Abstract
Background
Intracranial germ cell tumors (GCTs) frequently take an insidious clinical course before diagnosis. To date, clinical latency has been discussed in the context of germinoma in the suprasellar area and basal ganglia.
Objective
In this study, we classified the clinical latency of intracranial GCTs into three categories and described their characteristics in order to understand the full spectrum of the phenomenon.
Methods
In a cohort of 181 patients with intracranial GCTs, 17 patients had a delayed diagnosis of more than 3 months (90 days) from the initial brain magnetic resonance imaging to the definitive GCT diagnosis. Clinical records and radiological data of the patients were reviewed.
Results
The patients with a delayed diagnosis were categorized into three groups according to their tumor location: suprasellar (nine patients), basal ganglia (six patients), and pineal (two patients). Initial symptomatology corresponded with the tumor location: central diabetes insipidus for the suprasellar group, hemiparesis for the basal ganglia group, and precocious puberty for the pineal group. The overall survival of patients with germinoma and delayed diagnosis was significantly shorter than that of patients who were diagnosed within 3 months (P = 0.002).
Conclusions
Clinical latency and delayed diagnosis are not restricted to germinomas in the suprasellar area and basal ganglia; they are canonical features of intracranial GCTs including pineal non-germinomatous GCTs. Early detection and proactive diagnosis of these tumors are required because diagnosis delay may negatively influence patient survival.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intracranial germ cell tumor (GCT) is an important pediatric brain tumor. It is more prevalent in East Asian countries where intracranial GCTs occupy around 10 % of all pediatric brain tumors [1]. Intracranial GCTs predominantly develop in specific sites, notably in the suprasellar area, pineal region, and basal ganglia [2, 3]. All of these structures are situated around the third ventricle, overlying the hypothalamus, which governs the endocrine and vegetative functions of the body. The symptoms and signs of intracranial GCTs, depending on the location and size of the tumors, include headaches, visual disturbances, and endocrinopathy. For patients with a GCT in the basal ganglia, progressive hemiparesis is also a common complaint [4]. Intriguingly, intracranial GCTs have a tendency to progress insidiously, and many patients show a long symptomatic period before GCT diagnosis [5]. A protracted course of disease can be observed from symptom onset to the overt manifestation of an intracranial GCT [6, 7]. These patients are characterized by normal or slightly abnormal neuroimaging findings at presentation, a long symptomatic period, and a delay in the diagnosis, often more than several years. Occasionally, patients exhibit only a loss of the bright signal intensity of the posterior hypophysis on the T1-weighted magnetic resonance (MR) images, which represents the nonspecific finding of central diabetes insipidus (CDI) [7]. This type of clinical latency is challenging because surgical biopsy cannot be performed unless there is a highly suspicious contrast-enhancing lesion on neuroimaging. To date, experiences of GCT latency have been restricted to germinomas developing in the suprasellar area or basal ganglia, and to our knowledge, there have been no reports of a pineal GCT latency.
In this study, we assessed the clinical latency and delayed diagnosis of intracranial GCTs in a large cohort of patients. We found 17 patients with an intracranial GCT that had a delayed diagnosis of more than 3 months because the initial MRI provided no definitive clinical decision to perform a surgical biopsy. We categorized these patients into three groups according to the tumor location and analyzed their pattern and clinical features. Interestingly, two patients with a delayed diagnosis had a pineal non-germinomatous GCT (NGGCT). This study demonstrated that latency and delayed diagnosis are not restricted to suprasellar or basal ganglia germinomas, but these are fundamental characteristics of intracranial GCTs, including pineal NGGCTs.
Methods
Patient selection
The Institutional Review Boards of the Seoul National University Hospital approved this study protocol. We searched the electronic patient databases of our institution for patients who were diagnosed with intracranial GCTs. The databases nonselectively included all the patients who checked into the Seoul National University Children’s Hospital and the Seoul National University Hospital. We limited our search to the period between January 1998 and December 2010 because the radiological and clinical records for patients enrolled before 1998 were not fully digitalized and many of them were not available for review. We excluded metastatic germ cell tumors. Within the study period, 181 patients were clinically diagnosed with intracranial GCTs. Pineal region (N = 81; 44.8 %) was the most common tumor location, followed by the suprasellar region (N = 38; 21.0 %), basal ganglia (N = 29; 16.0 %), bifocal presentation in both suprasellar and pineal regions (N = 23; 12.7 %), and other regions (N = 10; 5.5 %). The detailed clinical characteristics of these patients were described in a previous study [8].
In the patient cohort, we investigated the period between initial symptom onset and the definitive intracranial GCT diagnosis (prodrome I). We then calculated the time interval between the initial brain MRI and the definitive diagnosis (prodrome II). The time at which a definitive diagnosis was made was determined as the day the tissue biopsy was performed or when elevated levels of tumor markers [i.e., beta-human chorionic gonadotropin (β-HCG) and/or alpha-fetoprotein (AFP)] sufficient for a diagnosis of GCT without biopsy were documented in either serum or cerebrospinal fluid (CSF). As expected, prodrome I (median, 2 month; range, 0–86 months) was more variable than prodrome II (median, 0 month; range, 0–64 months) according to the tumor location, the type and severity of symptoms, and the patients’ access to medical resources. Prodrome II was shortened because a tumor marker study and/or surgical biopsy are readily performed if a suspicious lesion is found in the MRI. In 160 patients (88.4 %), a definitive diagnosis was made within 3 months (90 days) of the initial brain MRI assessment. Twenty-one patients (11.6 %) had more than 3 months of prodrome II (Fig. 1). We excluded four patients from a delayed diagnosis group because a surgical biopsy could not be performed due to the refusal of the patient or medical comorbidity although it was strongly recommended before 3 months from initial MRI. Therefore, 17 patients (9.4 %) had their diagnosis delayed more than 3 months from the initial MRI. The yearly distribution of patients with a delayed diagnosis is depicted in Fig. 2. There was a clear decrease of incidence of delayed diagnosis after 2007.
Review of medical record
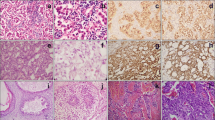
The medical records of the 17 patients, including radiological images, surgical records, and laboratory data, were collected and reviewed. The patients were categorized into three groups based on the tumor location: suprasellar, pineal, and basal ganglia. Patients with bifocal tumors (i.e., in both suprasellar and pineal areas) were grouped with patients with suprasellar tumors because of their similar symptomatology and initial radiological findings. The clinical features of the groups were described separately. Radiological images were reviewed by neuroradiologists (Kim I-O and Cheon J-E). The brain MRIs of patients with basal ganglia GCTs were classified according to a previously proposed scheme [9]: type I, a subtle patchy lesion mainly visible in T2-weighted images with faint or no contrast enhancement; type II, a small lesion (<3 cm in diameter) with contrast enhancement; type III, a small lesion with subependymal seeding and contrast enhancement; and type IV, a large lesion (≥3 cm in diameter).
If pathologic polyuria (exceeding 2 L/m2/24 h) was present, a CDI diagnosis was established if the serum osmolality was greater than 300 mOsm/kg and the urine osmolality was less than 300 mOsm/kg. Precocious puberty was defined as the onset of secondary sexual characteristics (i.e., breast development in girls and testis and/or phallus enlargement in boys) before 8 years in girls and 9 years in boys [10].
Acquisition of survival data and statistical analysis
The survival data of patients with germinoma (N = 119; including 13 patients with a delayed diagnosis) were acquired from the medical records. The event-free survival (EFS) was defined as the time interval from the day in which a clinical diagnosis was made to the date of the documentation of disease progression or development of life-threatening treatment-related complications, whichever came first. The overall survival (OS) was defined as the time interval between the day of a clinical diagnosis to the date of death or March 21, 2013, whichever came first.
For a nonparametric test for continuous variables between three groups, a Kruskal–Wallis test was applied. A Kaplan–Meier method was used for survival analyses and a log-rank test was used for comparison of EFS and OS between groups. All P values were two-sided and significance was set at P = 0.05. MedCalc version 12.4.0 (MedCalc, Ostend, Belgium; a free-trial version) was used for Kruskal–Wallis test, and IBM SPSS version 19.0 software (IBM, Armonk, NY) was used for log-rank tests.
Results
Location, age, and sex
For the 17 patients with a delayed diagnosis, the location of the tumor at the time of the definitive diagnosis was as follows: suprasellar area (9 patients including 3 patients with bifocal tumors), basal ganglia (6 patients), and pineal region (2 patients). The proportion of a delayed diagnosis in each location group was 14.8 % [9/(38 + 23)] for the suprasellar group including bifocal tumors, 20.7 % (6/29) for the basal ganglia group, and 2.5 % for the pineal group (2/81).
Four patients were female, and 13 patients were male. The median age at diagnosis was 13 years (range, 8–29 years). The distribution of sex and age was highly associated with tumor location. The four female patients had suprasellar GCTs, whereas all the patients with basal ganglia and pineal GCTs were male. The clinical characteristics of the 17 patients are summarized in Table 1.
Symptomatology
The initial symptoms and signs were associated with the tumor location groups. Eight patients with suprasellar GCTs (including two patients with bifocal GCTs) presented with polyuria and polydipsia, which is indicative of CDI. One patient who later developed bifocal GCTs presented with blurred vision without CDI. Five patients with basal ganglia GCTs initially developed hemiparesis, and one patient presented with recurrent vomiting and hiccups. Two patients with pineal GCTs initially sought medical attention because of precocious puberty.
Initial MRI and progression
In the suprasellar group, an initial brain MRI showed no specific abnormality in one patient, bright signal loss of the posterior hypophysis only in two patients, and a thickened pituitary stalk (TPS) in six patients (i.e., equivocal thickening in three patients and overt thickening in three patients). In the basal ganglia group, all the patients demonstrated lesions in the basal ganglia. Five patients had subtle non-enhancing lesions that corresponded to type I tumors and one patient had small contrast-enhancing lesions that corresponded to type II tumors. The initial brain MRIs of the two patients in the pineal group revealed no specific abnormalities.
All the patients had at least one more MRI examination before the definitive diagnosis (median number of brain MRIs, 3; range, 2–5). The median interval between the initial MRIs and the definitive diagnosis (prodrome II) was 13 months (range, 3–64 months). There was no significant difference in prodrome II among the three location groups (P = 0.664; Kruskal–Wallis test).
Fourteen patients showed disease progression during the radiological follow-up. In the suprasellar group, five patients later developed a suprasellar mass or a more prominent TPS. One patient with an initial loss of the bright signal of the posterior hypophysis developed bifocal tumors 7 month later. Two patients with an equivocal TPS at presentation developed bifocal tumors 8 and 24 months later. One of the patients also had multiple subependymal seedings at follow-up (Fig. 3). One patient had no change in an overt TPS for 3 months before the definitive diagnosis. In the basal ganglia group, four patients with initial type I lesions developed contrast-enhancing lesions after 9–30 months. Two of these patients had bilateral basal ganglia lesions and later developed subependymal seedings (Fig. 4). The patient with initial type II lesions had no change in the initially detected basal ganglia lesions for 15 months. The two patients in the pineal group developed a pineal mass 10 and 26 months after the initial normal MRI.
Serial MRIs of a 15-year-old boy presenting with polyuria and polydipsia (case no. 4). a An initial T1-weighted MR image shows the loss of the hyperintense signal of the posterior hypophysis (arrow). b The pituitary stalk showed an equivocal thickening and enhancement on a contrast-enhanced T1-weighted image, but c there was no remarkable change after 1 year of follow-up. d The MRI at the 2-year follow-up reveals a thickened pituitary stalk (arrow) and seeding in the third ventricle (arrowhead)
MRIs of a 13-year-old boy presenting with hemiparesis (case no. 12). b An initial T2-weighted image reveals small patchy lesions in the bilateral basal ganglia. There is also a mild focal thickening of the interventricular septum. b The MRI after 30 months demonstrates a large contrast-enhancing mass in the right basal ganglia and seeding in the interventricular septum (arrow)
Tumor markers
An initial serum tumor marker (i.e., β-HCG and AFP) study was performed in seven patients (i.e., three in the suprasellar group, two in the pineal group, and two in the basal ganglia group). The initial CSF tumor marker levels were measured in one patient with overt stalk thickening. All the initial tumor marker studies were within the normal limits except for one patient in the pineal group who had an elevated serum β-HCG level (46 mIU/ml).
At the definitive diagnosis, the serum tumor marker study was performed in all patients and the CSF tumor marker levels were evaluated in 12 patients. In the suprasellar group, the serum and CSF tumor marker levels were within normal limits in 7 patients. One patient (case no. 1) had elevated serum and CSF β-HCG and one patient with bifocal mixed GCT (case no. 9) had elevated serum β-HCG and AFP. In the basal ganglia group, the serum tumor markers were normal in five patients at definitive diagnosis. Two patients (case no. 10 and 11) had slightly elevated CSF β-HCG levels (14 and 12 mIU/ml, respectively) and one patient (case no. 12) had highly elevated β-HCG levels (serum, 92 mIU/ml; CSF, 810 mIU/ml) at definitive diagnosis. One patient with a pineal choriocarcinoma demonstrated an exponential increase in serum and CSF β-HCG levels. The other patient with a pineal immature teratoma had elevated β-HCG (serum, 13.2 mIU/ml; CSF, 31.1 mIU/ml) and AFP (serum, 62.6 ng/ml; CSF, 68.8 ng/ml) levels at the definitive diagnosis.
Diagnosis
Fifteen patients underwent a scheduled surgical biopsy. The surgical approach was mainly determined by the tumor location and topology. For patients in the suprasellar group, open (three patients), endoscopic (three patients), and transsphenoidal (two patients) biopsies were applied. All basal ganglia lesions were biopsied via a stereotactic method. One patient with a pineal lesion received an endoscopic biopsy. The other patient with a pineal lesion received an urgent tumor resection due to tumor bleeding. One patient was diagnosed with a mixed GCT without a surgical biopsy due to highly elevated serum and CSF AFP levels. CSF cytological analyses were performed in four patients before the definite diagnosis of GCT, and all were negative for malignant cells.
Thirteen patients were eventually diagnosed with a germinoma. All the patients in the suprasellar group (including the two bifocal) were diagnosed with a germinoma except for the patient described above with bifocal mixed GCTs. Five patients with basal ganglia tumors had a germinoma, and one patient had bilateral mixed GCTs. Two patients with pineal tumors were diagnosed with a choriocarcinoma or an immature teratoma.
Pineal GCT with precocious puberty
Two boys who presented with precocious puberty initially had nondiagnostic brain MRIs and later developed pineal GCTs. A 7-year-old boy (case no. 16) visited the hospital for the evaluation of an enlarged phallus and voice change. He had serum testosterone values in the early pubertal range. However, the peak levels of luteinizing hormone and follicle-stimulating hormone after stimulation with gonadotropin-releasing hormone (GnRH) were in the prepubertal range. Thus, he was diagnosed with peripheral precocious puberty and began taking medroxyprogesterone. Although the serum β-HCG level was elevated to 46 mIU/ml, the initial brain MRI showed no abnormal contrast-enhancing lesions. A nodular enhancement was observed in the pineal area, concordant with normal pineal enhancement. Serial serum β-HCG levels fluctuated between 30 and 50 mIU/ml during 6 months of follow-up, and the second follow-up MRI showed no pineal enhancement change. At the 8 months of follow-up, the serum and CSF β-HCG levels had risen to 397 and 933 mIU/ml, respectively. The serum and CSF AFP levels were within the reference value range. Two months after the second MRI, he was transferred to the emergency room for a sudden headache and drowsy mentality. Computed tomography (CT) scans revealed an acute intraventricular hemorrhage (IVH) and hydrocephalus. Extraventricular drainage was immediately performed. A brain MRI showed an IVH and a hemorrhagic mass in the pineal area (Fig. 5). The serum β-HCG level was elevated to 11,510 mIU/ml. The pineal mass was subtotally removed, and a pathological examination revealed a choriocarcinoma.
Serial MRIs of an 7-year-old boy presenting with precocious puberty (case no. 16). a A contrast-enhanced T1-weighted image at initial presentation shows a slight prominent enhancement of the pineal gland (arrow); however, it is compatible with normal pineal enhancement. b The MRI after 8 months shows virtually no significant change of the pineal area, but for a slightly prominent enhancement pattern. c A CT scan at the catastrophe after 10 months of initial presentation shows bleeding in the pineal area and intraventricular hemorrhage. d A contrast-enhanced T1-weighted image reveals a hemorrhagic mass in the pineal area
The other patient, a 6-year-old boy (case no. 17), developed pubic hair and an enlarged phallus. He was administered medroxyprogesterone for peripheral precocious puberty. No other causes of peripheral precocious puberty, such as adrenal or testicular disorders, were found. His β-HCG serum level (11 mIU/ml), which was slightly higher than the reference value at our institution (<10 mIU/ml), decreased to the normal range 1 year later. His pubertal signs gradually progressed, and gonadotropin showed pubertal response after GnRH stimulation at age 10 years. Because central precocious puberty followed peripheral precocious puberty, he was administered a GnRH agonist. The initial MRI and regular follow-up showed no abnormal contrast enhancement. Serum tumor markers remained within the normal limits during GnRH agonist therapy for the progressive central precocious puberty. At age 13 years, he suddenly developed headache, nausea, and diplopia. A brain MRI showed a large contrast-enhancing mass with a honeycomb structure in the pineal area and accompanying hydrocephalus. His serum AFP level was 62.6 ng/ml (reference value of our institution, <20 ng/ml), and his serum and CSF β-HCG levels were 13.2 and 31.1 mIU/ml. Endoscopic third ventriculostomy and tumor biopsy were performed. The pathological examination revealed a mature teratoma. Two weeks later, the patient received radical tumor resection and the pathological examination of the tumor revealed a Norris grade I immature teratoma.
Survival of patients with germinoma
In the whole patient cohort, 119 patients were diagnosed with germinoma. The survival of patients with germinoma and a delayed diagnosis (N = 13) was compared with those of patients who were diagnosed within 3 months (N = 106). There were only four patients with NGGCT in the delayed diagnosis group, and the diagnoses were also heterogeneous; no comparison of survival for NGGCT was made. There was no significant difference in EFS between the two groups (P = 0.221; log-rank test). However, the OS of germinoma patients with a delayed diagnosis was significantly shorter than those of other germinoma patients (P = 0.002; Fig. 6).
Discussion
Delay in the diagnosis is commonly observed for pediatric brain tumors [11]. Flores et al. [12] reported that delay in diagnosis was more significant for brain tumors than for other childhood malignancies. Young-age onset and atypical symptomatology may be the primal causes of delayed diagnosis, along with the lack of vigilance of medical personnel [13]. Sometimes, the indolent nature of brain tumor itself adds further difficulties to timely diagnosis of patients. The long-term latency of intracranial GCTs before diagnosis has been of interest to neuro-oncologists and endocrinologists. Suprasellar germinoma is the prototype of GCT latency. The association of CDI, thickening of the pituitary stalk, and normal serum tumor markers has been well-recognized, and together they constitute a syndrome of “occult” suprasellar germinoma. Mootha et al. [14] described six patients with occult suprasellar germinoma. Three of the patients had a TPS, but the initial MRIs of the three other patients were normal. The median time from presentation to the follow-up MRI with a notable change was 9.5 months (range, 3–14 months). Kato et al. [7] reported three patients in whom the initial MRI revealed only a loss of bright signal in the posterior hypophysis on T1-weighted images. Abnormal contrast-enhancing lesions appeared on the follow-up MRI after 12–50 months. Loss of the normal hyperintense signal of the posterior hypophysis may be an early sign of occult germinoma, but it is a nonspecific CDI finding [15–17].
In our study, the suprasellar group outnumbered the basal ganglia and pineal groups. The majority (eight patients) of the suprasellar group presented with CDI. It is known that 30–40 % of patients presenting with idiopathic CDI later progress to tumorous conditions such as germinoma or Langerhans cell histiocytosis [18, 19]. The serum β-HCG and AFP levels observed at initial presentation (three patients) and at the time of the surgical biopsy (seven patients) were within the normal range. Mootha et al. [14] also reported normal serum β-HCG levels in all patients with occult suprasellar germinoma. Interestingly, they reported an elevated CSF β-HCG level in one patient with a slightly thickened pituitary stalk at initial presentation. The authors further recommended a routine CSF examination for tumor markers and cytology when evaluating patients presenting with CDI and normal MRI or a TPS. However, it is unclear whether the CSF β-HCG study is helpful for the early diagnosis of germinomas in patients with CDI and a normal MRI or only a loss of the hyperintense signal of the posterior hypophysis. Leger et al. [20] recommended repeated MRI and tumor marker studies during the first 3 years following CDI onset because idiopathic TPS tended to spontaneously resolve, while the TPS of tumorous conditions progressed within 1.8 ± 1.6 years from the initial neuroimaging study. However, it is precarious to establish a time limit for radiological follow-up due to the report of a patient who developed a suprasellar germinoma 9 years after CDI onset and 4.5 years after the appearance of a TPS [21].
One interesting finding is that two patients who presented with CDI later developed bifocal GCTs in the suprasellar and pineal regions. The initial MRIs of these patients showed only the loss of a hyperintense signal in the posterior hypophysis or equivocal TPS. Bifocal tumor presentation in the suprasellar and pineal regions has been an unexplained phenomenon of intracranial GCT [22, 23]. Simultaneous tumor developments in both areas and metastasis from one site to the other have been proposed as the pathogenesis of bifocal tumors [24]. In our previous study, we supposed that metastatic spread is more likely than simultaneous development based on the demographic data and the high ventricular seeding rate in patients with bifocal GCTs [8]. The two patients who presented with CDI and developed bifocal tumors months later in this study may support the metastatic hypothesis of bifocal GCT. One of the patients developed multiple subependymal seeding, which also adds supporting evidence to this hypothesis.
Basal ganglia GCTs are also notorious for latent clinical courses and subtle imaging findings that prevent timely diagnoses [4, 25]. One study reported an 8-year asymptomatic history after the detection of a unilateral calcification in the basal ganglia that later progressed to a germinoma [26]. We previously reported the clinical course of 17 patients with basal ganglia germinoma and classified the initial MRI patterns [9]. Patients with subtle, non-enhancing abnormalities in the basal ganglia (so-called type I lesions) required a significantly longer time from the initial MRI to the pathological diagnosis. This situation is similar to suprasellar GCTs presenting with CDI and only the loss of a hyperintense signal of the posterior hypophysis. If a patient presents with hemiparesis and the MRI shows only a subtle abnormality of the basal ganglia in T2-weighted images, an urgent surgical biopsy may not be easily recommended. The usually normal serum tumor markers also provide little help in this situation. However, basal ganglia GCTs frequently show ancillary MRI findings such as atrophy of the basal ganglia and cerebral peduncle [27, 28]. These findings may be of great use in the early diagnosis of basal ganglia GCTs with subtle abnormalities [9]. Further investigations including 11C-methionine positron emission tomography and CSF tumor marker study could be useful for early diagnosis [25, 29].
Clinical latency and diagnostic delay may not be synonymous because the latter results from either the intrinsic characteristics of GCTs or from inappropriate application and interpretation of work-ups by clinicians. Actually, some of the patients in our study had a gadolinium-enhancing lesion on the initial MRI: three patients in the suprasellar group had overt TPS and one patient in the basal ganglia group had small enhancing nodules (type II lesion). Clinical experience of these patients may enable clinicians to cope with ambiguous MRI properly. We observed a clear decrease of the incidence of delayed diagnosis after 2007. This could be attributed to enhanced knowledge and vigilance of primary physicians on the disease who immediately refer suspicious patients to neurosurgeons. In our study, the survival outcome of 13 patients with germinoma and delayed diagnosis was significantly worse than those of the other 106 patients with germinoma who were diagnosed within 3 months from initial MRIs. It is possible that clinical factors other than diagnostic delay may influence the patients’ survival. However, it is also noteworthy that three germinoma patients who expired during the follow-ups developed overt tumor masses after diagnostic delay, whereas all patients without prominent changes on follow-up MRIs were alive (see Table 1). Therefore, proactive application of surgical biopsy is recommended for the patients with overt enhancing lesions because diagnostic delay can influence the survival of patients.
Two patients presented with precocious puberty and later developed overt pineal GCTs. Furthermore, they had an NGGCT and not a germinoma. To the best of our knowledge, this pattern of latency has not been reported for intracranial GCTs. Although the pineal gland of the patient with choriocarcinoma was slightly prominent, the initial MRI of this patient was essentially nondiagnostic. The rising β-HCG levels raised clinical suspicion; however, an open or stereotactic biopsy may be a challenging option for such a small, deep-situated area. The abrupt enlargement and spontaneous bleeding of a tumor after a rather long radiological latency is intriguing. These two patients present a novel clinical pattern of intracranial GCTs and demonstrated that the GCT clinical latency is not restricted to suprasellar and basal ganglia germinoma, and it is a general feature of intracranial GCTs in all locations.
At present, clinical latency mechanism of intracranial GCTs is unknown. Oosterhuis et al. [30] clarified that GCTs found in the whole body are strictly coordinated by genetic/epigenetic programs of germ cell development. The majority of intracranial GCTs arise in late childhood and during the teenage years. It is also noteworthy that intracranial GCTs differ in the age of onset and location according to the patient’s sex—female patients are younger than male patients at diagnosis. Ectopic primitive germ cells in the brain can proliferate at the original site, causing various site-specific symptomatologies; however, they may need further environmental cues, i.e., hormonal stimulation, to unleash full-blown tumorigenesis when the patient reaches a critical age threshold. Precocious puberty in GCTs is generally attributed to the secretion of β-HCG from the tumor; however, precocious puberty itself may precipitate the development of GCT in cases with initial normal MRIs and normal β-HCG levels. Whether these conjectures are true needs to be verified in further research.
Conclusions
About 10 % of patients with intracranial GCTs present with insidious symptoms, and the diagnosis is delayed. Clinical latency and delayed diagnosis are not restricted to germinomas in the suprasellar area and basal ganglia. They are canonical features of intracranial GCTs including pineal non-germinomatous GCTs. Early detection and proactive diagnosis of these tumors are required because diagnosis delay may negatively influence patient survival.
References
Cho KT, Wang KC, Kim SK, Shin SH, Chi JG, Cho BK (2002) Pediatric brain tumors: statistics of SNUH, Korea (1959–2000). Childs Nerv Syst 18(1–2):30–37
Goodwin TL, Sainani K, Fisher PG (2009) Incidence patterns of central nervous system germ cell tumors: a SEER study. J Pediatr Hematol Oncol 31(8):541–544
Matsutani M, Sano K, Takakura K, Fujimaki T, Nakamura O, Funata N, Seto T (1997) Primary intracranial germ cell tumors: a clinical analysis of 153 histologically verified cases. J Neurosurg 86(3):446–455
Sonoda Y, Kumabe T, Sugiyama S, Kanamori M, Yamashita Y, Saito R, Ariga H, Takai Y, Tominaga T (2008) Germ cell tumors in the basal ganglia: problems of early diagnosis and treatment. J Neurosurg Pediatr 2(2):118–124
Crawford JR, Santi MR, Vezina G, Myseros JS, Keating RF, LaFond DA, Rood BR, MacDonald TJ, Packer RJ (2007) CNS germ cell tumor (CNSGCT) of childhood: presentation and delayed diagnosis. Neurology 68(20):1668–1673
Birnbaum T, Pellkofer H, Buettner U (2008) Intracranial germinoma clinically mimicking chronic progressive multiple sclerosis. J Neurol 255(5):775–776
Kato T, Sawamura Y, Tada M, Murata J, Abe H, Shirato H, Fujieda K (1998) Occult neurohypophyseal germinomas in patients presenting with central diabetes insipidus. Neurosurg Focus 5(1):e6
Phi JH, Kim SK, Lee J, Park CK, Kim IH, Ahn HS, Shin HY, Kim IO, Jung HW, Kim DG, Paek SH, Wang KC (2013) The enigma of bifocal germ cell tumors in the suprasellar and pineal regions: synchronous lesions or metastasis? J Neurosurg Pediatr 11(2):107–114
Phi JH, Cho BK, Kim SK, Paeng JC, Kim IO, Kim IH, Kim DG, Jung HW, Kim JE, Wang KC (2010) Germinomas in the basal ganglia: magnetic resonance imaging classification and the prognosis. J Neurooncol 99(2):227–236
Carel JC, Leger J (2008) Clinical practice. Precocious puberty. N Engl J Med 358(22):2366–2377
Dobrovoljac M, Hengartner H, Boltshauser E, Grotzer MA (2002) Delay in the diagnosis of paediatric brain tumours. Eur J Pediatr 161(12):663–667
Flores LE, Williams DL, Bell BA, O’Brien M, Ragab AH (1986) Delay in the diagnosis of pediatric brain tumors. Am J Dis Child 140(7):684–686
Edgeworth J, Bullock P, Bailey A, Gallagher A, Crouchman M (1996) Why are brain tumours still being missed? Arch Dis Child 74(2):148–151
Mootha SL, Barkovich AJ, Grumbach MM, Edwards MS, Gitelman SE, Kaplan SL, Conte FA (1997) Idiopathic hypothalamic diabetes insipidus, pituitary stalk thickening, and the occult intracranial germinoma in children and adolescents. J Clin Endocrinol Metab 82(5):1362–1367
De Buyst J, Massa G, Christophe C, Tenoutasse S, Heinrichs C (2007) Clinical, hormonal and imaging findings in 27 children with central diabetes insipidus. Eur J Pediatr 166(1):43–49
Hamilton BE, Salzman KL, Osborn AG (2007) Anatomic and pathologic spectrum of pituitary infundibulum lesions. AJR Am J Roentgenol 188(3):W223–W232
Shin JH, Lee HK, Choi CG, Suh DC, Kim CJ, Hong SK, Na DG (2001) MR imaging of central diabetes insipidus: a pictorial essay. Korean J Radiol 2(4):222–230
Chung SJ, Lee SY, Shin CH, Yang SW (2007) Clinical, endocrinological and radiological courses in patients who was initially diagnosed as idiopathic central diabetes insipidus. Korean J Pediatr 50(11):1110–1115
Maghnie M, Cosi G, Genovese E, Manca-Bitti ML, Cohen A, Zecca S, Tinelli C, Gallucci M, Bernasconi S, Boscherini B, Severi F, Arico M (2000) Central diabetes insipidus in children and young adults. N Engl J Med 343(14):998–1007
Leger J, Velasquez A, Garel C, Hassan M, Czernichow P (1999) Thickened pituitary stalk on magnetic resonance imaging in children with central diabetes insipidus. J Clin Endocrinol Metab 84(6):1954–1960
Bettendorf M, Fehn M, Grulich-Henn J, Selle B, Darge K, Ludecke DK, Heinrich UE, Saeger W (1999) Lymphocytic hypophysitis with central diabetes insipidus and consequent panhypopituitarism preceding a multifocal, intracranial germinoma in a prepubertal girl. Eur J Pediatr 158(4):288–292
Cuccia V, Alderete D (2010) Suprasellar/pineal bifocal germ cell tumors. Childs Nerv Syst 26(8):1043–1049
Lafay-Cousin L, Millar BA, Mabbott D, Spiegler B, Drake J, Bartels U, Huang A, Bouffet E (2006) Limited-field radiation for bifocal germinoma. Int J Radiat Oncol Biol Phys 65(2):486–492
Lee L, Saran F, Hargrave D, Bodi I, Bassi S, Hortobagyi T (2006) Germinoma with synchronous lesions in the pineal and suprasellar regions. Childs Nerv Syst 22(12):1513–1518
Sudo A, Shiga T, Okajima M, Takano K, Terae S, Sawamura Y, Ohnishi A, Nagashima K, Saitoh S (2003) High uptake on 11C-methionine positron emission tomographic scan of basal ganglia germinoma with cerebral hemiatrophy. AJNR Am J Neuroradiol 24(9):1909–1911
Takeda N, Fujita K, Katayama S, Uchihashi Y, Okamura Y, Nigami H, Hashimoto K, Kohmura E (2004) Germinoma of the basal ganglia. An 8-year asymptomatic history after detection of abnormality on CT. Pediatr Neurosurg 40(6):306–311
Okamoto K, Ito J, Ishikawa K, Morii K, Yamada M, Takahashi N, Tokiguchi S, Furusawa T, Sakai K (2002) Atrophy of the basal ganglia as the initial diagnostic sign of germinoma in the basal ganglia. Neuroradiology 44(5):389–394
Ozelame RV, Shroff M, Wood B, Bouffet E, Bartels U, Drake JM, Hawkins C, Blaser S (2006) Basal ganglia germinoma in children with associated ipsilateral cerebral and brain stem hemiatrophy. Pediatr Radiol 36(4):325–330
Lee J, Lee BL, Yoo KH, Sung KW, Koo HH, Lee SJ, Choi JY, Lee KH, Lee JI, Shin HJ, Kim JH, Suh YL, Lee KH, Lee M (2009) Atypical basal ganglia germinoma presenting as cerebral hemiatrophy: diagnosis and follow-up with 11C-methionine positron emission tomography. Childs Nerv Syst 25(1):29–37
Oosterhuis JW, Stoop H, Honecker F, Looijenga LH (2007) Why human extragonadal germ cell tumours occur in the midline of the body: old concepts, new perspectives. Int J Androl 30(4):256–263
Acknowledgments
This study was supported by a grant from the Clinical Medical Scientist R&D Project, Ministry for Health, Welfare, and Family Affairs, Republic of Korea (grant no. A102053; to J.H. Phi).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Phi, J.H., Kim, SK., Lee, Y.A. et al. Latency of intracranial germ cell tumors and diagnosis delay. Childs Nerv Syst 29, 1871–1881 (2013). https://doi.org/10.1007/s00381-013-2164-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2164-y