Abstract
Purpose
There are few papers in the literature comparing outcomes between antero-posterior and posterior-only approaches for treating thoracolumbar tuberculosis (T10–L2) in children
Methods
We performed a retrospective review of 47 children who were diagnosed and treated as thoracolumbar tuberculosis (T10–L2) in our department from January 2005 to June 2009. Forty-seven cases of thoracolumbar tuberculosis were treated by two different surgical approaches. All the cases were divided into two groups: 25 cases in group A underwent one-stage posterior debridement, transforaminal fusion, and instrumentation, and 22 cases in group B underwent anterior debridement, bone graft, and posterior instrumentation in a single- or two-stage procedure. Two approaches were compared in terms of average operative time, blood loss, hospitalizations, bony fusion, intraoperative and postoperative complications, the Oswestry disability index score, neurological status, and the angle of kyphosis.
Results
All 47 patients (24 M/23F), averaged 9.1 ± 2.6 years old (range 5 to 14 years), who were followed up for mean of 49.3 ± 8.6 months (range 36 to 65 months). Spinal tuberculosis (TB) was completely cured, and the grafted bones were fused in 9 months in all cases. It was obviously that the average operative time, blood loss, hospitalization, and complication rate of group A was less than those of group B. Good clinical outcomes were achieved in both groups.
Conclusions
Both the antero-posterior and posterior approaches can effectively heal T10–L2 vertebral tuberculosis, but the average surgical time, blood loss, complications, and hospital stay following the posterior approach are prominently less than those following the antero-posterior approach. It might be a better surgical treatment for thoracic spinal tuberculosis in children with poor health status, especially for cases in early phase of bone destruction and/or mild and moderate kyphosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The thoracolumbar junction (TLJ), which includes the T10–L2 region, is a common site for various spinal pathological processes including fracture, neoplasm, and infection. Thoracolumbar spinal lesions can result in neurological deficits, instability, and other adverse sequelae due to significant anterior compression of the neural tissue. Spinal tuberculosis (TB) is one of the most common severe spinal diseases that usually cause neurologic deficit, kyphotic deformity, and even spinal cord compression, especially in thoracolumbar, which is the most commonly affected site in spine (30 %) [1]. Thoracolumbar spinal tuberculosis in children—which is characterized as involving more vertebrae—causes severe kyphosis deformity, and spinal cord compression had the worst prognosis with the greatest deterioration during the active phase [2]. The aims of spinal tuberculosis treatment are to eradicate disease, to prevent the development of paraplegia and kyphotic deformity, to manage the existing deformity and neurological deficit, to allow early ambulation, and to return the patient back to daily life [3]. The therapeutic strategy for thoracolumbar tuberculosis in children includes conservative and operative treatments. Antituberculous chemotherapy is the mainstay of spinal TB treatment, but it has been found to be ineffective in preventing the progression of the deformity.
Various surgical treatments have been performed on children with spine tuberculosis: anterior, anterio-posterior, and posterior approach [4–9]. Currently, posterior instrumentation has become popular as a technique to correct angular deformities and stabilize an unstable spine. However, the posterior-only approach remains controversial because it may affect posterior spinal column stability [10, 11], especially the skeletal immaturity of children. In addition, thoracolumbar lesions—the junction region of thoracic lesions and lumbar lesions—had the highest propensity to develop morphological changes likely to predispose to deformity progression in children with spinal tuberculosis [12]. Severe kyphosis is more often a complication of childhood spinal tuberculosis than of adult disease [2, 13]. We found that there is a lack of clinical studies comparing the antero-posterior approach (AP) with the one-stage posterior-only approach (P). Therefore, this study aimed to review and compare the efficacy of the two approaches. Our study may be of benefit to the field.
Materials and methods
The study was approved by the ethics board committee of our hospital, and the written informed consent for participation in the study was obtained from children and their patients. This was a retrospective, clinical, comparative study. From February 2005 to July 2009, 47 children of the TLJ tuberculosis received surgical treatment. In group P (n = 25), the posterior-only approach was combined with debridement, transforaminal fusion, and instrumentation. The remainder (n = 22) received posterior internal fixation, anterior debridement, and fusion in a single- or two-stage procedure and were used as the control group (group AP). Detailed patient characteristics for the two groups were similar (Table 1). The diagnosis of TB spondylitis was based on clinical presentation, radiologic findings (plain radiograph, computed tomography, and magnetic resonance imaging), hematologic examination, and pathological examination. Erythrocyte sedimentation rate (ESR) was used to evaluate whether the lesion was active or the disease was healed. American Spinal Injury Association (ASIA) classification was used to assess the neurological compromise function. Clinical outcome was assessed preoperatively and at the last follow-up visit using the Oswestry disability index (ODI) questionnaire [14]. Kyphotic angle was measured by drawing two lines—one was along the top surface of the immediate upper normal vertebral body, and the other was away from the diseased segment. The bone fusion was assessed by the Moon standard
Preoperative management
Two to 4 weeks preoperatively, the most common antituberculous chemotherapy was a combination of isoniazid (5–10 mg/kg/day, with no more than 300 mg/day), rifampicin (5–10 mg/kg/day, with no more than 300 mg/day), and ethambutol (15 mg/kg/day, with no more than 500 mg/day). Chemotherapy was usually administered for 1 year after surgery on an outpatient basis. When the erythrocyte sedimentation rate (ESR) and temperature returned to normal or had significantly decreased and anemia and hypoproteinemia were rectified completely, surgery was performed. Children with progressive neurologic deficit received additional intravenous isoniazid (0.4 g/day) for 3 days preoperatively.
Surgical procedure
In group A, all patients were operated under general anesthesia in the prone position. Through posterior debridement, fusion and internal fixation were performed in a single stage [7]. The posterior spinal elements including lamina, facet joints, and transverse processes were exposed (extraperiosteal dissection) extending one vertebrae above and below the involved segments. Then, debridement and spinal cord decompression were performed (Fig. 1).
An 11-year-old boy was diagnosed as having tuberculous spondylitis after a 7-month history of severe back pain. The infection has been resistant to chemotherapy for 3 months. The destructive changes seen at L1–L2 on plain radiographs were progressive, and the lumbar kyphotic angle was 49.6 (a–d).The lesion around the vertebral body of L1–L2 developed a great abscess with marked bony destruction. The abscess involved into the spinal canal with cord compromise resulted in neurologic deficit. We performed one-stage posterior debridement, transforaminal lumbar interbody fusion, and instrumentation (e, f) from T11 to L3, the postoperative lumbar kyphotic angle became 8.0° (e, f). Follow-up MRI showing complete resolution of epidural abscess and decompression of neural component (g). Forty months after surgery, lateral radiographs show good bone fusion and maintenance of the correction (h, i)
In group B, firstly, posterior internal fixation without fusion was performed; then, anterior debridement and titanium mesh fusion were applied in single- or two-stage procedure, as described by Huang et al. [8] (Fig. 2).
An 5-year-old boy was diagnosed as having tuberculous spondylitis. The lesion around the vertebral body of L2–L3 developed a great abscess with marked bony destruction. We performed a posterior instrumentation from L1 to L4. Two weeks after the first operation, anterior debridement and allograft was performed on the patient (d, e). Three months after surgery, lateral radiographs show good bone fusion and maintenance of the correction (f). The X-ray found that the anterior infected site had healed and bony union was achieved at the final follow-up (g)
Postoperative procedure
The drainage tube was removed when the amount of drainage was less than 30 ml/day postoperatively. Patients were permitted to ambulate after remaining supine for 15 to 20 days postoperatively. We recommended that the bracing apparatus until bony fusion was observed on radiography. All children received antituberculous chemotherapy regimen for 12–18 months after the operation. Liver function and ESR rates were monitored carefully at regular intervals. Follow-up examinations were performed at 3 months, 6 months, 1 year, and last follow-up. Subsequent follow-ups were conducted at 12-month intervals. For the statistical analysis, chi-squared test and t tests were used, and a p value <0.05 was considered statistically significant.
Result
The mean duration of follow-up of all patients was 49.3 ± 8.6 months (range 36 to 65 months).
Operative results
Average operative time, amount of bleeding, and average time to stand for groups AP and P were 142.6 ± 29.5 vs 359.3. ± 96.2 min, 520.0 ± 180.3 vs 877.3 ± 123.2 ml, and 7.6 ± 1.3 vs 12.5 ± 2.5 days, respectively. Group P were obviously less than those of group AP (Table 1). The operative complication rate of group P was obviously less than those of group AP (Table 2). Wounds healed without chronic infection or sinus formation.
Radiographic results and laboratory examination
Preoperative, postoperative, and last follow-up of Cobb angles for groups P and AP were 38.1 ± 5.1° vs 41.2 ± 4.3°, 7.4 ± 1.3 vs 8.2 ± 1.4°, and 8.5 ± 1.5° vs 9.3 ± 1.0°, respectively. Bony fusion was achieved in both groups, with an average fusion time of 5 and 4 months, respectively. The mean correction loss was 1.2 ± 0.7° vs 1.0 ± 1.2°, respectively (Table 2). The ESR decreased gradually after surgery and returned to normal in all patients within 3 months.
Recovery of neurological functions
No neurological deterioration was recorded in any children postoperatively. There were 43 cases who suffered neurologic insults before surgery, most recovered after surgery. There were no significant differences in improvement rates in the ASIA classification (Table 2).
Clinical outcome
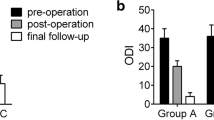
Mean ODI scores were 45.2 ± 2.9 vs 43.4 ± 3.5 before and 12.3 ± 3.4 vs 10.8 ± 3.5 after the operation for groups P and AP, respectively.
Discussion
Thoracolumbar lesions—the junction region of thoracic lesions and lumbar lesions—had the highest propensity to develop morphological changes likely to predispose to deformity progression in children with spinal tuberculosis [12]. Chemotherapy remains the mainstay in the management of children spinal TB, yet it cannot prevent the progression of kyphotic degeneration. Hence, timely and effective surgical intervention is essential. Indications for surgery are spinal instability, severe and/or progressive kyphosis, neurological deficit, no response to chemotherapy, and nondiagnostic and large paraspinal abscess [15]. In the clinic, however, there is still controversy over the strategy for thoracolumbar TB surgery. The thoracolumbar junction (T11–L2) poses an anatomical dilemma to spine surgeons during lateral approaches given the presence of the lower rib cage and the diaphragm, which is sandwiched between the pleura and peritoneum. Multiple surgical approaches have been described to access this area, from conventional anterior-only to more minimally invasive techniques: posterior-only as well as anterior-posterior approaches.
Generally, the lesion is usually located in anterior column; thus, anterior approach is considered better in view of decompression and fusion. However, the procedure may result in progression of kyphosis as a consequence of failure of the bone graft [16–19]. In children with spinal tuberculosis, anterior radical debridement destroys the anterior growth and limits the capacity for spinal remodeling, which leads to progressive kyphosis [20]. Also, this procedure has not been successful in preventing the progression of kyphosis or correcting the preexisting kyphosis [16, 18]. In view of this, an additional posterior instrumentation was applied by some surgeons [8, 10, 21–23] who have advocated this procedure. Its advantage lies in keeping the TB focus away from the instrument and fusion region, thus reducing the incidence of intraspinal infection. Also anterior abscess formation or multilevel involvement is essential, where an anterior debridement is mandatory. Even in cases of failure of union or reoccurrence in the tubercular focus region, the posterior fusion is not influenced, and the second stage revision surgery is comparatively easier [24]. Disadvantage of the AP approach are also obvious. The results of the present study demonstrate that with two positions and two incisions being used in the procedure, a longer operation time (359.3. ± 96.2 min), larger amount of bleeding (877.3 ± 123.2 ml), larger wounds, and prolonged bed rest (12.5 ± 2.5 days), the AP approach may not be tolerated by children <5 years who have a poor general state of health.
Currently, literatures on treating spinal tuberculosis in children by posterior procedure have been reported [7, 25–28]. However, Jain and Tuli [10, 11] consider that posterior approaches are unsafe because the posterior approach may destroy the healthy posterior spinal column, which may lead to spine instability. In addition, progression from thoracic kyphosis to lumber lordosis at T12 leads to transfer of weight from the posterior aspect to the anterior aspect of the spinal column which results in increased stress at this level. Moreover, many studies have shown a direct correlation between sagittal spine imbalance and severity of back pain [29, 30]. Posterior long-segment instrumentation, which is a rigid stabilization system, can provide better kyphosis correction and is beneficial to the stress dispersion which effectively prevents implant failure. Also, it can achieve relief of pain due to spinal instability. Meanwhile, a supplementary posterior short-segment fusion was applied to inhibit the overgrowth of posterior elements, which can balance the growth ratio between anterior height of fusion mass and posterior height of fusion mass and to prevent an increase in kyphosis during the growth period [12, 18, 31]. Lastly, reconstruction of spinal stability is beneficial to heal spinal tuberculosis and avoid recurrence [8].
In our middle-term follow-up results, although there was loss of correction in group P, the segmental stability of the spine was unaffected by this approach, which is consistent with the other efforts reported [7, 25–28]. The majority of patients achieved pronounced improvement in daily activities and neurologic deficits. Some scholars hold that the posterior approach could lead to intraspinal infection and central nervous system complications of TB infection, such as TB meningitis [25, 26]. In our research, this case did not happen, which is consistent with the other efforts reported [7, 25–28].
Posterior-only approach surgery provided adequate surgical space through resection of laminectomy, partial resection of the facet joints, and moderate stretch of nerve roots, at a 270° angle visualization for debridement, and the bony fusion 360° is also relatively fast. In this research, the rate and time of fusion in the two groups (4.8 ± 1.5 vs 6.4 ± 1.8 months) have no significant differences, which manifested that both groups achieved a reliable reconstruction of segmental stability.
In addition, minimally invasive surgery has become the direction of treatment for children’s spinal tuberculosis. The surgery wasn’t through thoracic cavity and mediastinum, as a result of the simple anatomical in the surgical approach. Through the posterior approach, debridement, fusion, and fixation can be accomplished simultaneously, and only one position and one incision are needed during operation. As a result, operation time is obviously reduced (142.6 ± 29.5 min), blood loss is decreased (520.0 ± 180.3 ml), and average time to stand is relatively short (7.6 ± 1.3 days). In our study, fewer complications happened in group P than in group AP, but this finding may be attributable to the small sample size. However, this approach can only be used with localized foci of no more than three levels and without extensive formation of abscesses. It is difficult to remove complete anterio-lateral debridement if the abscess is large and sticky [19].
Conclusion
Individualized treatment should be employed in treating TLJ tuberculosis. For carefully selected cases of thoracolumbar tuberculosis (T10–L2) in children, both approaches can successfully cure the disease. There were significant differences in operation time, blood loss, average time to stand, complications, or wound. Moreover, posterior-only approach alone cannot be used in cases of anterior abscess formation or multilevel involvement where an anterior debridement is mandatory.
References
Mankin HJ (2001) Tuberculosis of bone and joints: the Red King lives! Curr Opin Orthop 12:489–498
Rajasekaran S (2001) The natural history of post-tubercular kyphosis in children. Radiological signs which predict late increase in deformity. J Bone Joint Surg, Br Vol 83:954–962
Luk K (1999) Tuberculosis of the spine in the new millennium. Eur Spine J 8:338–345
Jeanneret B, Magerl F (1994) Treatment of osteomyelitis of the spine using percutaneous suction/irrigation and percutaneous external spinal fixation. J Spinal Disord Tech 7:185–205
Ozturk C, Aydinli U, Vural R, Sehirlioglu A, Mutlu M (2007) Simultaneous versus sequential one-stage combined anterior and posterior spinal surgery for spinal infections (outcomes and complications). Int Orthop 31:363–366
Oguz E, Sehirlioglu A, Altinmakas M, Ozturk C, Komurcu M, Solakoglu C, Vaccaro A (2008) A new classification and guide for surgical treatment of spinal tuberculosis. Int Orthop 32:127–133
Hong-Qi Z, Yu-Xiang W, Chao-Feng G, Jin-Yang L, Jian-Huang W, Jing C, Dai G, Ming-Xing T (2010) One-stage posterior approach and combined interbody and posterior fusion for thoracolumbar spinal tuberculosis with kyphosis in children. Orthopedics 33
Huang Q-S, Zheng C, Hu Y, Yin X, Xu H, Zhang G, Wang Q (2009) One-stage surgical management for children with spinal tuberculosis by anterior decompression and posterior instrumentation. Int Orthop 33:1385–1390
Jain S (2010) Comment on Huang et al.: one-stage surgical management for children with spinal tuberculosis by anterior decompression and posterior instrumentation. Int Orthop 34:769–770
Tuli S (2007) Tuberculosis of the spine: a historical review. Clin Orthop Relat Res 460:29–38
Jain A (2010) Tuberculosis of the spine a fresh look at an old disease. J Bone Joint Surg, Br Vol 92:905–913
Rajasekaran S, Shetty AP, Dheenadhayalan J, Reddy JS, Naresh-Babu J, Kishen T (2006) Morphological changes during growth in healed childhood spinal tuberculosis: a 15-year prospective study of 61 children treated with ambulatory chemotherapy. J Pediatr Orthop 26:716–724
Rajasekaran S (2002) The problem of deformity in spinal tuberculosis. Clin Orthop Relat Res 398:85–92
JCTDJ F, Couper J, O’Brien J (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
Sundararaj G, Behera S, Ravi V, Venkatesh K, Cherian V, Lee V (2003) Role of posterior stabilisation in the management of tuberculosis of the dorsal and lumbar spine. J BoneJoint Surg Br Vol 85:100–106
Rajasekaran S, Soundarapandian S (1989) Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Joint Surg 71:1314–1323
Alter AH (1973) Tuberculosis of the spine in children: Operative findings and results in one-hundred consecutive patients treated by removal of the lesion and anterior grafting: HL Bailey, M. Gabriel, AR Hodgson, and JS Shin. J Bone Joint Surg 54: A1633–1657 (December), 1972. J Pediatr Surg 8:567–568
Fountain S, Hsu L, Yau A, Hodgson A (1975) Progressive kyphosis following solid anterior spine fusion in children with tuberculosis of the spine. A long-term study. J Bone Joint Surg 57:1104–1107
Upadhyay S, Sell P, Saji M, Sell B, Leong J (1993) 17-year prospective study of surgical management of spinal tuberculosis in children: Hong Kong operation compared with debridement surgery for short- and long-term outcome of deformity. Spine 18:1704–1711
Schulitz K-P, Kothe R, Leong JC, Wehling P (1997) Growth changes of solidly fused kyphotic bloc after surgery for tuberculosis: comparison of four procedures. Spine 22:1150–1155
Hirakawa A, Miyamoto K, Masuda T, Fukuta S, Hosoe H, Iinuma N, Iwai C, Nishimoto H, Shimizu K (2010) Surgical outcome of 2-stage (posterior and anterior) surgical treatment using spinal instrumentation for tuberculous spondylitis. J Spinal Disord Tech 23:133–138
Kim D-J, Yun Y-H, Moon S-H, Riew KD (2004) Posterior instrumentation using compressive laminar hooks and anterior interbody arthrodesis for the treatment of tuberculosis of the lower lumbar spine. Spine 29:E275–E279
Fukuta S, Miyamoto K, Masuda T, Hosoe H, Kodama H, Nishimoto H, Sakaeda H, Shimizu K (2003) Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine 28:E302–E308
Klöckner C, Valencia R (2003) Sagittal alignment after anterior debridement and fusion with or without additional posterior instrumentation in the treatment of pyogenic and tuberculous spondylodiscitis. Spine 28:1036–1042
Rangel-Castilla L, Hwang SW, Whitehead WE, Curry DJ, Luerssen TG, Jea A (2012) Surgical treatment of thoracic Pott disease in a 3-year-old child, with vertebral column resection and posterior-only circumferential reconstruction of the spinal column: case report. J Neurosurg Pediatr 9:447–451
Pang X, Li D, Wang X, Shen X, Luo C, Xu Z, Zeng H, Wu P, Zhang P, Peng W (2014) Thoracolumbar spinal tuberculosis in children with severe post-tubercular kyphotic deformities treated by single-stage closing–opening wedge osteotomy: preliminary report a 4-year follow-up of 12 patients. Childs Nerv Syst 30:903–909
Sahoo MM, Mahapatra SK, Sethi GC, Dash SK (2012) Posterior-only approach surgery for fixation and decompression of thoracolumbar spinal tuberculosis: a retrospective study. J Spinal Disord Tech 25:E217–E223
Güzey FK, Emel E, Bas NS, Hacisalihoglu S, Seyithanoglu H, Karacor SE, Özkan N, Alatas I, Sel B (2005) Thoracic and lumbar tuberculous spondylitis treated by posterior debridement, graft placement, and instrumentation: a retrospective analysis in 19 cases. J Neurosurg Spine 3:450–458
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine 30:2024–2029
Roussouly P, Nnadi C (2010) Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 19:1824–1836
Jin D, Qu D, Chen J, Zhang H (2004) One-stage anterior interbody autografting and instrumentation in primary surgical management of thoracolumbar spinal tuberculosis. Eur Spine J 13:114–121
Acknowledgments
This work was financially supported by the National Natural Science Foundation of China (81271940) and the Project of Furong Scholar of Hunan Province.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interests concerning this paper.
Rights and permissions
About this article
Cite this article
Yin, X.H., Zhou, Z.H., Yu, H.G. et al. Comparison between the antero-posterior and posterior only approaches for treating thoracolumbar tuberculosis (T10-L2) with kyphosis in children: a minimum 3-year follow-up. Childs Nerv Syst 32, 127–133 (2016). https://doi.org/10.1007/s00381-015-2935-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2935-8