we had only one case that had significant IVH and required EVD insertion post-operatively. In a review of literature, it was reported that the incidence of intraoperative hemorrhage or neurological deficit lies between 12 and 20% with no significant post-operative morbidity [39, 55]. Other reported complications include neurological deficit and infection.
In our series, we used a rigid endoscope and single trajectory with a burr hole 1 to 2.5 cm anterior to the coronal suture and 1.5 to 3 cm lateral to the midline. The optimum position of the burr hole was planned on preoperative sagittal MRI in each case. Despite this, we had only one complication of IVH and with no observed injuries of the fornix. In addition, our results were comparable to others as shown in Table 3. Morgenstern et al. had shown that there were no significant differences between single and two trajectories in their series [38]. Ahn and Goumnerova stated that the success rate of biopsy was lower when a flexible endoscope was used (45.5%) in comparison with the rigid endoscope (81%). That was technically related to the flexible biopsy forceps that has limited sampling capacity in comparison with that used in rigid endoscopes [2].
One of the important complications in this series is tumor dissemination. One of our cases (case 1) showed that tumor has disseminated through the stoma towards the interpeduncular and the prepontine cistern, the growth of which resulted in brain stem compression and death of the patient later on. This issue has been previously raised in the literature with a rate of spread that lies between 5 and 20% [25, 34].
A question has been also raised regarding the survival and occurrence of VPS complications post-ETV failure. Some authors have suggested that ETV could decrease the risk of VPS failure especially if it is associated with choroid plexus cauterization [21, 47]. Others have suggested that ETV may increase the risk of VPS infection. Warf and colleagues have done a retrospective study on data from 2329 patients in Uganda; they stratified patients into three groups. A group who had upfront VPS, another who had VPS inserted at the time of aborted ETV, and a third one who had VPS inserted after ETV failure. There were no significant differences observed across the three groups as regards obstruction, infection, and other complications [52].
Conclusion
Endoscopic third ventriculostomy and biopsy should be an initial step in the management algorithm for pineal region tumors. In our series, we were able to achieve this through a single trajectory and a rigid endoscope with results comparable to other studies in the literature. The success of the procedure can be measured by the biopsy and ETV failure rates. The former is related to the number and size of acquired samples. The later, although can be estimated by the ETVSS, still other factors such as biopsy acquisition at the time of ETV, intraventricular permeation, and preoperative ventricular size should be further studied for better capability of prognostication.
References
Abtin K, Thompson BG, Walker ML (1998) Basilar artery perforation as a complication of endoscopic third ventriculostomy. Pediatr Neurosurg 28:35–41
Ahn ES, Goumnerova L (2010) Endoscopic biopsy of brain tumors in children: diagnostic success and utility in guiding treatment strategies. J Neurosurg Pediatr 5:255–262. https://doi.org/10.3171/2009.10.PEDS09172
Al-Tamimi YZ, Bhargava D, Surash S, Ramirez RE, Novegno F, Crimmins DW, Tyagi AK, Chumas PD (2008) Endoscopic biopsy during third ventriculostomy in paediatric pineal region tumours. Childs Nerv Syst 24:1323–1326. https://doi.org/10.1007/s00381-008-0632-6
Balossier A, Blond S, Touzet G, Lefranc M, de Saint-Denis T, Maurage CA, Reyns N (2015) Endoscopic versus stereotactic procedure for pineal tumour biopsies: comparative review of the literature and learning from a 25-year experience. Neurochirurgie 61:146–154. https://doi.org/10.1016/j.neuchi.2014.06.002
Balossier A, Blond S, Reyns N (2016) Endoscopic versus stereotactic procedure for pineal tumor biopsies: focus on overall efficacy rate. World Neurosurg 92:223–228. https://doi.org/10.1016/j.wneu.2016.03.088
Bruce JN (2012) Management of pineal region tumors. In: Quinones-Hinjosa A (ed) Schimdek and sweet operative neurosurgical techniques: indications, methods and results, 6th edn. Elsevier, Philadelphia, pp 357–366
Chernov MF, Kamikawa S, Yamane F, Ishihara S, Kubo O, Hori T (2006) Neurofiberscopic biopsy of tumors of the pineal region and posterior third ventricle: indications, technique, complications, and results. Neurosurgery 59:267–277; discussion 267-277. https://doi.org/10.1227/01.NEU.0000223504.29243.0B
Chibbaro S, Di Rocco F, Makiese O, Reiss A, Poczos P, Mirone G, Servadei F, George B, Crafa P, Polivka M, Romano A (2012) Neuroendoscopic management of posterior third ventricle and pineal region tumors: technique, limitation, and possible complication avoidance. Neurosurg Rev 35:331–338; discussion 338-340. doi:https://doi.org/10.1007/s10143-011-0370-1
De Divitiis O (1998) Provision of a neuroendoscopy service. The Southampton experience. J Neurosurg Sci 42:137–143
Decq P, Le Guerinel C, Sakka L, Roujeau T, Sol J, Palfi S, Nguyen J (2000) Endoscopic surgery of third ventricle lesions. Neurochirurgie 46:286–294
Depreitere B, Dasi N, Rutka J, Dirks P, Drake J (2007) Endoscopic biopsy for intraventricular tumors in children. J Neurosurg 106:340–346. https://doi.org/10.3171/ped.2007.106.5.340
Durnford AJ, Kirkham FJ, Mathad N, Sparrow OC (2011) Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus: validation of a success score that predicts long-term outcome. J Neurosurg Pediatr 8:489–493. https://doi.org/10.3171/2011.8.PEDS1166
Ellenbogen RG, Moores LE (1997) Endoscopic management of a pineal and suprasellar germinoma with associated hydrocephalus: technical case report. Minim Invasive Neurosurg 40:13–15; discussion 16. https://doi.org/10.1055/s-2008-1053406
Ezzat S, Kamal M, El-Khateeb N, El-Beltagy M, Taha H, Refaat A, Awad M, Abouelnaga S, Zaghloul MS (2016) Pediatric brain tumors in a low/middle income country: does it differ from that in developed world? J Neuro-Oncol 126:371–376. https://doi.org/10.1007/s11060-015-1979-7
Ferrer E, Santamarta D, Garcia-Fructuoso G, Caral L, Rumia J (1997) Neuroendoscopic management of pineal region tumours. Acta Neurochir 139:12–20 discussion 20-11
Field M, Witham TF, Flickinger JC, Kondziolka D, Lunsford LD (2001) Comprehensive assessment of hemorrhage risks and outcomes after stereotactic brain biopsy. J Neurosurg 94:545–551. https://doi.org/10.3171/jns.2001.94.4.0545
Fiorindi A, Longatti P (2008) A restricted neuroendoscopic approach for pathological diagnosis of intraventricular and paraventricular tumours. Acta Neurochir 150:1235–1239. https://doi.org/10.1007/s00701-008-0155-7
Frappaz D, Conter CF, Szathmari A, Valsijevic A, Mottolese C (2015) The management of pineal tumors as a model for a multidisciplinary approach in neuro-oncology. Neurochirurgie 61:208–211. https://doi.org/10.1016/j.neuchi.2014.03.003
Fukushima T (1978) Endoscopic biopsy of intraventricular tumors with the use of a ventriculofiberscope. Neurosurgery 2:110–113
Gaab MR, Schroeder HW (1998) Neuroendoscopic approach to intraventricular lesions. J Neurosurg 88:496–505. https://doi.org/10.3171/jns.1998.88.3.0496
Gallo P, Szathmari A, De Biasi S, Mottolese C (2010) Endoscopic third ventriculostomy in obstructive infantile hydrocephalus: remarks about the so-called 'unsuccessful cases. Pediatr Neurosurg 46:435–441. https://doi.org/10.1159/000324913
Gangemi M, Maiuri F, Colella G, Buonamassa S (2001) Endoscopic surgery for pineal region tumors. Minim Invasive Neurosurg 44:70–73. https://doi.org/10.1055/s-2001-16002
Gianaris TJ, Nazar R, Middlebrook E, Gonda DD, Jea A, Fulkerson DH (2017) Failure of ETV in patients with the highest ETV success scores. J Neurosurg Pediatr 20:225–231. https://doi.org/10.3171/2016.7.PEDS1655
Haw C, Steinbok P (2001) Ventriculoscope tract recurrence after endoscopic biopsy of pineal germinoma. Pediatr Neurosurg 34:215–217. https://doi.org/10.1159/000056022
Hayashi N, Murai H, Ishihara S, Kitamura T, Miki T, Miwa T, Miyajima M, Nishiyama K, Ohira T, Ono S, Suzuki T, Takano S, Date I, Saeki N, Endo S (2011) Nationwide investigation of the current status of therapeutic neuroendoscopy for ventricular and paraventricular tumors in Japan. J Neurosurg 115:1147–1157. https://doi.org/10.3171/2011.7.JNS101976
Hirato J, Nakazato Y (2001) Pathology of pineal region tumors. J Neuro-Oncol 54:239–249
Horowitz M, Albright AL, Jungreis C, Levy EI, Stevenson K (2001) Endovascular management of a basilar artery false aneurysm secondary to endoscopic third ventriculostomy: case report. Neurosurgery 49:1461–1464 discussion 1464-1465
Kim IY, Jung S, Moon KS, Jung TY, Kang SS (2004) Neuronavigation-guided endoscopic surgery for pineal tumors with hydrocephalus. Minim Invasive Neurosurg 47:365–368. https://doi.org/10.1055/s-2004-830150
Kulkarni AV, Drake JM, Kestle JR, Mallucci CL, Sgouros S, Constantini S, Canadian Pediatric Neurosurgery Study G (2010) Predicting who will benefit from endoscopic third ventriculostomy compared with shunt insertion in childhood hydrocephalus using the ETV success score. J Neurosurg Pediatr 6:310–315. https://doi.org/10.3171/2010.8.PEDS103
Kulkarni AV, Riva-Cambrin J, Browd SR (2011) Use of the ETV success score to explain the variation in reported endoscopic third ventriculostomy success rates among published case series of childhood hydrocephalus. J Neurosurg Pediatr 7:143–146. https://doi.org/10.3171/2010.11.PEDS10296
Kunz M, Schulte-Altedorneburg G, Uhl E, Schmid-Elsaesser R, Scholler K, Zausinger S (2008) Three-dimensional constructive interference in steady-state magnetic resonance imaging in obstructive hydrocephalus: relevance for endoscopic third ventriculostomy and clinical results. J Neurosurg 109:931–938. https://doi.org/10.3171/JNS/2008/109/11/0931
Labidi M, Lavoie P, Lapointe G, Obaid S, Weil AG, Bojanowski MW, Turmel A (2015) Predicting success of endoscopic third ventriculostomy: validation of the ETV success score in a mixed population of adult and pediatric patients. J Neurosurg 123:1447–1455. https://doi.org/10.3171/2014.12.JNS141240
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Luther N, Stetler WR, Jr., Dunkel IJ, Christos PJ, Wellons JC, 3rd, Souweidane MM (2010) Subarachnoid dissemination of intraventricular tumors following simultaneous endoscopic biopsy and third ventriculostomy. J Neurosurg Pediatr 5:61–67. doi:https://doi.org/10.3171/2009.7.PEDS0971
Macarthur DC, Buxton N, Punt J, Vloeberghs M, Robertson IJ (2002) The role of neuroendoscopy in the management of brain tumours. Br J Neurosurg 16:465–470
McLaughlin MR, Wahlig JB, Kaufmann AM, Albright AL (1997) Traumatic basilar aneurysm after endoscopic third ventriculostomy: case report. Neurosurgery 41:1400–1403 discussion 1403-1404
Morgenstern PF, Osbun N, Schwartz TH, Greenfield JP, Tsiouris AJ, Souweidane MM (2011) Pineal region tumors: an optimal approach for simultaneous endoscopic third ventriculostomy and biopsy. Neurosurg Focus 30:E3. https://doi.org/10.3171/2011.2.FOCUS10301
Morgenstern PF, Souweidane MM (2013) Pineal region tumors: simultaneous endoscopic third ventriculostomy and tumor biopsy. World Neurosurg 79(S18):e19–e13. https://doi.org/10.1016/j.wneu.2012.02.020
Mottolese C, Szathamari A, Beuriat PA, Grassiot B, Simon E (2015) Neuroendoscopy and pineal tumors: a review of the literature and our considerations regarding its utility. Neurochirurgie 61:155–159. https://doi.org/10.1016/j.neuchi.2013.12.008
O'Brien DF, Hayhurst C, Pizer B, Mallucci CL (2006) Outcomes in patients undergoing single-trajectory endoscopic third ventriculostomy and endoscopic biopsy for midline tumors presenting with obstructive hydrocephalus. J Neurosurg 105:219–226. https://doi.org/10.3171/ped.2006.105.3.219
Oi S, Shibata M, Tominaga J, Honda Y, Shinoda M, Takei F, Tsugane R, Matsuzawa K, Sato O (2000) Efficacy of neuroendoscopic procedures in minimally invasive preferential management of pineal region tumors: a prospective study. J Neurosurg 93:245–253. https://doi.org/10.3171/jns.2000.93.2.0245
Ostrom QT, Gittleman H, Xu J, Kromer C, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS (2016) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2009-2013. Neuro-Oncology 18:v1–v75. https://doi.org/10.1093/neuonc/now207
Pople IK, Athanasiou TC, Sandeman DR, Coakham HB (2001) The role of endoscopic biopsy and third ventriculostomy in the management of pineal region tumours. Br J Neurosurg 15:305–311
Rezende MT, Spelle L, Piotin M, Mounayer C, Lucas Cde P, Abud DG, Moret J (2008) Selective endovascular treatment of a traumatic basilar aneurysm after endoscopic third ventriculostomy. Neuroradiology 50:443–446. https://doi.org/10.1007/s00234-007-0357-3
Robinson S, Cohen AR (1997) The role of neuroendoscopy in the treatment of pineal region tumors. Surg Neurol 48:360–365 discussion 365-367
Sacko O, Boetto S, Lauwers-Cances V, Dupuy M, Roux FE (2010) Endoscopic third ventriculostomy: outcome analysis in 368 procedures. J Neurosurg Pediatr 5:68–74. https://doi.org/10.3171/2009.8.PEDS08108
Shim KW, Kim DS, Choi JU (2008) Simultaneous endoscopic third ventriculostomy and ventriculoperitoneal shunt for infantile hydrocephalus. Childs Nerv Syst 24:443–451. https://doi.org/10.1007/s00381-007-0526-z
Souweidane MM, Morgenstern PF, Kang S, Tsiouris AJ, Roth J (2010) Endoscopic third ventriculostomy in patients with a diminished prepontine interval. J Neurosurg Pediatr 5:250–254. https://doi.org/10.3171/2009.10.PEDS09187
Vandertop PW (1998) Traumatic basilar aneurysm after endoscopic third ventriculostomy: case report. Neurosurgery 43:647–648
Villano JL, Propp JM, Porter KR, Stewart AK, Valyi-Nagy T, Li X, Engelhard HH, McCarthy BJ (2008) Malignant pineal germ-cell tumors: an analysis of cases from three tumor registries. Neuro-Oncology 10:121–130. https://doi.org/10.1215/15228517-2007-054
Warf BC, Mugamba J, Kulkarni AV (2010) Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus in Uganda: report of a scoring system that predicts success. J Neurosurg Pediatr 5:143–148. https://doi.org/10.3171/2009.9.PEDS09196
Warf BC, Bhai S, Kulkarni AV, Mugamba J (2012) Shunt survival after failed endoscopic treatment of hydrocephalus. J Neurosurg Pediatr 10:463–470. https://doi.org/10.3171/2012.9.PEDS1236
Wong TT, Ho DM, Chang KP, Yen SH, Guo WY, Chang FC, Liang ML, Pan HC, Chung WY (2005) Primary pediatric brain tumors: statistics of Taipei VGH, Taiwan (1975-2004). Cancer 104:2156–2167. https://doi.org/10.1002/cncr.21430
Wong TT, Chen HH, Liang ML, Yen YS, Chang FC (2011) Neuroendoscopy in the management of pineal tumors. Childs Nerv Syst 27:949–959. https://doi.org/10.1007/s00381-010-1325-5
Yamini B, Refai D, Rubin CM, Frim DM (2004) Initial endoscopic management of pineal region tumors and associated hydrocephalus: clinical series and literature review. J Neurosurg 100:437–441. https://doi.org/10.3171/ped.2004.100.5.0437
Yurtseven T, Ersahin Y, Demirtas E, Mutluer S (2003) Neuroendoscopic biopsy for intraventricular tumors. Minim Invasive Neurosurg 46:293–299. https://doi.org/10.1055/s-2003-44450
Zaazoue MA, Goumnerova LC (2016) Pineal region tumors: a simplified management scheme. Childs Nerv Syst 32:2041–2045. https://doi.org/10.1007/s00381-016-3157-4
Acknowledgements
The authors would like to express their deepest gratitude to Professor Yosry El-Adawy, professor of Neurosurgery, Alexandria University, for sharing his results and his scientific guidance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
For this type of study, formal consent is not required except for the illustrative cases.
Rights and permissions
About this article
Cite this article
Abbassy, M., Aref, K., Farhoud, A. et al. Outcome of single-trajectory rigid endoscopic third ventriculostomy and biopsy in the management algorithm of pineal region tumors: a case series and review of the literature. Childs Nerv Syst 34, 1335–1344 (2018). https://doi.org/10.1007/s00381-018-3840-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3840-8