Abstract
Purpose
The aim of this study was to investigate the incidence, clinical profiles, latency, and outcomes of radiotherapy (RT)-related intracranial aneurysms, rare but often fatal complications of cranial irradiation.
Methods
We reviewed all published individual patient data regardless of language, using survival analysis to make statistical inferences.
Results
We examined a total of 58 patients with RT-related intracranial aneurysms, including one unpublished case presented here, of whom 74.1 % presented with rupture. In the study, 29.3 % were younger than 18 years. The mean age at which patients received the first course of RT was 34.8 ± 22.8 years old. The mean latency between initiating RT and presenting with aneurysm was 10.4 ± 8.5 years. Rapid death ensured in 24 % shortly after presentation. The only significant predictor of death was rupture. In those with a single aneurysm, 43.1 % were located at the internal carotid artery, while 15.5 % of patients had multiple aneurysms. A male-to-female ratio of 1.87, 0.5, and 1.32 was found in patients younger than age 52, 52 years of age or older, and all 58 patients, respectively. Older age when receiving RT and presentation with ruptured aneurysm were significantly associated with shorter latency.
Conclusions
RT-related intracranial aneurysms presented differently from classical ones based on age, sex, site, multiplicity, and type. Sex ratios differed with age. The younger age group showed a longer latency of occurrence of an aneurysm. Older patients and those who develop ruptured aneurysms presented earlier. Since rupture may affect outcome, early detection of aneurysms before rupture may save lives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
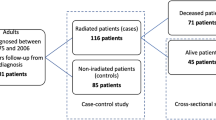
Radiotherapy(RT) effectively relieves symptoms and prolongs survival in many cancer patients, but cranial irradiation may also increase stroke risk in cancer survivors. The estimated relative risk of stroke and transient ischemic attack (TIA) in pediatric cancer patients ever treated with cranial RT is 8, with an incidence of 548/100,000 person-years [1]. Besides these toxicities, cranial irradiation also can cause lacunar lesions, vaso-occlusive diseases including moyamoya syndrome, vascular malformations including aneurysms, and hemorrhage [2]. Among these complications, aneurysm is very rare. The crude incidence can be estimated from single-institution retrospective chart reviews. The Ottawa Regional Cancer Clinic in Canada reviewed the data from 244 pediatric cancer patients who had received brain irradiation and found that postradiation cerebral vascular disease occurred in 11 (5 %) patients, one (0.4 %) of whom developed a ruptured aneurysm [3]. To the best of our knowledge, only 57 cases of postirradiation aneurysm have been published [4–51]. Of 529 pediatric brain tumor patients treated with RT between 1975 and 2004 at Taipei Veterans General Hospital (TVGH), Taipei, Taiwan, only one (0.19 %) developed an RT-related aneurysm [52]. To understand the characteristics of this rare complication and to analyze factors affecting the outcomes and latency of RT-related intracranial aneurysms, we performed a literature review of all patient data ever published describing intracranial aneurysms presenting in-field after cranial RT. One unpublished case from TVGH was added into the reviewed, published cases for statistical inference.
Materials and methods
The study followed the PRISMA guideline for meta-analyses [53]. We searched the PubMed, OVID, and Google Scholar databases using the keywords “aneurysm,” “radiotherapy,” “radiation,” and “RT,” including non-English language publications. Publications that did not provide the age at which RT was given were excluded. The date of last search was December 31, 2015. Two radiation oncologists reviewed the literature independently. Intracranial aneurysm(s) identified within prior radiation fields after cranial RT were deemed RT related, and the publications describing them, whether case series or single case reports, were included in the analysis. Data from patients that fulfilled the above criteria were pooled with an additional data from one unpublished case from the TVGH.
We set out to investigate the effect of all potential predictors on clinical outcomes and the latency between initiation of RT and presentation of intracranial aneurysm. We first performed univariate survival analysis for each factor, including age at first RT course, patient sex, cumulative conventional external beam RT (EBRT) dose, RT mode, aneurysm site, underlying diagnosis, type of aneurysm, whether the patient had ever received repeated RT or not, whether the aneurysm had ruptured or not, and the presence or absence of other clinical symptoms.
Conventional EBRT includes involved-field RT (IFRT) or whole-brain RT (WBRT) with a stated daily fraction size of 1.8–2.0 Gy as well as RT described as fractionated without an indication of fraction size. RT modes were categorized into hypofractionated EBRT, WBRT, conventional IFRT, brachytherapy, combined, and unknown. Patients who received more than one mode were listed as combined. Stereotactic radiosurgery (SRS), gamma knife radiosurgery (GKRS), and hypofractionated IFRT were all included in hypofractionated EBRT.
The mean cumulative dose for all patients was calculated, excluding SRS, hypofractionated radiotherapy, and brachytherapy, since their biological effects differ.
The sites of aneurysms were categorized as the internal carotid artery (ICA), anterior communicating artery (ACoA), posterior circulation (PC), multiple, and others. PC included the posterior cerebral artery (PCA), posterior communicating artery (PcoA), anterior inferior cerebellar artery (AICA), posterior inferior cerebellar artery (PICA), basilar artery (BA), and vertebral artery (VA). The categorization was based on our observation that the ICA, ACoA, PCoA, and PC might have a higher risk of rupture, while there were no solitary RT-related aneurysms reported over the PCoA [54, 55].
Given the high heterogeneity of diagnoses, patients were categorized only as nasopharyngeal carcinoma (NPC) or non-NPC patients. Types of aneurysm were categorized as saccular, fusiform, saccular and fusiform, giant, and dissecting. Those described as giant or with a diameter ≥25 mm were considered giant. Patients who received ˃1 course of RT were considered to have received repeated RT, but those receiving different RT modes within the same course of RT, e.g., brachytherapy after EBRT for patients with NPC, were not considered to have received repeated RT.
The significant predictor(s) in univariate analysis of the development of an aneurysm were included in multivariate Cox proportional hazard model. Potential predictors of aneurysmal fatality were analyzed by two-tailed Fisher’s exact test. To analyze the effect of menopause, we compared the sex ratios across the age of 52, while the median age of menopause in Western countries was 51.3 years [56]. All analyses were performed using SAS 9.3 software (Cary, NC). All p values less than 0.05 were considered significant, and no adjustments were made for multiple comparisons.
Results
Patient characteristics
Fifty-seven cases of RT-related intracranial aneurysm were found in 48 publications between 1984 and 2015. By combining these cases with one unpublished case from TVGH, individual patient data from 58 cases were analyzed. Characteristics of the patients and RT-related intracranial aneurysms are listed in Table 1.
Inferential statistics of the potential predictors and the results of univariate analysis for latency are listed in Table 2.
The mean latency between the first course of RT and presentation of radiotherapy-related intracranial aneurysm is 10.4 ± 8.5 years, with a median of 8.5 years. The mean ages of presenting with an aneurysm were 45.8 ± 20.6 years old, with a median of 52 years old. The mean cumulative dose of conventional EBRT was 66 ± 24 Gy, with a median dose of 59.4 Gy. Our study included 29.3 % pediatric patients who received RT at age 18 or younger. The mean age at the first course of RT was 34.8 ± 22.8 years old, with a median of 37.5 years old. In the study, the male-to-female ratio was 1.38 (25 men and 18 women) among those with ruptured aneurysms. The male-to-female ratio of all 58 patients was 1.32. By grouping the 58 patients in the present study into those less than 52 years of age versus 52 years of age or older, the sex ratios would be 1.87 and 0.5, respectively; multiple aneurysms were found in 15.5 % of the patients. For those presenting with a single aneurysm in the study, 43.1 % were located in the ICA. We also found that dissecting aneurysms were the most common type identified, accounting for 25.9 % of all cases.
Case presentation
A 17-year-old boy presented with sudden-onset left hemiplegia in January 2011. Emergency brain computerized tomography (CT) revealed intracranial hemorrhage (ICH) at the pons, with subarachnoid hemorrhage (SAH) at the circle of Willis and the pre-pontine cistern. There was no focal neurological sign except a fixed right pupil, 5–6 mm in size. No obvious increased intracranial pressure (IICP) signs nor hydrocephalus was observed to support placement of a ventriculoperitoneal (V-P) shunt. Angiography identified an arterial segment with an irregular lumen near the origin of the right AICA, compatible with a ruptured aneurysm, and another aneurysm at the right P1 section (from the termination of the BA to the PCA, within the interpeduncular cistern) of the PCA with a 1.8-mm sac and a 1.5-mm neck (Fig. 1). Coils were used to embolize the right AICA aneurysm. His symptoms, except for the left hemiparesis, improved after the embolization. This aneurysm was determined to be RT related, since the patient was extremely young for an aneurysm and the aneurysms were located outside the common sites of arterial branch points but within the radiation field and were dissecting in type.
The patient developed blood-tinged stool 15 months after the aneurysm ruptured. Sigmoidoscopy revealed a 1.5-cm polyp 20 cm from the anal verge. Polypectomy was performed, which identified signet ring cell adenocarcinoma.
He had a history of classic medulloblastoma with spinal seeding at the C6–7 level diagnosed at age 5. He underwent subtotal tumor resection in 1998. Subsequently, he received adjuvant chemotherapy with ifosfamide, cisplatin, and etoposide, followed by postoperative RT, including 5550 cGy in 34 fractions to the residual tumor, 4550 cGy in 29 fractions to the posterior fossa and C6–7 spinal canal, and 3150 cGy in 21 fractions to the craniospinal axis. After RT, chemotherapy continued for 1 year with 6 courses of intravenous ifosfamide, cisplatin, and etoposide and 10 courses of intrathecal nimustine hydrochloride (ACNU). Regular follow-up brain magnetic resonance imaging (MRI) through December 2010 was stable.
Both of his paternal grandparents died from strokes. His paternal grandfather’s stroke occurred in his sixth decade while his paternal grandmother’s occurred at the age of 40 and was rapidly fatal. There was no other family history of cerebral artery accident or cancer.
Statistical analysis
Fisher’s exact test revealed that the presence or absence of rupture at presentation was the only significant predictor of death shortly after aneurysm presentation with p = 0.047.
Univariate analysis identified age at first course of RT and whether or not the aneurysm had ruptured at presentation as the only two significant predictors for latency. These factors were included in a Cox proportional hazard model, and both were significant in multivariate regression (Table 3). An HR of 1.024 was noted for age. Increasing age at initiation of RT increased the chance of developing an intracranial aneurysm by approximately 2.4 % for each additional year in age, thus shortening the interval between RT and the presentation of RT-related aneurysm. The estimated HR for rupture as the presentation of RT-related aneurysm was 2.3, implying that those aneurysms that eventually rupture, compared with those that presented without rupture, i.e., that were identified by mass effect or follow-up imaging, were more likely to be identified and thus might be developed earlier after RT. As shown in Table 2, the mean latency between the first course of RT and RT-related aneurysm in those ruptured and not ruptured was 8.8 and 15.1 years, respectively.
The effect of age on aneurysm presenting with rupture was checked by mediation analysis (Table 4). The effects of age among models with rupture versus without rupture were similar (HR = 1.024 vs. 1.025), which indicated that the mediated effect of age in the path to rupture for aneurysm hazard is limited.
Discussion
In this study, we found RT-related intracranial aneurysms are different from classical ones in age, sex, multiplicity, site, and type. For classical aneurysms, the mean age of patients with aneurysmal subarachnoid hemorrhage is around 50 years [57]. The mean age of presentation of RT-related intracranial aneurysms is about 5 years younger. Male-to-female sex ratio of classical aneurysmal subarachnoid hemorrhage was found to be around 0.5 [58]. But a male dominance sex ratio was found in our study in RT-related intracranial aneurysms. Sex ratios reversed in elder patients. Multiplicity was found to be less frequent in RT-related than classical intracranial aneurysms, while multiple intracranial aneurysms, usually two or three in number, are found in 20–30 % of patients with classical aneurysms [57]. For those with a single lesion, our study found that RT-related intracranial aneurysm located at ICA about 6 times often than classical one [59]. Those with older age at receiving RT and presentation with aneurysmal rupturing had a shorter latency between RT and diagnosis of RT-related aneurysms with shorter latency. Rupture is the only predictor found to be associated with higher fatality after the diagnosis of RT-related aneurysm.
As a rare complication of RT, intracranial aneurysms were published mostly in forms of case reports or case series. This study is the first meta-analysis to investigate predictors of latency with multivariate analysis, to analyze predictor(s) of clinical outcome, and to investigate how age might affect sex ratios.
There are still many unknowns regarding the pathophysiology of this rare complication. Even in people without radiation exposure, little is known about the causes of intracranial aneurysms, although hypertension and smoking-induced vascular changes are thought to play a role [59]. Radiation causes cell death, induces inflammation, and damages arterial endothelial cells [60]. These effects might cause a decrease of the middle muscular layer of the artery, causing structural defects. Under hemodynamic shear force, an outpouching of the arterial wall is thus formed. Besides the direct insult of RT to the artery, indirect host factors, including obesity, metabolic syndrome, and atherosclerosis, may also contribute to aneurysm formation [61–64].
Early radiation exposure may explain the younger age at aneurysm presentation. The sex ratio appeared higher than that reported for classical intracranial aneurysms in younger patients but the same in older patients, perhaps related to a disturbance of sex hormones caused by irradiation to hypothalamus-pituitary axis [65].
The median radiation dose in patients with radiation-related intracranial aneurysms was nearly identical to the highest dose (60 Gy) generally prescribed for brain irradiation. Repeated RT did not shorten the interval of aneurysm presentation in univariate analysis (10 vs. 10.5 years) as in this study results. These findings imply that aneurysm development may be more due to individual conditions of the patients being treated rather than being caused by high RT doses. Several genetic conditions, including autosomal dominant polycystic kidney disease, fibromuscular dysplasia, Marfan’s syndrome, Ehlers-Danlos syndrome type IV, and AVM, are associated with the development of intracranial aneurysms [59]. Four patients with AVM and one with Ehlers-Danlos syndrome were identified in the literature review [11, 14, 20, 45]. Familial intracranial aneurysms are not rare, accounting for 7–20 % of patients with aneurysmal subarachnoid hemorrhage, and generally are not associated with any of the known heritable connective tissue disorders [66].
Regardless of a patient’s genetic predisposition, the RT dose still plays a role in aneurysm development: high doses of RT are more likely to cause intracranial aneurysms. Intrathecal gold isotopes (IT-Au) were administered together with EBRT in the 1960s to treat medulloblastoma, to increase the radiation dose in leptomeningeal sites. In a case series of 14 patients treated in this manner, six died of the disease while three of the remaining eight that survived more than 2 years developed ruptured intracranial aneurysms [67]. It was later learned that intrathecal isotopes tend to pool in the basal cisterns and cause radiation hot spots, which might explain the unusually high incidence of aneurysms in these patients. In contrast, our study did not show the association between the RT dose and the latency of the diagnosis of RT-related aneurysm. However, our study still found that those who received brachytherapy only, which would have delivered minimal radiation to adjacent arteries, presented with aneurysms later than those who received conventional IFRT.
Rupture of the aneurysm was a significant predictor for mortality from aneurysm. This suggests that early detection of RT-related aneurysms, prior to rupture, may save lives.
This study found that the latency between administration of RT and diagnosis of aneurysms was inversely proportional to age. Age per se has been recognized as a risk factor for aneurysmal rupture [54]. Other known risk factors, such as hypertension and smoking, may also be more prevalent in older patients. However, the increased risk of death with advancing age as a confounding factor, i.e., younger patients receiving cranial RT usually survive longer, may also contribute to this finding. Those with ruptured aneurysms presented sooner after RT. The chance of aneurysmal rupture thus decreases with time. The necessity to screen for intracranial aneurysms in patients who have received cranial RT may decrease years after treatment.
Limitation of the study
For this rare complication, we only were able to evaluate cases reported in the literature. Reporting bias is inevitable [68]. The actual RT doses to the involved arteries could not be evaluated, because the prescribed RT dose published typically is the dose given to the target volume rather than that of the affected artery. Evaluating biologically equivalent doses is difficult. The fraction size is often unavailable. Some publications did not provide the total dose of RT. The interval between repeated RT treatments is usually several years. There is no reliable way to sum up these treatments. For single fraction irradiation, brachytherapy, and IT-Au, there is also no generally accepted method to convert these treatments to biologically equivalent doses. More detailed analyses were not likely, since the known risk factors, such as hypertension, smoking, and menopause, were not described in the publications examined. The effect of chemotherapy could not be analyzed, since many of the searched articles did not indicate whether or not the patient received chemotherapy, although, from the history, we suspect some patients should have received it.
Conclusions
RT-related aneurysms present at a younger age, more frequently in the ICA, less frequently with multiplicity, more often in men, and more often with dissection, than classical aneurysms. The male-to-female ratio was significantly higher in younger patients. The only predictor for survival was whether or not the aneurysm presented with rupture. Early detection of RT-related aneurysms prior to rupture may save lives. Older age at treatment with RT and presentation with ruptured aneurysm were associated with a shorter latency. Follow-up imaging for aneurysm may be less necessary years after RT.
References
Campen CJ, Kranick SM, Kasner SE, Kessler SK, Zimmerman RA, Lustig R, et al. (2012) Cranial irradiation increases risk of stroke in pediatric brain tumor survivors. Stroke 43(11):3035–3040
Murphy ES, Xie H, Merchant TE, Jennifer SY, Chao ST, Suh JH (2015) Review of cranial radiotherapy-induced vasculopathy. J Neuro-Oncol 122(3):421–429
Keene DL, Johnston DL, Grimard L, Michaud J, Vassilyadi M, Ventureyra E (2006) Vascular complications of cranial radiation. Child Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg 22(6):547–555
Azzarelli B, Moore J, Gilmor R, Muller J, Edwards M, Mealey J (1984) Multiple fusiform intracranial aneurysms following curative radiation therapy for suprasellar germinoma. Case report. J Neurosurg 61(6):1141–1145
Gomori JM, Levy P, Weshler Z (1987) Radiation-induced aneurysm of the basilar artery—a case report. Angiology 38(2):147–150
Nishi T, Matsukado Y, Kodama T, Hiraki T (1987) Multiple intracranial aneurysms following radiation therapy for pituitary adenoma. Case report. Neurol Med Chir 27(3):224–228
Benson PJ, Sung JH (1989) Cerebral aneurysms following radiotherapy for medulloblastoma. J Neurosurg 70(4):545–550
Scodary DJ, Tew JM Jr, Thomas GM, Tomsick T, Liwnicz BH (1990) Radiation-induced cerebral aneurysms. Acta Neurochir 102(3–4):141–144
Thun F, Lanfermann H (1991) Intracranial giant aneurysm due to the effects of radiation. Radiologe 31(5):244–246
Moriyama T, Shigemori M, Hirohata Y, Konishi J, Tokunaga T, Kuramoto S (1992) Multiple intracranial aneurysms following radiation therapy for pituitary adenoma; a case report. No Shinkei Geka 20(4):487–492
Casey AT, Marsh HT, Uttley D (1993) Intracranial aneurysm formation following radiotherapy. Br J Neurosurg 7(5):575–579
John DG, Porter MJ, van Hasselt CA (1993) Beware bleeding from the ear. J Laryngol Otol 107(2):137–139
McConachie NS, Jacobson I (1994) Bilateral aneurysms of the cavernous internal carotid arteries following yttrium-90 implantation. Neuroradiology 36(8):611–613
Holodny AI, Deck M, Petito CK (1996) Induction and subsequent rupture of aneurysms of the circle of Willis after radiation therapy in Ehlers-Danlos syndrome: a plausible hypothesis. AJNR Am J Neuroradiol 17(2):226–232
Jensen FK, Wagner A (1997) Intracranial aneurysm following radiation therapy for medulloblastoma. A case report and review of the literature. Acta Radiol 38(1):37–42
Mak W, Chow T, Kwok S (2000) Radionecrosis of internal carotid artery in nasopharyngeal carcinoma presenting as epistasis. Aust N Z J Surg 70(3):237–238
Maruyama K, Mishima K, Saito N, Fujimaki T, Sasaki T, Kirino T (2000) Radiation-induced aneurysm and moyamoya vessels presenting with subarachnoid haemorrhage. Acta Neurochir 142(2):139–143
Aichholzer M, Gruber A, Haberler C, Bertalanffy A, Slavc I, Czech T (2001) Intracranial hemorrhage from an aneurysm encased in a pilocytic astrocytoma—case report and review of the literature. Child Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg 17(3):173–178
Cheng KM, Chan CM, Cheung YL, Chiu HM, Tang KW, Law CK (2001) Endovascular treatment of radiation-induced petrous internal carotid artery aneurysm presenting with acute haemorrhage. A report of two cases. Acta Neurochir 143(4):351–355 discussion 5-6
Huang PP, Kamiryo T, Nelson PK (2001) De novo aneurysm formation after stereotactic radiosurgery of a residual arteriovenous malformation: case report. AJNR Am J Neuroradiol 22(7):1346–1348
Lam HCK, Abdullah VJ, Wormald PJ, Van Hasselt CA (2001) Internal carotid artery hemorrhage after irradiation and osteoradionecrosis of the skull base. Otolaryngol Head Neck Surg 125(5):522–527
Aoki S, Hayashi N, Abe O, Shirouzu I, Ishigame K, Okubo T, et al. (2002) Radiation-induced arteritis: thickened wall with prominent enhancement on cranial MR images—report of five cases and comparison with 18 cases of moyamoya disease 1. Radiology 223(3):683–688
Murakami N, Tsukahara T, Toda H, Kawakami O, Hatano T (2002) Radiation-induced cerebral aneurysm successfully treated with endovascular coil embolization. Acta Neurochir Suppl 82:55–58
Pereira P, Cerejo A, Cruz J, Vaz R (2002) Intracranial aneurysm and vasculopathy after surgery and radiation therapy for craniopharyngioma: case report. Neurosurgery 50(4):885–887 discussion 7-8
Auyeung KM, Lui WM, Chow LC, Chan FL (2003) Massive epistaxis related to petrous carotid artery pseudoaneurysm after radiation therapy: emergency treatment with covered stent in two cases. Am J Neuroradiol 24(7):1449–1452
Louis E, Martin-Duverneuil N, Carpentier AF, Mayer JM, Delattre JY (2003) Radiation-induced aneurysm of the cavernous internal carotid artery. Rev Neurol 159(3):319–322 Anevrysme post-radique de la carotide intra-caverneuse
Chen H-C, Lin C-J, Jen Y-M, Juan C-J, Hsueh C-J, Lee J-C, et al. (2004) Ruptured internal carotid pseudoaneurysm in a nasopharyngeal carcinoma patient with skull base osteoradionecrosis. Otolaryngol Head Neck Surg 130(3):388–390
Gabriel CM, Stevens JC, Bremner F, Brew S, Plant GT (2004) Optic chiasm enhancement associated with giant aneurysm and yttrium treated pituitary adenoma. J Neurol Neurosurg Psychiatry 75(9):1343–1345
Yucesoy K, Feiz-Erfan I, Spetzler RF, Han PP, Coons S (2004) Anterior communicating artery aneurysm following radiation therapy for optic glioma: report of a case and review of the literature. Skull Base: Off J N Am Skull Base Soc [et al] 14(3):169–173
Lau WY, Chow CK (2005) Radiation-induced petrous internal carotid artery aneurysm. Ann Otol Rhinol Laryngol 114(12):939–940
Ghoshhajra BB, McLean GK, Foundation SIR (2006) SIR 2006 Annual Meeting Film Panel Case: radiation-induced cerebral aneurysms. J Vasc Interv Radiol: JVIR 17(12):1891–1896
Gonzales-Portillo GA, Valdivia JM (2006) Uncommon presentation of pediatric ruptured intracranial aneurysm after radiotherapy for retinoblastoma. Case report. Surg Neurol 65(4):391–395 discussion 5-6
Sciubba DM, Gallia GL, Recinos P, Garonzik IM, Clatterbuck RE (2006) Intracranial aneurysm following radiation therapy during childhood for a brain tumor. Case report and review of the literature. J Neurosurg 105(2 Suppl):134–139
Takao T, Fukuda M, Kawaguchi T, Nishino K, Ito Y, Tanaka R, et al. (2006) Ruptured intracranial aneurysm following gamma knife surgery for acoustic neuroma. Acta Neurochir 148(12):1317–1318 discussion 8
Cheng KY, Lee KW, Chiang FY, Ho KY, Kuo WR (2008) Rupture of radiation-induced internal carotid artery pseudoaneurysm in a patient with nasopharyngeal carcinoma—spontaneous occlusion of carotid artery due to long-term embolizing performance. Head Neck 30(8):1132–1135
Akamatsu Y, Sugawara T, Mikawa S, Saito A, Ono S, Takayama K, et al. (2009) Ruptured pseudoaneurysm following gamma knife surgery for a vestibular schwannoma: case report. J Neurosurg 110(3):543–546
Liu AK, Bagrosky B, Fenton LZ, Gaspar LE, Handler MH, McNatt SA, et al. (2009) Vascular abnormalities in pediatric craniopharyngioma patients treated with radiation therapy. Pediatr Blood Cancer 52(2):227–230
Park KY, Ahn JY, Lee JW, Chang JH, Huh SK (2009) De novo intracranial aneurysm formation after gamma knife radiosurgery for vestibular schwannoma. J Neurosurg 110(3):540–542
Yamaguchi S, Kato T, Takeda M, Ikeda H, Kitamura K (2009) Ruptured distal anterior inferior cerebellar artery aneurysm following stereotactic irradiation for vestibular schwannoma: case report. Neurol Med Chir 49(5):202–205
Pavlisa G, Rados M, Ozretic D, Pavlisa G (2010) Endovascular treatment of a ruptured radiation-induced aneurysm in a patient previously treated by Yttrium-90 brachytherapy. Acta Neurol Belg 110(3):276–278
Endo H, Fujimura M, Inoue T, Matsumoto Y, Ogawa Y, Kawagishi J, et al. (2011) Simultaneous occurrence of subarachnoid hemorrhage and epistaxis due to ruptured petrous internal carotid artery aneurysm: association with transsphenoidal surgery and radiation therapy—case report. Neurol Med Chir 51(3):226–229 English
Vogel TD, Kulwin CG, DeNardo AJ, Payner TD, Boaz JC, Fulkerson DH (2011) Tumor bleeding from a de novo aneurysm associated with optic glioma. J Neurosurg Pediatr 7(6):633–636
Yoon WS, Lee KS, Jeun SS, Hong YK (2011) De novo aneurysm after treatment of glioblastoma. J Korean Neurosurg Soc 50(5):457–459
Huh W, Bang JS, Oh CW, Kwon OK, Hwang G (2012) Intracranial aneurysm following cranial radiation therapy. J Cerebrovasc Endovasc Neurosurg 14(4):300–304
Gross BA, Ropper AE, Du R (2013) Vascular complications of stereotactic radiosurgery for arteriovenous malformations. Clin Neurol Neurosurg 115(6):713–717
Tamura M, Kogo K, Masuo O, Oura Y, Matsumoto H, Fujita K, et al. (2013) Formation and rupture of the internal carotid artery aneurysm after multiple courses of intensity-modulated radiation therapy for management of the skull base Ewing sarcoma/PNET: case report. J Neurol Surg Rep 74(2):111
Fujita K, Tamura M, Masuo O, Sasaki T, Yamoto T, Fukai J, et al. (2014) Ruptured internal carotid artery aneurysm presenting with catastrophic epistaxis after repeated stereotactic radiotherapies for anterior skull base tumor: case reports and review of the literature. J Neurol Surg Rep 75(2):e200
Gulati P, Bhattacharyya B, Deb S, Ghosh S (2014) Multiple intracranial aneurysms following radiation therapy for nasopharyngeal carcinoma. Indian J Neurosurg 3(1):44
Kellner CP, McDowell MM, Connolly ES, Sisti MB, Lavine SD (2014) Late onset aneurysm development following radiosurgical obliteration of a cerebellopontine angle meningioma. J Neurointerventional Surg. doi:10.1136/neurintsurg-2014-011206.rep
Nanney AD, El Tecle NE, El Ahmadieh TY, Daou MR, Ivan ENB, Marymont MH, et al. (2014) Intracranial aneurysms in previously irradiated fields: literature review and case report. World Neurosurg 81(3):511–519
Wu H, Guo L, Qiu Y, Yuan X (2014) Cavernous internal carotid artery aneurysm after radiotherapy presenting with external ophthalmoplegia. J Craniofac Surg 25(4):e380–e382
Yang K-L, Huang P-I, Wong T-T, Chang K-P, Wang L-W, Shiau C-Y, et al. (2010) Long-term outcomes of radiotherapy for primary pediatric brain tumors: statistics and strategies of a single institute in Taiwan. Ther Radiol Oncol 17(2):85–99
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269
Rinkel GJ, Djibuti M, Algra A, van Gijn J (1998) Prevalence and risk of rupture of intracranial aneurysms: a systematic review. Stroke; J Cereb Circ 29(1):251–256
Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, Hashimoto N, et al. (2012) The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med 366(26):2474–2482
Kato I, Toniolo P, Akhmedkhanov A, Koenig KL, Shore R, Zeleniuch-Jacquotte A (1998) Prospective study of factors influencing the onset of natural menopause. J Clin Epidemiol 51(12):1271–1276
Schievink WI (1997) Intracranial aneurysms. N Engl J Med 336(1):28–40
Group A (2000) Epidemiology of aneurysmal subarachnoid hemorrhage in Australia and New Zealand incidence and case fatality from the Australasian Cooperative Research on Subarachnoid Hemorrhage Study (ACROSS). Stroke; J Cereb Circ 31(8):1843–1850
Brisman JL, Song JK, Newell DW (2006) Cerebral aneurysms. N Engl J Med 355(9):928–939
Partap S ed (2012) Stroke and cerebrovascular complications in childhood cancer survivors. Semin Pediatr Neurol 19:18–24. Elsevier
Green DM, Cox CL, Zhu L, Krull KR, Srivastava DK, Stovall M, et al. (2011) Risk factors for obesity in adult survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. 30(3):246–255. doi:10.1200/JCO.2010.34.4267
De Haas EC, Oosting SF, Lefrandt JD, Wolffenbuttel BH, Sleijfer DT, Gietema JA (2010) The metabolic syndrome in cancer survivors. Lancet Oncol 11(2):193–203
Wong ND, Nelson JC, Granston T, Bertoni AG, Blumenthal RS, Carr JJ, et al. (2012) Metabolic syndrome, diabetes, and incidence and progression of coronary calcium: the multiethnic study of atherosclerosis study. J Am Coll Cardiol Img 5(4):358–366
McGill HC, McMahan CA, Herderick EE, Zieske AW, Malcom GT, Tracy RE, et al. (2002) Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation 105(23):2712–2718
Constine LS, Woolf PD, Cann D, Mick G, McCormick K, Raubertas RF, et al. (1993) Hypothalamic-pituitary dysfunction after radiation for brain tumors. N Engl J Med 328(2):87–94
Schievink WI (1997) Genetics of intracranial aneurysms. Neurosurgery 40(4):651–663
Pence DM, Kim TH, Levitt SH (1990) Aneurysm, arachnoiditis and intrathecal Au (gold). Int J Radiat Oncol Biol Phys 18(5):1001–1004
Abla AA, Lawton MT, McDermott MW (2014) Intracranial aneurysm formation following radiation. World Neurosurg 3(81):492–493
Acknowledgments
The authors are grateful for the financial support from grants of Taipei Veterans General Hospital (No: V103C-092, V104C-166 and V105C-152), Ministry of Science and Technology (MOST), R.O.C. (103-2314-B-075-MY3), Department of Health, R.O.C. (DOH102-TD-C-111-007), and partial research grant support from the charity Foundation of Mr. Chung-Yi Lee.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Wu, YH., Lin, SS., Chen, HH. et al. Radiotherapy-related intracranial aneurysm: case presentation of a 17-year male and a meta-analysis based on individual patient data. Childs Nerv Syst 32, 1641–1652 (2016). https://doi.org/10.1007/s00381-016-3144-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-016-3144-9