Abstract
Purpose
Abdominal cerebrospinal fluid (CSF) pseudocyst is a rare but important complication in patients with ventriculoperitoneal shunt (VPS). In addition to presenting our experience, we performed a comparative analysis between children and adults with this entity. To the author’s knowledge, there are no studies in which this condition has been compared.
Methods
The PubMed database was searched for all relevant reports published from 1954 to 2012. The differences were statistically compared, especially regarding clinical investigations, etiology of the hydrocephalus, shunt revision, CSF infection, treatment, and recurrence. Chi-square test or Fisher’s exact test was used to find associations among the variables.
Results
Compiled from literature, we found 393 cases of abdominal pseudocyst: 295 children, including our cases, and 55 adults, with age not informed in 43 cases. In children, 33 % of the patients have a positive culture on presentation, with higher incidence in children younger than 10 years. In contrast, only 15 % among adults were positive CSF culture. In total, 287 abdominal pseudocyst cases who underwent shunt revision have been reported; 78.4 % of children and 62.2 % of adults. The main occurrence of this complication according to the etiology of hydrocephalus in children was different from adults. The recurrence of pseudocyst occurred in 19.8 and 24.2 % of children and adults, respectively.
Conclusions
The differences between children and adults might represent distinct trends on the etiology and treatment of this entity. Hence, additional well-designed cohort studies will be necessary to strengthen our findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The modern ventriculoperitoneal shunt (VPS) era started in 1948 by Cone, Lewis, and Jackson [26, 52] and later by Ames, who between 1950 and 1957 performed several polyethylene tubing VPS with almost unsatisfactory results [6, 7]. Now, VPS is the standard therapy for the management of hydrocephalus. However, as more patients with hydrocephalus survive and live longer, more complications developed [59]. Approximately 5 to 47 % of abdominal complications by VPS are reported [44, 71]. One of the less frequent but important complications is the abdominal CSF pseudocyst, with a reported rate of less than 1 % on all patients with shunt [14], although higher rates were reported as well [94]. Even more uncommon are hepatic [37, 62, 65, 66, 85, 95, 110] or splenic pseudocyst as a complication of VPS insertion [72].
The cyst is called pseudocyst because its walls consists only of peritoneal serous membrane, thickened by a chronic inflammatory process [18, 70]. The invasion of lymphocytes in the specimen may have suggested that the inflammatory reaction to the shunt tube was associated with cyst formation [80]. We agree with others who prefer the term “abdominal pseudocyst” [31, 84, 94, 98, 103, 105] rather than peritoneal [14, 18, 45, 52], intraperitoneal [75], or omental cyst [41].
The aim of this paper was to report a comparative analysis between children and adults with abdominal CSF pseudocyst on the clinical presentation, etiology of the hydrocephalus, rate of CSF infection and shunt revision, treatment, and results on the literature of the last 58 years. In this review, we have included five new cases treated at our institution (Figs. 1 and 2).
Methods
An analysis of the 502 shunt placement procedures performed for an 8-year period (January 2005 to December 2012) at our hospital, revealed that five patients developed abdominal CSF pseudocyst. Details of history, clinical features, radiological finding, cerebrospinal and abdominal CSF pseudocyst culture, and clinical outcomes were summarized (Table 1). In addition, the information for this review was retrieved from the author’s files and the National Library of Medicine database (PubMed) for the period 1954–2012 using the following keywords: “intra-abdominal pseudocyst”, “cerebrospinal fluid pseudocyst”, “abdominal cerebrospinal fluid pseudocyst”, “peritoneal pseudocyst”, “intraperitoneal pseudocyst”, “omental cyst”, “shunt infection”, and “shunt complications.” In total, 100 articles of case–control studies, case reports, and case series were included in our revision (Table 2).
Our reviewed included 393 cases of abdominal pseudocyst related to the use of VPS. Because of the possible difference between children and adults, the analysis was performed for each subgroup, considering individuals younger than 19 years as children and individuals older than 19 years as adults. Chi-square test or Fisher’s exact test was used to find associations among the variables and verified the odds ratio for recurrence related to the etiology of hydrocephalus, CSF infection and surgical treatment. The Stata software version 13.0 (Copyright 1985–2013; Stata Corp. LP, College Station, TX) was used for statistical analysis. A p value < 0.05 was considered significant.
Discussion
Epidemiology
Since Harsh [54] described in 1954 a periumbilical cyst associated among 12 ventriculofallopian shunts and Jackson and Snodgrass [60] also reported another case 1 year later, large series were published in the world literature [14, 36, 42, 52, 53, 63, 74, 94, 98], some of them in Latin America [31, 38, 102]. Our literature review included a total of 100 articles, including five cases of the current study, totaling 393 cases of abdominal CSF pseudocyst since the first case reported by Harsh [54] (Table 2). According to several authors, this condition accounted for approximately 0.25 to 10 % of all VPS [11, 14, 18, 36, 52, 71, 74, 94, 103]. In our series, abdominal pseudocyst formation represents only 1 % of all patients with VPS (5/502). However, the prevalence rate found in 21 case–control studies, including our study, recompiled from the literature was 2.3 % of the cases based on the total of patients evaluated, that is, 10,803 controls with 183 cases [4, 10, 11, 14, 18, 29, 33, 36, 49, 52, 53, 60, 71, 74, 90, 91, 94, 101, 103, 108].
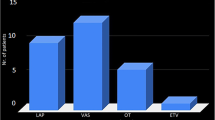
Many authors have reported this complication in pediatric patients because hydrocephalus is more common in children. However, in a series, the child–adult ratio was 1.8:1 [94]. According to this survey, 295 children, including our cases, and 55 adults have been reported until 2012; age was not provided in 43 cases (Fig. 3). There are reports of abdominal CSF pseudocyst in a 75-year-old man and an 84-year-old woman [100, 109]; on the other hand, one of the youngest patients was 2 months old [94, 102]. In children, our study identified 48.2 % males and 51.8 % females, and among adults, 43 % males and 57 % females. We found a mean age of 7.2 ± 4.7 years in children; 80 % of the cases were younger than 10 years, and only 20 % were children between 10 and 19 years old. In adults, the mean age was 36.7 ± 15.1 years. We observed a proportion of 47.3 % of the cases for adults 30 years and younger and 52.7 % for adults older than 30 years (Table 3).
Histogram of age between a children and b adults. Distribution of age among children, showing that the vast majority of the sample had children younger than 10 years, 13 % had younger than 1 year, and only 4.4 % had 15–19 years old. Among adults, we observed a right-skewed distribution, showing that most individuals were 20 to 25 years (25.5 %) and 20 % were older than 45 years
Predisposing factors
Although the etiology of abdominal CSF pseudocyst is not clear, different authors attribute cyst formation to several predisposing factors, with no clinical or scientific support. The most frequent factor is the inflammatory process, either sterile or infectious. In some patients, it could be an inflammatory response to some components of the shunting system or to a high concentration of protein in the peritoneal cavity [2, 28, 30], associated sometimes with an antigen–antibody reaction by an unidentified protein moiety in the CSF [8]. This hypothesis would explain the cases of abdominal pseudocyst in which CSF culture proved negative. Other predisposing causes are as follows: (a) prior abdominal surgeries or multiple revisions of the shunt in the abdomen; (b) allergic reactions to silicone or ethylene oxide [55] and a reaction due to the starch granules from the surgical gloves; for this reason, some neurosurgeons recommend the use of latex-free gloves while inserting a VPS or excising pseudocyst [103]; and (c) in a lesser proportion, liver dysfunction [67].
Most authors agree that infection is the main cause of the formation of abdominal CSF pseudocyst [18, 33, 73]. One paper reviewed eight studies with 128 cases showing that infection rates vary between 17 and 80 %, with an average of 42 % [74]. Some neurosurgeons recommend a routine culture of the abdominal catheter tip. In the series of Salomão et al. [102], cultures of the CSF and the tip were positive in 44.4 and 61 % of the samples, respectively. In their opinion, the latter seems to be more reliable. The most common organisms isolated from the culture are Staphylococcus epidermidis and Staphylococcus aureus. According to Erşahin et al. [36], when the abdominal CSF pseudocyst associated with a shunt infection occurs within 1 year after a shunting procedure, the probable organism is S. epidermidis. Mobley et al. [74] stated that it is possible to find slow-growing bacteria such as P. acnes in culture more than 7 days. Some few isolated cases of infected abdominal CSF pseudocyst with others bacteria have been reported [36, 56, 63, 74, 102]. In contrast, similar to our five cases, Bartolek et al. [11] did not find infection signs in their five patients, nor did Sena et al. [105] and Agha et al. [4].
In our analysis of 295 pediatric cases, 92 patients (33 %) have a positive culture on presentation, 188 cases (67 %) have sterile CSF, and 15 children have infection as missing data. The positive culture rate was 41 % for those 5 years and younger, 39 % for children between 5 and 10 years old, 16 % for patients between 10 and 15 years old, and only 4 % positive culture for those 15 years and older. In contrast, only 6 cases (15 %) among 41 adults were infected. The positive culture rate was 66 % for those 30 years and younger. The other 14 adults were not informed of the CSF culture. This information confirms that the prevalence of infection is lower in adults than that in children and shows a higher prevalence in children younger than 10 years (p = 0.042) and in adults younger than 30 years (p = 0.355). Furthermore, some authors suggest that a smaller pseudocyst tends to be infected and a larger abdominal CSF pseudocyst tends to be sterile [46, 84].
One of the most suggested predisposing factors of CSF pseudocyst formation is multiple shunt revisions. Hahn et al. [53] found that the average number of previous shunt revisions in patients with abdominal CSF pseudocyst was 11.2, and Rainov et al. [94] described 50 % of the patients with 5 to 10 shunt revisions. This revision rate is significantly higher compared with our cases and other reports [18, 31, 36, 42, 102].
In total, 287 abdominal CSF pseudocyst cases who underwent shunt revision have been reported; 196 (78.4 %) of 250 children and 23 (62.2 %) of 37 adults evaluated were submitted to VPS revision. In children, of the 196 patients who had at least one shunt revision, 68 (35 %) had positive cultures on presentation. On the other hand, of the 54 patients who did not have a revision, only 12 (22 %) had an infection (p = 0.09). In contrast, of the six adult patients reported with positive CSF culture, two had previous shunt revision (2/19), 2 had not underwent shunt revision (2/12), and the other two were not informed history of VPS revision (2/6) (p = 0.507). Comparing adults and children, we found an association between shunt revision and positive cultures (p = 0.017), suggesting that children who had a previous shunt revision had the most positive cultures compared with adults, with an odds ratio of 1.84.
Additionally, the etiology of the hydrocephalus has been thought to predispose the development of abdominal pseudocyst. Gutiérrez and Raimondi [52] observed the high incidence of abdominal CSF pseudocyst in patients with Dandy-Walker cyst (4 of 11). Likewise, myelomeningocele seemed to be an important etiology factor for pseudocyst formation in de Oliveira’s [31] series (6 of 12). Central nervous system (CNS) tumors have been associated with this pathology, such as astrocytomas, meningioma, papilloma of plexus choroideus, ependymoma, and primitive neuroectodermal tumors [9, 11, 20, 23, 30, 62, 95, 106, 115, 116].
In international literature, the most common etiology-related hydrocephalus in children was congenital hydrocephalus (21.7 %), followed by myelomeningocele (19.3 %), intraventricular hemorrhage in premature infants (14.6 %), brain tumor (7.8 %), and meningitis (7.8 %). On adult patients, the main causes of hydrocephalus included tumor (21.8 %), meningitis (16.3 %), intraventricular hemorrhage (11.3 %), trauma (7.2 %), and congenital hydrocephalus (5.5 %) (Table 3). Although 21 and 19 % of children had congenital hydrocephalus and myelomeningocele, respectively, these diagnoses do not represent predisposition to positive CSF cultures (p = 0.421 for congenital hydrocephalus and p = 0.325 for myelomeningocele). On the other hand, almost 22 and 16 % of the adults had brain tumor and meningitis, respectively, as a main cause of hydrocephalus. Of the adult cases with negative culture, 34 and 20 % had brain tumor and meningitis, respectively, as opposed to none of the adults with these conditions had infection (p = 0.106 for brain tumor and p = 0.299 for meningitis). Hence, the etiology of hydrocephalus has not seemed to be a risk factor in the development of abdominal CSF pseudocyst in either children or adults.
Clinical aspects
Although there are no pathognomonic signs in patients with abdominal CSF pseudocyst, the common presentations in children are headache, vomiting, and decreased level of consciousness [94]. Moreover, this pathology may be presented as an acute abdomen [117]; therefore, this presentation in children with VPS requires a skillful diagnostic workup [92, 97]. In adults, the abdominal signs are more important than the infectious signs or neurological complaints, which usually appear days or weeks after abdominal symptoms [42, 77]. Ohba et al. [80] found abdominal symptoms in most of the adult cases, where approximately 30 % presented with symptoms because of shunt malfunction. In abdominal CSF pseudocyst has been also described hyponatremic seizure, hydronephrosis, inferior vena caval obstruction with bilateral hydronephrosis, ureteropelvic junction obstruction, caliectasis with both ureters deviated laterally, cholelithiasis, suggestive of a full-term pregnancy, hemorrhage as a complication of anticoagulant therapy, markedly elevated liver function test, and a right pleural effusion [19, 35, 47, 48, 57, 67, 69, 88, 89, 111].
In our series, three patients (60 %) had shunt dysfunction. However, in literature revision, the neurological symptoms occurred only in 38.6 % of the children and 34.6 % of the adults. Hence, there was no tendency toward presentation with neurological symptoms in the children compared with the adults (p = 0.569, chi-square test). On the other hand, abdominal symptoms were more frequent, representing 89 % of the sample, with 89.9 % in children and 83.6 % in adults. Hence, there was no tendency toward presentation, with abdominal symptoms compared in both groups (p = 0.184, chi-square test). However, to determine the association between the types of symptoms assessed, we identified 35 % of children with both abdominal and neurological symptomatology (p = 0.000) and 24 % of adults (p = 0.000), demonstrating that the association of abdominal and neurological symptoms was obtained for children and adults.
The time interval from the shunt application to the onset of symptoms had a mean of approximately 2 years [18], but frequently within the first 6 months [108]. The shortest interval was 5 days in one patient [24] and 6 days in other patients [52]. The longest interval was 10 years [99, 105] and 15 years [31, 87]. The length of time from the last shunting procedure to the development of abdominal CSF pseudocyst in our series ranged from 6 months to 5.9 years (mean 2.6 years). The fact that abdominal CSF pseudocyst occurs within a short amount of time after a shunt revision implies that an infectious state is probably present, despite the low infection rates published in the literature.
Diagnosis
For radiological diagnosis, ultrasound is the method of choice because it is noninvasive, easy to perform, not expensive, and sufficient for a satisfactory diagnosis for larger, localized, or loculated abdominal CSF collection, and generally, it can be displaced in the tip of the peritoneal catheter [7, 42]. Grunebaum et al. [50] drew attention to the sonographic signs of the noninfected pseudocyst, infected pseudocyst, or abscess. For these authors, the noninfected abdominal CSF pseudocyst is characterized by a well-defined sonolucent mass without septa and increased echogenicity beneath it. The shunt tip will produce and echo a signal of higher amplitude than a septum, and the two parallel sides of the shunt will produce the characteristic “railroad sign”. In an infected abdominal pseudocyst, a mixture of echoes is demonstrated. The presence of septa or even a fluid level may be detected [93].
The CT scan of the abdomen provides a more accurate diagnosis, especially when these abdominal CSF pseudocysts are large and deform the normal architecture of the abdomen [43]. CT scan may be a better first choice in the initial evaluation to exclude other causes such as peritonitis, appendicitis, volvulus, or diverticulitis [8]. The CT scan shows a cyst containing homogeneous water density fluid with a fine and well-defined margin. The distal catheter of the shunt appears as a higher-density structure with the tip within the pseudocyst [91]. Our patients were diagnosed based on CT scan and reflect the trend for using it as the basis for evaluation, especially when there is a suspected mass.
Treatment
On the basis of treatment, there has been no consensus for both handling the VPS as pseudocyst itself because of the treatment changes according to the characteristics of patients, the experience of the surgeon, and the findings during the operation [104]. All patients with abdominal pseudocyst must have CSF from the shunt, the pseudocyst, or both preoperatively. When the CSF is positive for bacteria on Gram stain or had a suspicious glucose, protein, or white blood cell count, the treatment tends to be an externalization of the shunt and proper antibiotic therapy [74].
In the absence of infection, the most widely accepted opinions are replacement of the distal catheter into the nonperitoneal space, especially if there are signs of peritonitis and peritoneal adhesions or laparotomy for catheter replacement in the opposite quadrant of abdomen pseudocyst. Therefore, removing the peritoneal shunt entirely became preferable [31, 103]. Although an acute infection may not be evident, prophylactic antibiotic therapy is warranted until infection is ruled out [8].
About the treatment of pseudocyst, some authors propose full or partial exeresis by laparotomy or laparoscopy, especially if the large cavity is attached to the abdominal wall [76]. Some surgeons had demonstrated that the simple remotion of the catheter diverted the CSF, making the pseudocyst disappear [42]. Sonographically guided abdominal CSF pseudocyst aspiration is also an effective technique, allowing the exclusion or confirmation of CSF infection and providing the relief of abdominal symptoms [25, 93]. If there is no sign of infection, a single operative shunt revision may be a reasonable and less invasive method of treatment, sparing the patient a surgical procedure and shunt externalization [25].
In summary, the most common definitive procedures in children and adults include seven main categories: (1) direct exploratory laparotomy or laparoscopic procedure with abdominal pseudocyst excision or aspiration and (a) reposition of the distal shunt into the opposite site of peritoneum, (b) replacement of the distal shunt, and/or (c) reposition of the distal catheter into the nonperitoneal space; (2) direct exploratory laparotomy or laparoscopic procedure with abdominal pseudocyst excision or aspiration and VPS externalization or external ventricular drainage (EVD) and (a) new VPS and/or (b) reposition of the distal catheter into the nonperitoneal space; (3) aspiration only; (4) VPS externalization or EVD and new VPS; (5) reposition of the shunt; (6) replacement of the shunt; and (7) removal or reposition of the distal shunt catheter into the nonperitoneal space. Lately, for selected cases, after shunt externalization, de Oliveira et al. [31] had advocated the endoscopic third ventriculostomy in these cases because CSF flow is reestablished and the peritoneal cavity would be preserved for future use.
Regarding the risk of the recurrence of abdominal CSF pseudocyst in the literature, we performed an analysis for each subgroup of children and adults according to the etiology of hydrocephalus, shunt revision, and infection (Tables 4 and 5). The recurrence of abdominal pseudocyst occurred in 19.8 and 24.2 % of children and adults, respectively, with no information in 48 children and 22 adults. Age was not a relevant factor in the recurrence even for children (p = 0.198) or adults (p = 0.801), with no statistical difference between those who had the recurrence and those who had not. However, among male children, we identified a higher proportion statistically different (p = 0.011), representing 65.3 % of the children who had recurrence.
The recurrence of abdominal pseudocyst in children submitted previous shunt revision (86 %) found an odds ratio of two, although without significant association. The most frequent hydrocephalus etiologies found in these children were congenital hydrocephalus (27 %, OR = 1.2), myelomeningocele (25 %, OR = 1.2), and intraventricular hemorrhage (23 %, OR = 1.8); however, they also have not found significant statistical associations. In adults, congenital hydrocephalus (25 %, OR = 8, p = 0.07) was suggested to be a relevant risk factor for CSF abdominal pseudocyst recurrence.
With respect to the surgical treatment developed, we described all surgeries reported in the literature for adults and children with the odds ratio of recurrence for each intervention evaluated (Table 6). For children, the odds of recurrence was statistically associated with VPS reposition (odds 9.4 and p = 0.000). In contrast, the lowest odds of recurrence was identified for repositioning the distal catheter into the nonperitoneal space without exploratory laparotomy procedure after removing the VPS (odds = 0.08 and p = 0.001), and for adults, we have not found any statistical association. Therefore, the reposition of the peritoneal catheter on the abdominal cavity seems to carry more risk of recurrence in children compared with adults, and the reposition of the distal shunt into the nonperitoneal space is not a risk factor for recurrence in children.
By checking the different surgeries performed after or without exploratory laparotomy for CSF pseudocyst excision or aspiration, we found that the number of recurrence in children was higher for treatments without exploratory laparotomy (55 % and p = 0.853) than for the group with laparotomy technique (39 % and p = 0.255), but there was no statistical relationship with recurrence. In adults, the situation is different because 75 and 13 % of the number of recurrences were identified for the group of treatment with and without exploratory laparotomy, respectively. However, we do not identify statistical significance (p = 0.556 and p = 0.544).
In children, the abdominal pseudocyst recurrence with the reposition of the distal shunt after exploratory laparotomy treatment was not statistically significant among patients with negative CSF cultures; however, for treatment with the reposition of the distal shunt without exploratory laparotomy, we identified a suggestive probability for recurrence (p = 0.050).
Conclusions
In this literature survey, we have analyzed a relatively large number of abdominal CSF pseudocysts in children compared with adults. The level of evidence in most of the studies in the literature is low. However, from our comprehensive literature review, we conclude the following:
-
1.
As opposed to the literature reported, this review showed no statistical differences in the clinical picture between children and adults with this entity.
-
2.
The prevalence of infection is lower in adults than that in children and higher in children younger than 10 years.
-
3.
We identified a statistical significance association between shunt revision and positive cultures in children when compared with adults.
-
4.
We did not identify the predisposing causes of hydrocephalus related to the development of abdominal CSF pseudocyst between children and adults. However, congenital hydrocephalus suggests being a risk factor for recurrence in adults.
-
5.
Age was not a relevant factor in the abdominal CSF pseudocyst recurrence, although there is a higher proportion of recurrence in male children.
-
6.
In children, pseudocyst recurrence was statistically associated in treatment with repositioned distal catheter. In adults, we did not find any statistical association.
-
7.
In children, the number of recurrence was higher for treatments without exploratory laparotomy (55 %) than for the group with laparotomy technique (39 %). In adults, it was the opposite situation, that is, 75 % after exploratory laparotomy and 13 % without laparotomy.
-
8.
Future research in these patients not only will allow a better understanding of the pathogenesis of abdominal CSF pseudocyst but also will determine which procedure should be the best neurosurgical treatment in children and adults with these conditions.
References
Acharya R, Ramachandran CS, Singh S (2001) Laparoscopic management of abdominal complications in ventriculoperitoneal shunt surgery. J Laparoendosc Adv Surg Tech 11:167–170
Adegbite AB, Khan M (1982) Role of protein content in CSF ascites following ventriculoperitoneal shunting. J Neurosurg 57:423–425
Agarwal T, Pandey S, Niranjan A, Jain V, Mishra S, Agarwal V (2009) Unusual complication of ventriculoperitoneal shunt urgery. J Pediatr Neurosci 4:122–123
Agha FP, Amendola MA, Shirazi KK, Amendola BE, Chandler WF (1983) Abdominal complications of ventriculoperitoneal shunts with emphasis on the role of imaging methods. Surg Gynecol Obstet 156:473–478
Aguirre Rivero R, Pérez Salcedo C, Meza Martínez H, Kuri Guinto J, Vázquez Cruz I (1998) Giant abdominal pseudocyst in patients with ventriculoperitoneal shunt [in Spanish]. Rev Gastroenterol Mex 63:153–158
Ames RH (1967) Ventriculo-peritoneal shunts in the management of hydrocephalus. J Neurosurg 27:525–529
Anderson CM, Sorrells DL, Kerby JD (2003) Intraabdominal pseudocysts as a complication of ventriculoperitoneal shunts. J Am Coll Surg 196:297–300
Anderson CM, Sorrells DL, Kerby JD (2003) Intra-abdominal pseudocysts as a complication of ventriculoperitoneal shunts: a case report and review of the literature. Curr Surg 60:338–40
Aparici-Robles F, Molina-Fabrega R (2008) Abdominal cerebrospinal fluid pseudocyst: a complication of ventriculoperitoneal shunts in adults. J Med Imaging Radiat Oncol 52:40–43
Badiane SB, Sakho Y, Kabre A, Ba MC, Fall B, Ndoye N, Badiane M, Gueye EM, Gueye M (1997) Peritoneal pseudocysts: complications of ventriculo-peritoneal shunts. A propos of 3 cases. Dakar Med 42:149–151
Bartolek F, Zganjer M, Pajić A, Cizmić A, Kljenak A, Cigit I, Car A, Stepan J, Bartolek D, Boras A (2010) A 10-year experience in the treatment of intraabdominal cerebrospinal fluid pseudocysts. Coll Antropol 34(4):1397–1400
Baumgartner FJ, Moore TC, Mitchner J (1990) Recurrent ventriculoperitoneal shunt pseudocyst in a nine-year-old girl. Klin Wochenschr 68:485–487
Bauni CE, Sigura L, Carestia P, Urquiola C (2007) Intraperitoneal cerebrospinal fluid pseudocyst: an unusual complication of ventriculoperitoneal shunt. Apropos of 2 cases [in Spanish]. RAR 71:429–433
Besson R, Hladky JP, Dhellemmes P, Debeugny P (1995) Peritoneal pseudocyst–ventriculo-peritoneal shunt complications. Eur J Pediatr Surg 5:195–197
Birbilis T, Kontogianidis K, Matis G, Theodoropoulou E, Efremidou E, Argyropoulou P (2008) Intraperitoneal cerebrospinal fluid pseudocyst. A rare complication of ventriculoperitoneal shunt. Chirurgia 103:365–367
Briggs JR, Hendry GM, Minns RA (1984) Abdominal ultrasound in the diagnosis of cerebrospinal fluid pseudocysts complicating ventriculoperitoneal shunts. Arch Dis Child 59(7):661–4
Bryant MS, Bremer AM, Tepas JJ 3rd, Mollitt DL, Nquyen TQ, Talbert JL (1988) Abdominal complications of ventriculoperitoneal shunts. Case reports and review of the literature. Am Surg 54:50–5
Burchianti M, Cantini R (1988) Peritoneal cerebrospinal fluid pseudocysts: a complication of ventriculoperitoneal shunts. Child’s Nerv Syst 4:286–290
Buyukyavuz BI, Duman L, Karaaslan T, Turedi A (2012) Hyponatremic seizure due to huge abdominal cerebrospinal fluid pseudocsyt in a child with ventriculoperitoneal shunt: a case report. Turk Neurosurg 22:656–658
Castellucio MS, Hermida CR, Plaza PM, Licciardello M (2006) Intestinal occlusion in a patient with a ventriculoperitoneal shunt [in spanish]. Acta Gastroenterol Latinoam 36(3):108
Chandra S, Bhatnagar V, Mitra DK (1992) Intraperitoneal CSF Pseudocysts Following Ventriculo-peritoneal Shunts. Indian Pediatr 29:1438–1440
22. Chitkara N, Rahul G, Singla SL, Sharma NK (2004) Lower end of ventriculoperitoneal shunt embedding in liver parenchyma. Letter to the editor. Neurol India 52: 405
Chuang VP, Fried AM, Oliff M, Ellis GT, Sachatello CR (1978) Abdominal CSF pseudocyst secondary to ventriculoperitoneal shunt: diagnosis by computed tomography in two cases. J Comput Assist Tomogr 2:88–91
Chung JJ, Yu JS, Kim JH, Nam SJ, Kim MJ (2009) Intraabdominal complications secondary to ventriculoperitoneal shunts: CT findings and review of the literature. AJR Am J Roentgenol 193:1311–1317
Coley BD, Shiels WE 2nd, Elton S, Murakami JW, Hogan MJ (2004) Sonographically guided aspiration of cerebrospinal fluid pseudocysts in children and adolescents AJR. Am J Roentgenol 183:1507–151
Cone WV, Lewis RD, Jackson IJ (1949) Shunting of cerebrospinal fluid into the peritoneal cavity. Presented at meeting of American College of Physicians. Montreal, Canada
Coşkun E, Süzer T, Kildaci T, Şahin S, Tiryaki A, Devrent T, Tahta K (1999) Abdominal pseudocyst: an usual complication of ventriculoperitoneal shunts. Türk Nöroşirürji Dergisi 9:34–38
Courtice FC, Steinbeck AW (1951) Absorption of protein from the peritoneal cavity. J Physiol (Lond) 114:336–355
Davidson RI (1976) Peritoneal bypass in the treatment of hydrocephalus: historical review and abdominal complications. J Neurol Neurosurg Psychiatry 39:640–646
Davidson RI, Lingley JF (1975) Intraperitoneal pseudocysts: treatment by aspiration. Surg Neurol 4:33–36
de Oliveira RS, Barbosa A, Vicente YA, Machado HR (2007) An alternative approach for management of abdominal cerebrospinal fluid pseudocysts in children. Childs Nerv Syst 23:85–90
Deindl C, Kellnar S (1986) Diagnosis and therapy of intraperitoneal cerebrospinal fluid pseudocyst in ventriculoperitoneal cerebrospinal fluid shunts in patients with hydrocephalus. Z Kinderchir 41:295–298
Egelhoff J, Babcock DS, McLaurin R (1985) Cerebrospinal fluid pseudocysts: sonographic appearance and clinical management. Pediatr Neurosci 12:80–86
Ekong CE, Clein LJ (1979) Formation of abdominal cyst secondary to ventriculoperitoneal shunting. Can J Surg 22(3):250–3
Engelhard HH, Miller FB (1992) Abdominal pain resulting from cerebrospinal fluid pseudocyst and cholelithiasis. South Med J 85:851–852
Erşahin Y, Mutluer S, Tekeli G (1996) Abdominal cerebrospinal fluid pseudocysts. Child’s Nerv Syst 12:755–758
Faraj W, Ahmad HH, Mukherji D, Khalife M (2011) Hepatic cerebrospinal fluid pseudocyst mimicking hydatid liver disease: a case report. J Med Case Reports 5:475
Figueiredo DG, Carvalho FF (1981) Pseudo-cistosperitoneais como complicação de derivações liquoricas. Arq Neuro-Psiquiat 39:50–56
Fischer EG, Shillito J Jr (1969) Large abdominal cysts: a complication of peritoneal shunts. Report of three cases. J Neurosurg 31:441–444
Fortea-Sanchis C, Martínez-Ramos D, Merino J, Salvador-Sanchis JL (2011) Percutaneous drainage as a posible treatment of an intra-abdominal pseudo-cyst secondary to a ventriculoperitoneal catheter. Cir Esp 89:411–414
Gamal R, Moore TC (1988) Massive acquired omental cyst as a complication of ventriculo-peritoneal shunting. J Pediatr Surg 23:1041–1042
Gaskill SJ, Marlin AE (1989) Pseudocysts of the abdomen associated with ventriculoperitoneal shunts: a report of twelve cases and a review of the literature. Pediatr Neurosci 15:23–27
Gebarski KS, Gebarski SS, McGuillicuddy JE (1984) Cerebrospinal fluid abdominal cyst. Computed tomographic resolution of a sonographic dilemma. Surg Neurol 21:414–416
Ghidirim G, Mishin G, Zastavnitsky V, Brinza M (2010) Laparoscopic management of associated abdominal complications of ventriculoperitoneal shunt: case report. Eur Surg 42(4):184–186
Ghritlaharey RK, Budhwani KS, Shrivastava DK, Jain AK, Gupta G, Kushwaha AS (2006) CSF pseudocyst peritoneal cavity following VP shunt surgery: report of three cases in children and review of literature. J Indian Assoc Pediatr Surg 11:41–43
Goeser CD, McLeary MS, Young LW (1998) Diagnostic imaging of ventriculoperitoneal shunt malfunctions and complications. Radiographics 18:635–51
Golfine SL, Turetz F, Beck R, Eiger M (1978) Cerebrospinal fluid intraperitoneal cyst: an unusual abdominal mass. Am J Roentgenol 130:568–569
Gomutbutra T (2004) Large lower abdominal cerebrospinal fluid pseudocyst 6 years after a ventriculo-peritoneal shunt: clinical features and surgical management. Chiang Mai Med Bull 43:169–173
Grosfeld JL, Cooney DR, Smith J, Campbell R (1974) Intra-abdominal complications following ventriculoperitoneal shunt procedures. Pediatrics 54:791–796
Grunebaum M, Ziv N, Kornreich L, Horev G, Lombrozo R (1988) The sonographic signs of the peritoneal pseudocyst obstructing the ventriculo-peritoneal shunt in children. Neuroradiolog 30:433–488
Guice KS, Kosloske AM, Turner P, Wachtel T (1978) Recurrent pseudocyst from a ventriculoperitoneal shunt: an unusual abdominal mass. Am J Dis Child 132:285–286
Gutierrez FA, Raimondi AJ (1976) Peritoneal cysts: a complication of ventriculoperitoneal shunts. Surgery 79:188–92
Hahn YS, Engelhard H, McLone DG, Abdominal CSF pseudocyst (1985) Clinical features and surgical management. Pediatr Neurosci 12:75–79
Harsh GR (1954) Peritoneal shunt for hydrocephalus: utilizing the fimbria of the fallopian tube for entrance to the peritoneal cavity. J Neurosurg 11:284–294
Hashimoto M, Yokota A, Urasaki E, Tsujigami S, Shimono M (2004) A case of abdominal CSF pseudocyst associated with silicone allergy. Childs Nerv Syst 20(10):761–764
Hernández JG, Martínez JL, Romero T, Blanco R (2004) Abdominal pseudocyst in a patient with ventriculoperitoneal shunt. Case Report [in Spanish]. Cir Ciruj 72:401–403
Horikawa M, Yamada T, Tominaga K, Yoshida S (1999) Abdominal Cerebrospinal Fluid Pseudocyst in a Severely Handicapped Patient with Hidrocephalus. J Child Neurol 14:329–331
Hsieh CT, Pai CC, Tsai TH, Chiang YH, Su YH (2006) Hepatic cerebrospinal fluid pseudocyst: a case report and review of the literature. Neurol India 54(1):86–8
Ivan LP, Choo SH, Ventureyra ECG (1980) Complications of venriculoatrial and ventriculoperitoneal shunts in a new children’s hosp. Can J Surg 23:566–568
Jackson IJ, Snodgrass SR (1955) Peritoneal shunts in the treatment of hydrocephalus and increased intracranial pressure. J Neurosurg 12:216–222
Jain S, Bhandarkar D, Shah R, Vengsarkar U (2003) Laparoscopic management of complicated ventriculoperitoneal shunts. Neurol India 51(2):269–70
Kaplan M, Ozel SK, Akgun B, Kazez A, Kaplan S (2007) Hepatic pseudocyst as a result of ventriculoperitoneal shunts: case report and review of the literature. Pediatr Neurosurg 43:501–503
Kariyattil R, Steinbok P, Singhal A, Cochrane DD (2007) Ascites and abdominal pseudocysts following ventriculoperitoneal shunt surgery: variations of the same theme. J Neurosurg 106:350–353
Kim HB, Raghaavendran K, Kleinhaus S (1995) Management of an abdominal cerebrospinal fluid pseudocyst using laparoscopic techniques. Surg Laparosc Endosc 5:151–154
Koçak A, Baysal T, Çaylı SR, Ateş O, Önal C (2004) An unusual complication of ventriculo-peritoneal shunt: cerebrospinal fluid cyst in liver. European Journal of Radiology Extra 51(1):21–24
Kolić Z, Kukuljan M, Bonifačić D, Vukas D (2010) CSF liver pseudocyst as a complication of a ventriculoperitoneal shunt. Wien Klin Wochenschr 122:641–644
Latchaw JP Jr, Hahn JF (1981) Intraperitoneal pseudocyst associated with peritoneal shunt. Neurosurgery 8:469–472
Lee TG, Parsons PM (1978) Ultrasound diagnosis of cerebrospinal fluid abdominal cyst. Radiology 127:220
Leung GK (2010) Abdominal cerebrospinal fluid (CSF) pseudocyst presented with inferior vena caval obstruction and hydronephrosis. Childs Nerv Syst 26:1243–1245
Lloyd WM III, Doran S, Hellbusch L (2005) Abdominal pseudocysts: predisposing factor and treatment algorithm. Pediatr Neurosurg 41:77–83
Lortat-Jacob S, Pierre-Kahn A, Renier D, Hirsch JF, Martelli H, Pellerin D (1984) Abdominal complications of ventriculo-peritoneal shunts in children. 65 cases. Chir Pediatr 25:17–21
Mata J, Alegret X, Llauger J (1986) Splenic pseudocyst as a complication of ventriculoperitoneal shunt: CT features. J Comput Assist Tomogr 10:341–2
McLaurin R, Frame PT (1987) Treatment of infections of cerebrospinal fluid shunts. Rev Infect Dis 9(3):595–603
Mobley LW 3rd, Doran SE, Hellbusch LC (2005) Abdominal pseudocyst: predisposing factors and treatment algorithm. Pediatr Neurosurg 41:77–83
Nakagaki H, Matsunaga M, Maeyama R, Mizoguchi R (1979) Intraperitoneal pseudocyst after ventriculoperitoneal shunt. Surg Neurol 11:447–450
Nfonsam V, Chand B, Rosenblatt S, Turner R, Luciano M (2008) Laparoscopic management of distal ventriculoperitoneal shunt complications. Surg Endosc 22:1866–1870
Norfray JF, Henry HM, Givens JD, Sparberg MS (1979) Abdominal complications from peritoneal shunts. Gastroenterology 77:337–340
Nugent P, Hoshek S (1986) Large extra-abdominal cyst as a postpartum complication of peritoneal shunt. Case report. J Neurosurg 64(1):151–2
Oh A, Wildbrett P, Golub R, Yu LM, Goodrich J, Lee T (2001) Laparoscopic repositioning of a ventriculo-peritoneal catheter tip for a sterile abdominal cerebrospinal fluid (CSF) pseudocyst. Surg Endosc 15:518
Ohba S, Kinoshita Y, Tsutsui M, Nakagawa T, Shimizu K, Murakami H (2012) Formation of abdominal cerebrospinal fluid pseudocyst—case report. Neurol Med Chir (Tokyo) 52:838–842
Palomar JM, Matthews A, Evans BB (1977) Cerebrospinal fluid pseudocyst after urinary diversion. J Urol 118(6):1046–9
Parrish RA, Potts JM (1973) Torsion of omental cysts–a rare complication of ventriculoperitoneal shunt. J Pediatr Surg 8(6):969–70
Parry SW, Schuhmacher JF, Llewellyn RC (1975) Abdominal pseudocysts and ascites formation after ventriculoperitoneal shunt procedures. Report of four cases. J Neurosurg 43:476–80
Pathi R, Sage M, Slavotinek J, Hanieh A (2004) Abdominal cerebrospinal fluid pseudocyst. Australas Radiol 48:61–63
Peltier J, Demuynck F, Fichten A, Lefranc M, Toussaint P, Desenclos C, Nicot B, Pruvot AS, Le Gars D (2011) Non-traumatic pseudocyst of Glisson capsule complicating a ventriculoperitoneal shunt. Neurochirurgie 57:31–33
Pérez Moreno J, Saavedra Lozano J, García Leal R, Ferreras Ferreras B, Peinador García M, Sebastián S (2012) Difficulty in diagnosing infections in cerebrospinal fluid shunts [in Spanish]. An Pediatr (Barc) 77:143–145
Pernas JC, Catala J (2004) Case 72: pseudocyst around ventriculoperitoneal shunt. Radiology 232(1):239–243
Piercy SL, Gregory JG, Young PH (1984) Ventriculo-peritoneal shunt pseudocyst causing ureteropelvic junction obstruction in a child with myelomeningocele and retrocaval ureter. J Urol 132:345–348
Pombo FF, Suarez A, de Centi L, Varela Romero JR, Deben G (1989) Haemorrhage in an abdominal cerebrospinal fluid-pseudocyst as a complication of anticoagulant therapy. Rofo 150:733–734
Popa F, Grigorean VT, Onose G, Popescu M, Strambu M, Sandu AM (2009) Laparoscopic treatment of abdominal complications following ventriculoperitoneal shunt. J Med Life 4:426–436
Price HI, Rosenthal SJ, Betnitzky S, Lee KR, Wilson ME (1981) Abdominal pseudocysts as a complication of ventriculoperitoneal shunt. A report of two cases. Neuroradiology 21:273–276
Pumberger W, Löbl M, Geissler W (1998) Appendicitis in children with a ventriculoperitoneal shunt. Pediatr Neurosurg 28:21–26
Raghavendra BN, Epstein FJ, Subramanyam BR, Becker MH (1981) Ultrasonographic evaluation of intraperitoneal CSF pseudocyst. Report of 3 cases. Childs Brain 8:39–43
Rainov N, Schobess A, Heidecke V, Burkert W (1994) Abdominal CSF pseudocysts in patients with ventriculo-peritoneal shunts. Report of fourteen cases and review of the literature. Acta Neurochir (Wien) 127:73–78
Rana SR, Quivers ES, Haddy TB (1985) Hepatic cyst associated with ventriculoperitoneal shunt in a child with brain tumor. Childs Nerv Syst 1:349–51
Redman JF, Seibert JJ (1977) Abdominal and genitourinary complications following ventriculoperitoneal shunts. J Urol 119:295–7
Rekate HL, Yonas H, White RJ, Nulsen FE (1979) The acute abdomen in patients with ventriculoperitoneal shunts. Surg Neurol 11:442–5
Roitberg BZ, Tomita T, McLone DG (1998) Abdominal cerebrospinal fluid pseudocyst: a complication of ventriculoperitoneal shunt in children. Pediatr Neurosurg 29:267–73
Rovlias A, Kotsou S (2001) Giant abdominal CSF pseudocyst in an adult patient 10 years after a ventriculo-peritoneal shunt. Br J Neurosurg 15:191–192
Ruiz-Tovar J, Hargreaves GM, Delgado AL, Forcen PM, Rico RC (2010) Laparoscopic treatment of an intra-abdominal pseudo-cyst as a ventriculo-peritoneal catheter complication [in Spanish]. Cir Esp 88:414–5
Rush DS, Walsh JW, Belin RP, Pulito AR (1985) Ventricular sepsis and abdominally related complications in children with cerebrospinal fluid shunts. Surgery 97:420–427
Salomão JF, Leibinger RD (1999) Abdominal pseudocysts complicating CSF shunting in infants and children. Report of 18 cases. Pediatr Neurosurg 31:274–278
Sanal M, Laimer E, Haussler B, Hager J (2007) Abdominal cerebrospinal fluid pseudocysts in patients with ventriculoperitoneal shunt: 30 years of experience. J Indian Assoc Pediatric Surg 12:214–217
Seçer M, Dalgiçic A, Doğanay M, Altintoprak (2011) A rare complication of ventriculoperitoneal shunt; abdominal cerebrospinal pseudocyst. A case report. J Surg Arts 4:14–16
Sena FG, Sousa RM, Meguins LC (2010) Abdominal cerebrospinal fluid pseudocyst: a complication of ventriculoperitoneal shunt in a Brazilian Amazon woman. Case report. G Chir 31(8–9):371–373
Sharma AK, Pandey AK, Diyora BD, Mamidanna R, Sayal PP (2004) Abdominal CSF pseudocyst in a patient with ventriculoperitoneal shunt. Indian J Surg 66:360–363
Sivalingam S, Corkill G, Getzen L, Matolo N (1976) Reccurent abdominal cyst: a complication of ventriculoperitoneal shunt and its management. J Pediatr Surg 11:1029–1030
Suematzu K, Shitamichi M, Ide W, Okada Y, Sasaki T, Takeda R (1984) Abdominal pseudocyst associated with peritoneal shunt. Neurol Med Chir (Tokyo) 24:722–727
Takeuchi S, Takasato Y, Hiroyuki M (2012) Abdominal cerebrospinal fluid pseudocyst surrounding a ventriculoperitoneal shunt. Intern Med 51:343
Verma A, Mohan S, Gupta A (2012) Ventriculo-peritoneal shunts can cause liver injury, juxta and intrahepatic pseudocysts: imaging findings and review of literature. Clin Neurol Neurosurg 114:389–391
Wang BH, Hasadsri L, Wang H (2012) Abdominal cerebrospinal fluid pseudocyst mimicking full-term pregnancy. JSCR 7:6
Wang F, Miller JH (1989) Cerebrospinal fluid pseudocyst presenting as a hepatic mass: a complication of ventriculoperitoneal shunt. Pediatr Radiol 19:326–327
White B, Kropp K, Rayport M (1991) Abdominal cerebrospinal fluid pseudocyst: occurrence after intraperitoneal urological surgery in children with ventriculoperitoneal shunts. J Urol 146:583–585
Wolbers JG, van Zanten TE, van Alphen HA (1987) Ventriculo-peritoneal shunt procedure complicated by liver capsule perforation. A case report. Clin Neurol Neurosurg 89(1):55–7
Yamamoto Y, Waga S, Okada M (1979) Large abdominal pseudocyst as a complication of ventriculoperitoneal shunt–diagnosis by ultrasonography and whole body CT scan. No Shinkei Geka 7:589–592
Yamashita K, Yonekawa Y, Kawano T, Ihara I, Taki W, Kobayashi A, Handa Y, Kaku Y (1990) Intra-abdominal cyst following revision of ventriculoperitoneal shunt–case report. Neurol Med Chir (Tokyo) 30:748–752
Yuh S, Vassilyadi M (2012) Management of abdominal pseudocyst in shunt-dependent hydrocephalus. Surg Neurol Int 3:146
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dabdoub, C.B., Dabdoub, C.F., Chavez, M. et al. Abdominal cerebrospinal fluid pseudocyst: a comparative analysis between children and adults. Childs Nerv Syst 30, 579–589 (2014). https://doi.org/10.1007/s00381-014-2370-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-014-2370-2