Abstract
Purpose
We aimed to present a practical three-dimensional (3D) printed simulator to comprehensively and effectively accelerate the learning curve of endoscopic endonasal transsphenoidal surgery (EETS).
Methods
The 3D printed simulator consists of three parts: (1) skull frame, (2) the nasal passage and the nasal alar of the face, and (3) a modified sella turcica. We aimed to improve three basic operational skills of surgeons: drilling, curetting, and aspirating. Eighteen neurosurgeons and five post-graduates were recruited and consented for the training.
Results
For trainees, (1) as the training progressed, the scores increased gradually, (2) a significant increase in the average scores was observed in the tenth training compared to the first training, and (3) there is a significant decrease in trainee variability in the shortening of the gap. The 18 neurosurgeons were divided into three groups: experts, assistants, and observers. For all three basic operations, (1) the average score of experts was obviously higher than that of the assistants, observers, and trainees’ tenth training and (2) the average scores of assistants and observers were obviously higher than that of trainees’ first training. A significant high in the average score between the assistants and the observers was seen for aspirating, but not for drilling or curetting. For curetting and aspirating, the tenth training average score of trainees was obviously higher than that of assistants and observers.
Conclusion
This 3D printed simulator allows different endoscopic basic operations to be simulated and improves the EETS techniques of surgeons. We believed it to be a practical, simple, and low-cost simulator.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since Jho and Carrau conducted pioneering work in endoscopic endonasal transsphenoidal surgery (EETS) in 1997 [1], the technique has developed rapidly and evolved from being used for removal of pituitary tumors to removal of other lesions of the parasellar region. Advocates of this technique note that it allows surgeons to resect adenomas more completely and safely due to its wide visualization and minimal invasiveness [2, 3].
However, the endoscopic technique presents a challenge for many surgeons, especially for younger surgeons. The deep location in the skull base, limited operative field, long pistol-grip surgical instruments, and dangerous anatomic structures require surgeons go through a steep learning curve [4]. Additionally, the opportunity of leading an EETS on patients is rare for younger surgeons due to the restriction of surgical seniority. Although some surgeons participate in operations as an assistant, most surgical operations are often still done by the attending surgeons.
Different types of training simulators for neurosurgery have been invented to allow additional surgical training [5]. However, there have been only few simulators for EETS, with disadvantages. Use of a cadaver [6] or virtual reality simulator [7] may be prohibitively expensive for many young surgeons, and animal models require animal sacrifice [8]. Some models just focused on improving the techniques of drilling [9, 10], and some lacked obvious validation [11]. In this study, we developed a practical three-dimensional (3D) printed simulator based on our combined endoscopic experiments of many years in multiple practices. We hope that this practical, simple, low-cost simulator is able to improve the basic operational skills of surgeons.
Methods
Simulator design
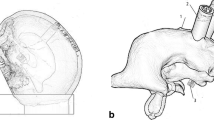
The 3D printed simulator, designed to target the practice of drilling, curetting, and aspirating, consisted of three parts: (1) skull frame, (2) the nasal passage and the nasal alar of the face, and (3) the modified sella turcica where eggs could be placed (Fig. 1). The geometry of the simulator originated from high-resolution CT scans of de-identified patients.
The 3D printed simulator. a Frontal view of the simulator. b The nasal alar of the face and septal cartilage were simulated with special flexible, elastomeric materials that allowed a certain degree of displacement. c Posterior view of the simulator. The sellar fossa was modified into a hole in the shape of an egg. d A thin plastic woven mesh was used to fix the eggs. Through these modifications, the eggs were allowed to be effectively inserted for each trial. e The main anatomy landmark of the nasal passage was constructed. a Inferior turbinate, b middle turbinate, c nasal septum, and d the open sellar floor. f Actual training on the simulator
The skull frame was manufactured using 3D printable thermal plastic, which allowed a realistic skeletal structure and a high level of durability. The nasal passage and the nasal alar of the face provided high-fidelity anatomical structures and realistic haptic feedback. The main anatomy landmark of the nasal passage was constructed including turbinate, nasal septum, nasal cavity, and naris. The nasal alar of the face and septal cartilage was simulated with special flexible, elastomeric materials that allowed a certain degree of displacement to create a realistic constraint to endoscope and other tool movement required during EETS. Considering both the one-nostril [2] and two-nostril [12] approaches of EETS, the posterior nasal septum was partly removed, allowing surgeons to choose the optimal approach.
As this simulator used eggs simulating pituitary adenomas with various textures, the sella turcica was made according to some modifications: (1) the anterior wall of the sphenoid and sellar floor was open, (2) the sellar fossa was modified into a hole in the shape of an egg, and (3) a thin plastic woven mesh was used to fix the eggs. Through these modifications, the eggs were allowed to be effectively inserted for each trial.
The egg had high anatomical similarity to a pituitary adenoma [11]. The egg shell simulated the sellar floor, the egg shell membrane simulated the dura mater, the egg albumen simulated the tumor, and the egg yolk simulated the normal pituitary. Through preliminary experiments, we found that after the eggs were boiled for 5 min, the egg yolk became slightly solid and there was a mild segregation between the egg shell and the shell membrane. These two characteristics provided a better surgical environment for aspirating and drilling. We also discovered that the texture of the egg albumen after being boiled for 15 min was similar to most pituitary adenomas and suitable for curetting.
Training criterion and validation
Eighteen neurosurgeons and five post-graduate without any experience in neurosurgical surgery were recruited and consented for the training. In an effort to validate the 3D printed simulator, an endoscopic experience questionnaire (Table 1) was designed and was administered to 18 neurosurgeons.
All training tools and equipment used were the same as those of the actual surgery, including endoscopes (4 mm, 30°), video recording system, diamond burr, ring curette, aspirator, and others. We used this simulator to improve three basic operational skills of the participants, and we assessed the subjects’ performance using a standardized set of objective scoring criterion.
Drilling
This training was defined as removing the thin and hard eggshell by a high-speed diamond burr without rupturing the fragile shell membrane. To calculate the removal area, each egg was attached with a self-adhesive label stock (2 mm× 2 mm2). The scoring criterion for drilling evaluation is described as follows: every participant was given 5 min for drilling. If the egg shell membrane was ruptured, the trial stopped and we recorded the operational time (T, s) and the area of drilling (S, mm2). The score = S + T / 300 × 20 (Fig. 2a, b).
Three basic operational trainings. a Thin and hard eggshell was removed by a high-speed diamond burr without rupturing the fragile shell membrane. b The fragile shell membrane was broken (arrow). c The egg albumen was removed by a ring curette without breaking the egg yolk. d The egg yolk was broken (arrow). e The egg albumen was aspirated by an aspirator without breaking the vitelline membrane. f The vitelline membrane was broken (arrow)
Curetting
This training was defined as removing the egg albumen by a ring curette without breaking the egg yolk. Every participant was given 5 min for the operation. If the egg yolk broke, the participant had to stop curetting and we recorded the operational time (T, s) and the curetted weight (W = full egg weight (F) − residual egg weight gram). The score = W/F × 100 + T / 300 s × 10 (Fig. 2c, d).
Aspirating
This training was defined as aspirating the egg albumen by aspirator without breaking the vitelline membrane. Every participant was given 5 min for the operation. If the vitelline membrane broke, the participant had to stop aspirating and we recorded the operational time (T, s) and the aspirated weight (W = full egg weight (F) − residual egg weight gram). The score = W/F × 100 + T / 300 s × 10 (Fig. 2e, f).
Statistical analyses were made using one-way ANOVA test, and all quantitative variables were described as averages with standard deviation (SD).
Results
Five post-graduates were considered as trainees. Eighteen neurosurgeons were divided into three groups according to the results of the questionnaire: five endoscopic experts, seven assistants who had experience only as an endoscopic assistant, and six observers who had only observed endoscopic surgery.
Trainees
As the training progressed, the scores of the five trainees increased (Fig. 3). For the first round of drilling, curetting, and aspirating, the average scores of the trainees were 51.9 ± 14.2, 11.3 ± 6.6, and 17.8 ± 4.8, respectively, and the average scores were 140.8 ± 9.7, 31.9 ± 2.6, and 44.9 ± 3.8, respectively, on the tenth training. The observed increase in the average scores was significant (Fig. 4).
There was a significant variability in the abilities of the trainees for all three basic operations. This variability was consistent for the first few trials, but after trial 5 or 6, this variability gradually decreased (Fig. 5).
Neurosurgeons
Experts, assistants, and observers were allowed only one time training for every basic operation. The average scores of the drilling were 205.6 ± 10.7, 120.1 ± 17.5, and 114.7 ± 8.1 for the experts, assistants, and observers, respectively; the average scores of the curetting were 43.2 + 4.0, 22.1 ± 1.7, and 21.9 ± 2.5, respectively; and the average scores of the aspirating were 58.7 ± 3.1, 31.3 ± 2.3, and 26.8 ± 1.8, respectively.
For the three basic operations, the average score of experts was obviously higher than that of assistants, observers, and trainees’ first training. A significant high in the average score between the assistants and the observers was seen for aspirating, but not for drilling or curetting (Fig. 6). For curetting and aspirating, the tenth training average score of trainees was obviously higher than that of assistants and observers. However, the tenth training average score of trainees was still lower than that of the experts for the three basic operations (Fig. 7).
Discussion
The 3D-printed simulator
The skill set required for minimally invasive endoscopic surgery is different from that required to perform open surgery [13]. The manipulation of instruments during these procedures is challenging due to the complex anatomy and proximity to important structures [14]. Therefore, EETS presents a steep learning curve for endoscopic skills [4] and training with simulators is a good method to accelerate this learning process [15, 16].
Varieties of simulators can be 3D printed or non-3D printed models. The non-3D printed models include animal, cadaveric, and virtual reality models. Animal models are useful in surgical training, but their low similarity to humans and ethical issues limit their application [17]. The use of a cadaver provides correct anatomic structure and better sensory feedback [9]. However, cadavers are expensive, require specialized and complicated preparation, and are toxic due to storing in formalin [18]. Although virtual reality models have been validated by many neurosurgical residents [7, 19], they are limited for widespread use due to high costs. The new-generation 3D printer allows the creation of neurosurgery simulators in a manner not previously possible. The 3D printed simulator possesses the characteristic of being high realistic, entirely reliable, easy to handle, and low in cost. Although 3D printing technology in neurosurgery is in the rapid developing phase, there are few reports of its application to EETS. There are two models that focus on improving the techniques of drilling [9, 10] and another simulator lacking the depiction of validations [11].
Therefore, we produced a practical simulator to improve the drilling, curetting, and aspirating skills of neurosurgeons. The main anatomy landmark of the nasal passage was accurately reproduced based on the high-resolution CT images from specific patients, which provided an actual EETS operating condition. Meanwhile, to reproduce the flexibility of the nasal passage and to mimic the degree of displacement caused by surgical instruments, we created the nasal alar of the face and septal cartilage from a special elastomeric material. The important unique innovation of this 3D printed simulator was the modified sella turcica: eggs could be well emplaced in the egg-shaped sellar fossa and were easily replaced as required for training.
Three basic operational skills
The procedure of EETS consists of nasal, sphenoidal, and sella stages. Each procedure is performed with different instruments and accomplished within a very limited operative field. Although EETS is considered to allow minimal invasiveness and high efficiency [20], the risk of adverse events and complications will be obviously increased with inexperience [21]. It is because each inexperienced operation has the potential to cause serious consequences that neurosurgeons must be proficient in every basic operational skill.
According to our endoscopic experiments of many years and in combination with multiple practices, holding the endoscope, drilling, curetting, and aspirating are the most important skills of EETS. Therefore, our simulator was designed and developed as a comprehensive training tool to practice these basic skills: (1) removing the eggshell by diamond burr to simulate opening the sphenoid sinus, (2) curetting the egg albumen by ring curette to simulate resecting a solid tumor, and (3) aspirating the egg albumen by aspirator to simulate resecting a cystic tumor. During observation of the training, we determined that other EETS skills including holding the endoscope would also be improved by training.
Training criterion
Surgeons must learn to resist surgical pressure. To simulate the pressure of surgery, the operational time was incorporated into the scoring criteria. Through a series of preliminary experiments and the analysis of training results, we determined that our objective scoring criterion is able to establish discriminant validity of this 3D printed simulator.
Evaluation of training validation
The score of five trainees went up in a curve, and there was a significant increase in the average scores from the tenth training compared with the first training. These indicate that the three basic skills of trainees were improved through training on our simulator. The different training curves also revealed that there were ups and downs in EETS training and that the progress of each surgeon occurred differently. Meanwhile, the score of five trainees went up not in a line but in a hectic curve. These indicate that surgeons may meet new trouble in different times training and they may be “down” sometimes. However, as a surgeon, they are able to resist surgical pressure and acquire new experience from failure.
During the first few trainings, evident variability in the ability to perform the three basic operations was noted. Presumably, this was caused by differences in individual ability. However, as the training progressed, the variability between trainees decreased and all trainees improved their proficiency. These data further illustrate that this 3D printed simulator was of wide suitability and high efficiency.
The average score of experts was obviously higher than those of the assistants and the observers in drilling, curetting, and aspirating. However, there was no obvious difference between assistants and observers in drilling and curetting. This may be attributed to the fact that the opportunity of leading an EETS on patients is scarce for assistants, while acquiring the endoscopic basic skills required not only a solid grasp of anatomic relationships, but also the actual psychomotor task of endoscopic tumor removal practice.
The scores of assistants were higher than those of the observers in drilling and curetting (although there was no statistical difference), and a statistically significant difference was witnessed in aspirating. This data demonstrated that although both participating in operations as an assistant and observing the operation by video allowed acquiring theoretical knowledge, working as an assistant did improve EETS operative skills, specifically improving the skills of aspirating.
The tenth training average score of trainees was still lower than that of experts for the three basic operations, and there was no statistical difference between trainees’ tenth training and assistant for drilling. These data illustrated that ten trainings might not be sufficient to reach the same level of skill. For all three basic operations, the average scores of assistants and observers were obviously higher than the first training average score of trainees. However, for curetting and aspirating, the tenth training average score of trainees was obviously higher than that of assistants and observers. These data demonstrated that although assistants and observers had previous EETS experience, they still needed practice and the training model presented here was a good choice.
Conclusions
This 3D printed simulator allows different endoscopic basic operations to be simulated and improves the EETS techniques of surgeons. We believed it to be a practical, simple, and low-cost simulator.
References
Jho HD, Carrau RL (1997) Endoscopic endonasal transsphenoidal surgery: experience with 50 patients. J Neurosurg 87:44–51
Oertel J, Gaab MR, Tschan CA, Linsler S (2015) Mononostril endoscopic transsphenoidal approach to sellar and peri-sellar lesions: personal experience and literature review. Br J Neurosurg 29:532–537
Linsler S, Gaab MR, Oertel J (2013) Endoscopic endonasal transsphenoidal approach to sellar lesions: a detailed account of our mononostril technique. J Neurol Surg Part B-Skull Base 74:146–154
Chi F, Wang Y, Lin Y, Ge J, Qiu Y, Guo L (2013) A learning curve of endoscopic transsphenoidal surgery for pituitary adenoma. J Craniofac Surg 24:2064–2067
Rehder R, Abd-El-Barr M, Hooten K, Weinstock P, Madsen JR, Cohen AR (2015) The role of simulation in neurosurgery. Child’s Nerv Syst ChNS: Off J Int Soc Pediatric Neurosurg 32:43–54
Olabe J, Olabe J, Sancho V (2009) Human cadaver brain infusion model for neurosurgical training. Surg Neurol 72:700–702
Rosseau G, Bailes J, del Maestro R, Cabral A, Choudhury N, Comas O, Debergue P, De Luca G, Hovdebo J, Jiang D, Laroche D, Neubauer A, Pazos V, Thibault F, Diraddo R (2013) The development of a virtual simulator for training neurosurgeons to perform and perfect endoscopic endonasal transsphenoidal surgery. Neurosurgery 73(Suppl 1):85–93
Jaimovich SG, Bailez M, Asprea M, Jaimovich R (2015) Neurosurgical training with simulators: a novel neuroendoscopy model. Child’s Nerv Syst ChNS Off J Int Soc Pediatric Neurosurg 32:345–349
Tai BL, Wang AC, Joseph JR, Wang PI, Sullivan SE, McKean EL, Shih AJ, Rooney DM (2015) A physical simulator for endoscopic endonasal drilling techniques: technical note. J Neurosurg 124:1–6
Okuda T, Yamashita J, Fujita M, Yoshioka H, Tasaki T, Kato A (2014) The chicken egg and skull model of endoscopic endonasal transsphenoidal surgery improves trainee drilling skills. Acta Neurochir 156:1403–1407
Okuda T, Kataoka K, Kato A (2010) Training in endoscopic endonasal transsphenoidal surgery using a skull model and eggs. Acta Neurochir 152:1801–1804
El-Fiki ME, Aly A, Elwany S (2012) Binasal endoscopic approach to the sellar region: experience and outcome analysis of 80 cases. J Neurol Surg B Skull Base 73:287–291
Arora H, Uribe J, Ralph W, Zeltsan M, Cuellar H, Gallagher A, Fried MP (2005) Assessment of construct validity of the endoscopic sinus surgery simulator. Arch Otolaryngol Head Neck Surg 131:217–221
Nogueira JF, Stamm AC, Lyra M, Balieiro FO, Leao FS (2008) Building a real endoscopic sinus and skull-base surgery simulator. Otolaryngol Head Neck Surg Off J Am Acad Otolaryngol Head Neck Surg 139:727–728
Satava RM (2010) Emerging trends that herald the future of surgical simulation. Surg Clin North Am 90:623–633
Selden NR, Origitano TC, Hadjipanayis C, Byrne R (2013) Model-based simulation for early neurosurgical learners. Neurosurgery 73(Suppl 1):15–24
Hayashi N, Kurimoto M, Hamada H, Kurosaki K, Endo S, Cohen AR (2008) Preparation of a simple and efficient laboratory model for training in neuroendoscopic procedures. Child’s Nerv Syst ChNS Off J Int Soc Pediatric Neurosurg 24:749–751
Filho FV, Coelho G, Cavalheiro S, Lyra M, Zymberg ST (2011) Quality assessment of a new surgical simulator for neuroendoscopic training. Neurosurg Focus 30:E17
Lemole M, Banerjee PP, Luciano C, Charbel F, Oh M (2009) Virtual ventriculostomy with ‘shifted ventricle’: neurosurgery resident surgical skill assessment using a high-fidelity haptic/graphic virtual reality simulator. Neurol Res 31:430–431
Bodhinayake I, Ottenhausen M, Mooney MA, Kesavabhotla K, Christos P, Schwarz JT, Boockvar JA (2014) Results and risk factors for recurrence following endoscopic endonasal transsphenoidal surgery for pituitary adenoma. Clin Neurol Neurosurg 119:75–79
Zador Z, Gnanalingham K (2013) Endoscopic transnasal approach to the pituitary—operative technique and nuances. Br J Neurosurg 27:718–726
Acknowledgments
We thank the teaching and research section of anatomy, Nanjing University, for technical support and equipment assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors have no support or funding to report.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Wen, G., Cong, Z., Liu, K. et al. A practical 3D printed simulator for endoscopic endonasal transsphenoidal surgery to improve basic operational skills. Childs Nerv Syst 32, 1109–1116 (2016). https://doi.org/10.1007/s00381-016-3051-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-016-3051-0