Abstract
Introduction
The aim of this study was to report a rare pediatric case of spontaneous spinal epidural hematoma (SSEH) mimicking Guillain-Barré syndrome (GBS), secondary to an epidural arteriovenous malformation (AVM). Furthermore, a case-based update and insight into the entity is attempted.
Methods
An 8-year-old male presented with progressing severe lower limb weakness and no traumatic history. Presentation was mimicking GBS with ascending symptoms. Magnetic resonance (MR) scan revealed a dorsal epidural mass, extending from C6–C7 to T2, compressing the spinal cord. Emergency laminoplasties and surgical evacuation of the hematoma were performed. An up-to-date review of reported SSEH cases in children was conducted, with emphasis on underlying vascular malformations (epidural AVMs in particular). Pathogenesis, predisposing factors, imaging, diagnosis, treatment and outcome are discussed.
Results
The hematoma was successfully evacuated. A vascular membrane on the dura was peeled off and sent for histopathology. There was no evidence of intradural vascular penetration. The patient improved postoperatively and was able to walk with support 7 months later. Histology revealed closely packed thin-walled angiomatous structures with wide lumens (filled with red blood cells) with walls composed of collagen and smooth muscle fibers, findings consistent with AVM.
Conclusions
Non-traumatic SSEH is rare in the pediatric population. Although vascular malformations are suspected, they are extremely rarely identified histopathologically. This case represents one of the very few reports of pediatric SSEH caused by a histologically proven, purely epidural AVM. High index of clinical suspicion and low threshold for MR can lead to timely diagnosis and prompt treatment with good functional outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal epidural hematoma is usually observed in a traumatic context or following lumbar puncture or epidural anesthesia in a background of coagulopathy [1]. Non-traumatic hematoma can occur without any clear cause and is described as spontaneous [42]. Spontaneous spinal epidural hematoma (SSEH) represents an extremely rare cause of spinal cord compression in the pediatric age range [1, 40, 41, 50]. Bleeding predisposition constitutes the most common pathological substrate in this patient group [40].
Although suspected, vascular malformations have only been identified as the underlying lesion in less than ten children, only two of which had a purely extradural intraspinal arteriovenous malformation (AVM). We report a rare case of spontaneous hemorrhage from an epidural AVM in an 8-year-old male and attempt a case-based update on the entity. To our knowledge, this represents the third case of spinal cord compression from a non-traumatic SSEH caused by a histologically proven epidural arteriovenous malformation. Clinical presentation was mimicking Guillain-Barré syndrome (GBS), diagnosis was set with magnetic resonance imaging, and pathology was confirmed by histological analysis.
Case presentation
An 8-year-old male presented to the pediatric department with a 24-h history of progressing severe weakness of lower limbs. No history of trauma was mentioned. Neurological examination revealed flaccid paraplegia, absent reflexes of the lower limbs and sensory impairment below the T2 level. Motor and sensory system examination of the upper extremities and cranial nerves was initially normal. Presentation was mimicking GBS with ascending symptoms affecting the lower limbs first and progressing upwards. Bladder and bowel sphincters control was affected.
Magnetic resonance (MR) scan of the whole spine revealed a large posterior epidural mass, extending from C6–C7 to T2 level, displacing the spinal cord anteriorly and slightly to the left. The mass was isointense with the spinal cord on T1-weighted images, hyperintense with regions of low signal intensity on T2-weighted images and showed no avid enhancement after the intravenous administration of gadolinium, findings consistent with a possible epidural hematoma (Fig. 1). Coagulation profile was within normal range and the patient had never received any anticoagulant medication.
Spinal epidural hematoma, extending from C6–C7 to T2 level, displacing the spinal cord anteriorly and slightly to the left. Regions of low signal intensity can be noted in T2-weighted images on the periphery of the lesion. a Sagittal T2-weighted image. b, c Sagittal T1-weighted images before and after the intravenous administration of gadolinium, respectively. d Axial T2-weighted. e Axial post-gadolinium T1-weighted images
The patient underwent emergency C7–T3 laminoplasties. Intraoperatively, after removal of the laminae, there was egress of liquefied and solid blood. The blood clot was extending from C6–C7 to T3. The epidural space was irrigated free of blood, under which a thick vascular membrane was lining on the dorsal dura. This membrane was completely peeled off the dura and sent for histopathology. The membranous material was coated with blood and no vessels could be grossly seen. There was no evidence of vascular penetration through the dura.
Histologic sections (Fig. 2) revealed fibroadipose tissue, containing closely packed thin-walled angiomatous structures with wide lumens, filled with red blood cells. The walls of these structures were composed of collagen fibers and occasional smooth muscle fibers, as was evident on histochemical (Masson’s trichrome) and immunohistochemical (smooth muscle actin) stains, findings consistent with AVM. In adjacent areas, there were cystic spaces lined by granulation tissue, containing thrombi (hematoma formation). The fibroadipose tissue showed hemorrhage and focal fibroblastic reaction (Fig. 2).
Histological sections. a Representative area of angiomatous structures (hematoxylin and eosin, ×200). b Immunohistochemical stain for smooth muscle actin (immunohistochemical stain, ×100). Histology revealed fibroadipose tissue, containing closely packed thin-walled angiomatous structures with wide lumens, filled with red blood cells. The walls of these structures were composed of collagen fibers and occasional smooth muscle fibers, findings consistent with AVM. In adjacent areas, there were cystic spaces lined by granulation tissue and containing thrombi (hematoma formation)
A postoperative MR scan confirmed complete resection of the posterior epidural mass and re-expansion of the previously compressed spinal cord. Limited intramedullary high signal intensity on T2-weighted sequences was detected, probably representing compression-induced myelitis. No pathologic enhancement was present (Fig. 3). Two weeks postoperatively, the patient underwent spinal angiography which did not reveal any residual vascular or other pathology.
Postoperative MR scan. a Sagittal T2-weighted image. b Axial T2-weighted image (degraded low quality image). c, d Sagittal T1-weighted images before and after the intravenous administration of gadolinium, respectively. Images reveal the complete evacuation of the dorsal epidural mass, repositioning of the spinal cord, and a small intramedullary lesion with high signal intensity on T2-weighted sequences, with no pathologic enhancement. Fluid collection is noted in the operative field, around the spinous processes
After the operation, the patient partially improved, initially recovering motor strength proximally in the lower limbs, and was sent for rehabilitation. Seven months after the operation, the patient was able to walk with support.
Discussion
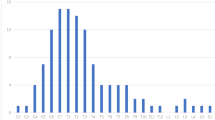
The term SSEH refers to hemorrhage not related to any precipitating cause, such as a traumatic injury [4, 17] and accounts for 40 to 50 % of spinal epidural hematomas in the general population [42]. Non-traumatic SSEH in the pediatric age group is extremely rare [44], with overall less than 40 cases reported in the English literature [6, 9–11, 23, 28, 29, 34, 37, 40, 45, 46, 48, 49, 51]. Age distribution shows bimodal peaks at 15 to 20 and 65 to 70 years [25], which makes it very rare in children [3]. The first report was by Jackson in 1869 in a 14-year-old girl [2, 22, 40]. Two extensive reviews of the literature discovered 23 reported cases in 1994 [7], which increased to 27 reports by 1998 [40, 41]. Cakir et al. [6] identified 32 cases until 2004 in the literature. Liu et al. [30] reported a series of 23 patients from 1998 to 2006, 7 of which were between 10 and 19 years old.
The most common locations include the dorsal epidural space of the cervicothoracic junction for those younger than 40 years and the thoracolumbar junction for those 40 to 80 years [19]. The cervicothoracic region is the most common location for SSEH in children [1, 2, 40] and, in particular, the C5–T1 regions [3, 40].
Typical presentation is with acute onset of neck or back pain and radiculopathy, followed within hours by myelopathy [5], although nonspecific or even misleading clinical signs and symptoms have also been reported in children, resulting sometimes in a delay of diagnosis [40, 45]. Differential diagnosis is broad and includes intrinsic or extrinsic cord tumor, unwitnessed or minor trauma, spinal abscess, spinal cord ischemia, disk disease, GBS, transverse myelitis, and congenital abnormalities such as a syringomyelia [1, 6]. Presentation in our patient was mimicking GBS, in which a very common pattern is the ascending version with symptoms affecting the lower limbs first and progressing upwards. Manifestation as GBS has previously been reported for SSEH in children only in very few cases [6, 31, 50].
Multiple predisposing etiopathogenic factors have been associated with SSEH, most of which are related to inherited or acquired coagulopathic states, blood dyscrasias (leukemia or hemophilia), anticoagulant or thrombolytic therapy, spinal vascular malformations (AVM, hemangioma), cocaine use and chiropractic spinal manipulation [1, 15, 40]. Iatrogenic factors such as lumbar puncture or epidural anesthesia have also been reported [32]. Other possible causes in adults include atherosclerotic disease, hypertension and bleeding diatheses [13, 17, 42]. Hemorrhagic diathesis (use of anticoagulants, blood dyscrasias) is the most commonly associated, potential etiopathogenic factor, encountered in more than 30 % of pediatric SSEH [40]. Vascular malformations, although suspected as underlying lesions, are rarely identified at pathological examination, which makes this case quite rare. Several adult cases have been attributed to vascular malformations in the epidural space [14, 16]; Kubo et al. [26], in a literature review of 99 adult patients with SSEH, found an underlying vascular malformation in 14 cases. To our knowledge, very few pediatric cases with SSEH attributable to a proven vascular malformation have been described [13, 35].
Vascular malformations that have been overlooked or obliterated could be a possible explanation in idiopathic cases [16]. A vascular anomaly is often suspected yet difficult to prove [1]. In the pediatric age group, a purely epidural vascular malformation responsible for non-traumatic SSEH is reported in only few cases (Table 1). Chuang et al. [11] reported two cases of purely epidural arteriovenous fistulas (AVF); Moiyadi et al. [34] described a purely extradural non-osseous spinal epithelioid hemangioma without bony involvement; Nadig et al. [37] presented an epidural AVM in a patient with NF1; finally, Muhonen et al. [35] reported an extradural vascular malformation devoid of elastin. Lo [31] described two cases of SSEH having cavernous vascular malformation origin, one with an intramedullary AVM and one with an extradural hemangioma. Miyagi et al. [33] reported a cervical epidural hematoma secondary to an AVM in a 16-year-old patient. Kitagawa et al. [24] reviewed 16 previously published pediatric cases of paraspinal AVMs, in which the patients had presented with spinal venous hypertension, and described the case of a 12-year-old child with a paraspinal AVM who presented with spontaneous spinal epidural hematoma.
The pathogenesis of SSEH remains unclear [40]. The source of bleeding was generally thought to be venous in origin. The fragile valveless epidural venous plexus is unprotected from sudden fluctuations of intrathoracic and intra-abdominal pressure after activities such as sneezing, coughing, voiding, and bending [2, 7, 17, 40, 46]. Arterial origin resulting from disruption of a tortuous arterial plexus by traction on nerve roots also has been suggested [40]. Miyagi et al. [33] suggested that an arterial source was more persuasive, since pressure inside the epidural venous plexus is lower than intrathecal pressure at the same level. In addition, the rapidly deteriorating neurological deficits after the initial onset of back pain suggests fast accumulation of hematoma and spinal cord compression, which would be consistent with arterial origin [30, 33].
MR imaging is the modality of choice for the evaluation of a suspected epidural hematoma, not only by displaying high sensitivity in detecting blood products and defining the age of hemorrhage but also being particularly accurate in demonstrating the extent of the hematoma and its effect on the spinal cord. The most usual findings within 24 h from onset are isointensity in T1-weighted images and hyperintensity in T2-weighted images. After 24 h, it appears as a high signal on T1-weighted images and a low signal on T2-weighted images. After injection of gadolinium, peripheral enhancement of lesion is mostly found and central enhancement is occasionally found [8]. Holtas et al. [21] suggested that a change of signal isointensity in the hyperacute phase to signal hyperintensity after 36 h could be pathognomonic for SSEH, but in the vast majority of the reported studies, including ours, the MR scan is not repeated, because a rapid evacuation of the hematoma is indicated. Liao et al. [29] reported that T2-weighted images have a greater diagnostic value since they can detect foci of very low signal intensity, representing hemosiderin deposits. However, in some reported studies, no hemosiderin deposits could be detected in T2-weighted images, probably because of the rapid removal of hemorrhagic products from the epidural space, provided by its great vascularity. In our case, regions of low signal intensity in T2-weighted images were noted mainly on the periphery of the hematoma.
Spinal angiography is a useful technique to demonstrate AVMs and is considered the gold standard for diagnosis by many authors [13, 35, 38]. However, clinical presentation may be too rapid to allow preoperative angiography. Furthermore, if a vascular malformation is not demonstrated or suspected on MR, angiography may not be helpful either. If the neurological status of the patient is stable, angiography could be preoperatively performed to establish the diagnosis [13]. In cases with progressive deficits where the neurological condition does not allow angiography, consideration should be given to a postoperative study [35, 38].
Spontaneous rupture of occult AVMs has been postulated as a cause of SSEH in children [3, 4]. Although often suspected as a cause of SSEH, vascular malformations have rarely been demonstrated [35]. Arteriovenous malformations are identified histopathologically by the presence of elastin and smooth muscle fibers in the walls of clustered abnormal arteries and veins, while cavernous angiomas are devoid of elastin or smooth muscle fibers in the walls of their clustered abnormal vessels [18]. In the present study, we describe a non-traumatic SSEH caused by a histologically proven vascular malformation. The latter was composed by closely packed abnormal vessels, whose walls were thin, containing collagen and smooth muscle fibers, findings characteristic of AVM.
The vast majority of dural AVMs affect elderly patients and are thought to be acquired [35]. A distinguishing feature between dural and epidural vascular malformations is the intradural extension of blood vessels in dural vascular malformations. Intradural vascular malformations have their nidus in the cord or pia and receive their blood supply from the medullary arteries [47]. The presence of flow voids and serpentine vessels intradurally can differentiate dural from purely epidural vascular malformations [35]. The vascular malformation we describe in this case was located entirely in the epidural space and had no evidence of intradural penetration of draining veins. The blood supply to epidural vascular malformations is purely within the epidural space. Reports of such lesions are rare, particularly in childhood, and have been described as venous angioma, hemangioma, or epidural varix [12, 14, 17]. Purely epidural vascular malformations are likely fed by radicular vessels accompanying the exiting nerve root [13, 35]. This concept is supported by the common location of SSEH in the lower cervical and thoracic region, where radicular arteries are prominent [13, 16, 17, 36].
Regardless of the cause of SSEH, early diagnosis and surgical evacuation allow maximal functional recovery [1, 20, 27]. Early surgery, preferably within 48 h, is indicated for patients with progressive neurological deficit [39]. Decompressive laminectomy and evacuation of the hematoma is usually the treatment of choice. Laminoplasties can also be performed, in order to decrease the risk of spinal deformity in children, particularly in the cervical region or cervicothoracic junction. Time lapse between symptom onset and surgical intervention is critical. Favorable outcomes can be achieved when surgical intervention is performed within 36 or 48 h after onset in patients with complete and incomplete deficits, respectively [20]. Unlike adults, delayed recovery of neurological function can occur in children [39, 41], even if the period between the onset of clinical presentation and surgery exceeds 72 h [39]. The longest duration of time (2 months) between initial symptoms of SSEH and surgical decompression was reported by Poonai et al. [43]. In children, surgical decompression should be considered even despite delayed presentation and poor neurological status, as the benefits of surgery, however delayed, far outweigh the morbidity occurring following nonoperative treatment [39]. Last but not least, recovery after surgery depends on the severity of preoperative neurologic deficit [17, 27].
Conservative management can be an option in patients with minimal or improving neurological deficits. Recently, the number of diagnosed SSEH cases as well as the number of patients not requiring surgery have increased owing to the wider use of early MR [3]. Azumagawa et al. [3] reviewed the literature since 1988 and identified at least 15 cases with spontaneous regression of SSEH younger than 18 years.
Conclusion
Non-traumatic SSEH in pediatric population is a rare pathological entity. The case presented here is one of the very few reports of SSEH in children caused by a histologically proven epidural AVM, with a presentation mimicking GBS and no significant previous medical history, no trauma, and no warning signs. SSEH should be included in the differential diagnosis in patients whose presentation is even slightly suggestive. A high index of clinical suspicion and a low threshold for MR are required for timely diagnosis, which is essential due to the high risk of poor outcome without treatment.
References
Abram HS, DeLaHunt MJ, Merinbaum DJ, Hammond DN (2007) Recurrent spontaneous spinal epidural hematoma in a child: first case report. Pediatr Neurol 36(3):177–180. doi:10.1016/j.pediatrneurol.2006.09.009
Arya R, Jain P, Kumar A, Gulati S (2012) Spontaneous spinal epidural hematoma in an infant. J Child Neurol 27(12):1577–1579. doi:10.1177/0883073811435241
Azumagawa K, Yamamoto S, Tanaka K, Sakanaka H, Teraura H, Takahashi K, Tamai H (2012) Non-operative treated spontaneous spinal epidural hematoma in a 12-year-old boy. Pediatr Emerg Care 28(2):167–169. doi:10.1097/PEC.0b013e318244785d
Beatty RM, Winston KR (1984) Spontaneous cervical epidural hematoma. A consideration of etiology. J Neurosurg 61(1):143–148. doi:10.3171/jns.1984.61.1.0143
Binder DK, Sonne DC, Lawton MT (2004) Spinal epidural hematoma. Neurosurg Q 14(1):51–59
Cakir E, Karaarslan G, Usul H, Baykal S, Kuzeyli K, Mungan I, Yazar U, Peksoylu B, Aynaci M, Cakir F (2004) Clinical course of spontaneous spinal epidural haematoma mimicking Guillain-Barré syndrome in a child: a case report and literature review. Dev Med Child Neurol 46(12):838–842
Caldarelli M, Di Rocco C, La Marca F (1994) Spontaneous spinal epidural hematoma in toddlers: description of two cases and review of the literature. Surg Neurol 41(4):325–329
Caldemeyer KS, Mocharla R, Moran CC, Smith RR (1993) Gadolinium enhancement in the center of a spinal epidural hematoma in a hemophiliac. J Comput Assist Tomogr 17(2):321–323
Chang CW, Lin LH, Liao HT, Hung KL, Hwan JS (2002) Spontaneous spinal epidural hematoma in a 5-year-old girl. Acta Paediatr Taiwan 43(6):345–347
Chretiennot-Bara C, Guet A, Balzamo E, Noseda G, Torchet MF, Rothshild C, Blakime P, Schmit P (2001) Epidural hematoma in a child with hemophilia: diagnostic difficulties. Arch Pediatr 8(8):828–833
Chuang NA, Shroff MM, Willinsky RA, Drake JM, Dirks PB, Armstrong DC (2003) Slow-flow spinal epidural AVF with venous ectasias: two pediatric case reports. AJNR Am J Neuroradiol 24(9):1901–1905
Cooper DW (1967) Spontaneous spinal epidural hematoma. Case report. J Neurosurg 26(3):343–345. doi:10.3171/jns.1967.26.3.0343
D’Angelo V, Bizzozero L, Talamonti G, Ferrara M, Colombo N (1990) Value of magnetic resonance imaging in spontaneous extradural spinal hematoma due to vascular malformation: case report. Surg Neurol 34(5):343–344
Dickman CA, Zabramski JM, Sonntag VK, Coons S (1988) Myelopathy due to epidural varicose veins of the cervicothoracic junction. Case report. J Neurosurg 69(6):940–941. doi:10.3171/jns.1988.69.6.0940
Dinsmore AJ, Leonard RB, Manthey D (2005) Spontaneous spinal epidural hematoma: a case report. J Emerg Med 28(4):423–426. doi:10.1016/j.jemermed.2004.11.023
Emery DJ, Cochrane DD (1988) Spontaneous remission of paralysis due to spinal extradural hematoma: case report. Neurosurgery 23(6):762–764
Foo D, Rossier AB (1981) Preoperative neurological status in predicting surgical outcome of spinal epidural hematomas. Surg Neurol 15(5):389–401
Graziani N, Bouillot P, Figarella-Branger D, Dufour H, Peragut JC, Grisoli F (1994) Cavernous angiomas and arteriovenous malformations of the spinal epidural space: report of 11 cases. Neurosurgery 35(5):856–863, discussion 863–854
Groen RJ (2004) Non-operative treatment of spontaneous spinal epidural hematomas: a review of the literature and a comparison with operative cases. Acta Neurochir (Wien) 146(2):103–110. doi:10.1007/s00701-003-0160-9
Groen RJ, van Alphen HA (1996) Operative treatment of spontaneous spinal epidural hematomas: a study of the factors determining postoperative outcome. Neurosurgery 39(3):494–508, discussion 508–499
Holtas S, Heiling M, Lonntoft M (1996) Spontaneous spinal epidural hematoma: findings at MR imaging and clinical correlation. Radiology 199(2):409–413
Jackson R (1869) Case of spinal apoplexy. Lancet 94(2392):5–6
Kirwan R, Saigal G, Faingold R, O’Gorman A (2004) Nontraumatic acute and subacute enhancing spinal epidural hematoma mimicking a tumor in a child. Pediatr Radiol 34(6):499–502. doi:10.1007/s00247-003-1129-9
Kitagawa RS, Mawad ME, Whitehead WE, Curry DJ, Luersen TG, Jea A (2009) Paraspinal arteriovenous malformations in children. J Neurosurg Pediatr 3(5):425–428. doi:10.3171/2009.2.PEDS08427
Kreppel D, Antoniadis G, Seeling W (2003) Spinal hematoma: a literature survey with meta-analysis of 613 patients. Neurosurg Rev 26(1):1–49. doi:10.1007/s10143-002-0224-y
Kubo Y, Nishiura I, Koyama T (1984) [Repeated transient paraparesis due to solitary spinal epidural arterio-venous malformation. A case report]. No Shinkei Geka 12(7):857, Article in Japanese
Lawton MT, Porter RW, Heiserman JE, Jacobowitz R, Sonntag VK, Dickman CA (1995) Surgical management of spinal epidural hematoma: relationship between surgical timing and neurological outcome. J Neurosurg 83(1):1–7. doi:10.3171/jns.1995.83.1.0001
Liao CC, Hsieh PC, Lin TK, Lin CL, Lo YL, Lee SC (2009) Surgical treatment of spontaneous spinal epidural hematoma: a 5-year experience. J Neurosurg Spine 11(4):480–486. doi:10.3171/2009.4.SPINE08904
Liao CC, Lee ST, Hsu WC, Chen LR, Lui TN, Lee SC (2004) Experience in the surgical management of spontaneous spinal epidural hematoma. J Neurosurg 100(1 Suppl Spine):38–45
Liu Z, Jiao Q, Xu J, Wang X, Li S, You C (2008) Spontaneous spinal epidural hematoma: analysis of 23 cases. Surg Neurol 69(3):253–260. doi:10.1016/j.surneu.2007.02.019, discussion 260
Lo MD (2010) Spinal cord injury from spontaneous epidural hematoma: report of 2 cases. Pediatr Emerg Care 26(6):445–447
Metzger G, Singbartl G (1991) Spinal epidural hematoma following epidural anesthesia versus spontaneous spinal subdural hematoma. Two case reports. Acta Anaesthesiol Scand 35(2):105–107
Miyagi Y, Miyazono M, Kamikaseda K (1998) Spinal epidural vascular malformation presenting in association with a spontaneously resolved acute epidural hematoma. Case report. J Neurosurg 88(5):909–911. doi:10.3171/jns.1998.88.5.0909
Moiyadi AV, Bhat DI, Devi BI, Mahadevan A, Shankar SK, Sastry KV (2005) Spinal epidural epitheloid hemangioma—case report and review of the literature. Pediatr Neurosurg 41(3):155––157. doi:10.1159/000085875
Muhonen MG, Piper JG, Moore SA, Menezes AH (1995) Cervical epidural hematoma secondary to an extradural vascular malformation in an infant: case report. Neurosurgery 36(3):585–587, discussion 587–588
Muller H, Schramm J, Roggendorf W, Brock M (1982) Vascular malformations as a cause of spontaneous spinal epidural haematoma. Acta Neurochir (Wien) 62(3–4):297–305
Nadig M, Munshi I, Short MP, Tonsgard JH, Sullivan C, Frim DM (2000) A child with neurofibromatosis-1 and a lumbar epidural arteriovenous malformation. J Child Neurol 15(4):273–275
Nagel MA, Taff IP, Cantos EL, Patel MP, Maytal J, Berman D (1989) Spontaneous spinal epidural hematoma in a 7-year-old girl. Diagnostic value of magnetic resonance imaging. Clin Neurol Neurosurg 91(2):157–160
Nayak N, Baldawa S, Diyora B, Sharma A (2011) Delayed recovery of paraplegia following surgical evacuation of spontaneous cervicothoracic epidural hematoma. Childs Nerv Syst 27(12):2031–2032. doi:10.1007/s00381-011-1591-x
Patel H, Boaz JC, Phillips JP, Garg BP (1998) Spontaneous spinal epidural hematoma in children. Pediatr Neurol 19(4):302–307
Pecha MD, Able AC, Barber DB, Willingham AC (1998) Outcome after spontaneous spinal epidural hematoma in children: case report and review of the literature. Arch Phys Med Rehabil 79(4):460–463
Penar PL, Fischer DK, Goodrich I, Bloomgarden GM, Robinson F (1987) Spontaneous spinal epidural hematoma. Int Surg 72(4):218–221
Poonai N, Rieder MJ, Ranger A (2007) Spontaneous spinal epidural hematoma in an 11-month-old girl. Pediatr Neurosurg 43(2):121–124. doi:10.1159/000098385
Posnikoff J (1968) Spontaneous spinal epidural hematoma of childhood. J Pediatr 73(2):178–183
Ravid S, Schneider S, Maytal J (2002) Spontaneous spinal epidural hematoma: an uncommon presentation of a rare disease. Childs Nerv Syst 18(6–7):345–347. doi:10.1007/s00381-001-0540-5
Rosenberg O, Itshayek E, Israel Z (2003) Spontaneous spinal epidural hematoma in a 14-year-old girl. Case report and review of the literature. Pediatr Neurosurg 38(4):216–218
Rosenblum B, Oldfield EH, Doppman JL, Di Chiro G (1987) Spinal arteriovenous malformations: a comparison of dural arteriovenous fistulas and intradural AVM’s in 81 patients. J Neurosurg 67(6):795–802. doi:10.3171/jns.1987.67.6.0795
Sano H, Satomi K, Hirano J (2004) Recurrent idiopathic epidural hematoma: a case report. J Orthop Sci 9(6):625–628. doi:10.1007/s00776-004-0821-4
Tender GC, Awasthi D (2004) Spontaneous cervical spinal epidural hematoma in a 12-year-old girl: case report and review of the literature. J La State Med Soc 156(4):196–198
Tewari MK, Tripathi LN, Mathuriya SN, Khandelwal N, Kak VK (1992) Spontaneous spinal extradural hematoma in children. Report of three cases and a review of the literature. Childs Nerv Syst 8(1):53–55
van Heesewijk JP, Casparie JW (2000) Acute spontaneous spinal epidural haematoma in a child. Eur Radiol 10(12):1874–1876
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Paraskevopoulos, D., Magras, I. & Polyzoidis, K. Spontaneous spinal epidural hematoma secondary to extradural arteriovenous malformation in a child: a case-based update. Childs Nerv Syst 29, 1985–1991 (2013). https://doi.org/10.1007/s00381-013-2214-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2214-5