Abstract
Purpose
The anatomy of the pedicle is complex and three-dimensional; however, there are basic dimensions important for possible screw placement. There are relatively few studies examining the pedicle anatomy in children. This study was performed to evaluate the feasibility of pedicle screw placement in children aged 5–16, based on key anatomic dimensions. A case illustration is also provided.
Methods
The CT scans of 102 consecutive children were studied. Patients with abnormal anatomy were excluded. The parameters of the pedicle isthmus width (W), estimation of screw length (L), and axial angle (A) were recorded for 1,632 pedicles from T10 through L5. Patients were divided into four age groups. Statistical analysis was performed evaluating the difference between males and females and of the particular anatomy at the thoracolumbar junction.
Results
The pedicles increase in both L and W from T10–T12 and from L1–L5. L1 has a consistently smaller W compared to T12 in both genders over all age ranges. Estimating a W of 4.5 mm necessary for safe screw placement, we calculate that virtually all pedicles of T12 and L3–L5 are large enough for screw placement in both genders after age 8. L4 and L5 are large enough for screw placement in both genders in the youngest age range.
Conclusions
Most of the pedicles of the lower lumbar spine and T12 are large enough to house the smallest commercially available screw. Understanding of the anatomy at the thoracolumbar junction is important, as the W of L1 is consistently smaller than T12.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pedicle screw fixation is a mainstay of adult spine surgery. Pedicle screws offer a number of advantages, including three-column fixation, stability over short segment fusions, and reduced pseudoarthrosis rates compared to other forms of instrumentation [2, 11, 14, 18, 23, 25, 29]. However, the anatomy of a child may make screw placement difficult.
The pedicle size and anatomy has been thoroughly studied in adults. However, there are few studies in children. In this study, we evaluate the pedicle dimensions germane to screw placement based on CT scan at the lower thoracic and lumbar spine. We divide patients by gender and into four age groups. The study was performed to give an estimation of the age and level where the pedicle size is large enough to safely house the smallest diameter commercially available screw.
Methods
We reviewed the fine-cut CT scans of 102 consecutive children (56 male and 46 female) aged 5–16 years. The study period was from 2008 to 2011. We excluded patients with conditions potentially causing abnormal anatomy, such as scoliosis or spinal dysraphism. The CT scans were performed as part of the clinical evaluation of patients for trauma, back pain, or abdominal pathology. All patients were eligible for the study provided that the scans had sufficient quality high-resolution sagittal and axial images of the lower thoracic and lumbar spine.
The patients were divided into four groups based on age: group A (5–7 years), B (8–10 years), C (11–13 years), and D (14–16 years). The patients were also divided by sex. Individual measurements of all pedicles were performed using the integrated software inherent in the Synapse Multiview system, version 3.2.15111.0 (Fujifilm Medical Systems, Stamford, CT, USA). We recorded three measurements germane to pedicle screw placement:
-
Pedicle width (W) defined as the pedicle isthmus, the most narrow outer cortical dimension of the pedicle in an axial plane
-
Length (L) defined as the length from the laminar cortex through the center of the pedicle to the inner cortex of the vertebral body; this measurement provides an estimation of the potential screw length
-
Axial angle (A) defined as the angle between L and a vertical line from the center of the vertebral body through the center of the spinous process.
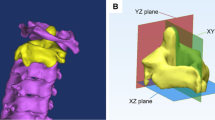
A representation of these measurements is shown in Fig. 1.
The growth was estimated by calculating the percentage change across age groups. For example, the percentage change in W from groups A to B was calculated by (W B − W A)/W A.
The three measurements were performed on all pedicles from T10–L5. A total of 1,632 pedicles were measured. Statistical analysis was performed using Microsoft Excel for windows. Comparison between groups was performed using either a one- or two-tailed Student’s t test with clinical significance (p) set at 0.05. Data points were tabulated with a mean and 95 % confidence interval.
The study began after approval from the local Institutional Review Board.
Results
The study consisted of anatomic measurements of 1,632 pedicles in 102 patients. There were 56 male and 46 female patients. Both the right and left pedicles were measured in each patient from the T10 through the L5 level. The number of pedicles evaluated for each age group is shown in Table 1.
Table 2 shows the male and female mean value and 95 % confidence intervals for W across the four age groups. In group A, females had a statistically significantly smaller W for T11–L5 levels compared to males. W was statistically similar between males and females in groups B and C. Males again showed a significantly greater W for all spinal levels except T12 and L5 in group D.
Table 3 shows the male and female mean value and 95 % confidence intervals for L across the four age groups. Males had a significantly longer L for all levels in group A except L1. L was shorter in females at T10 and T11 for groups A, B, and C. The L4 and L5 levels had statistically similar values for L in groups B, C, and D.
Table 4 shows the male and female mean value and 95 % confidence intervals for A across the four age groups. There were differences in A between males and females at the T10, T11, and L5 levels in group A. A was statistically similar between males and females at all levels in groups B, C, and D, with the exception of L2 in group C.
The mean values for W, L, and A for males are graphed in Fig. 2. W and L show growth through the age groups. A remains similar for the respective level between age groups. The mean values for W, L, and A for females are graphed in Fig. 3. W and L show growth most prominently between groups A and B at all levels. A remains relatively stable over all age groups.
The rate of growth for W and L for males is shown in Fig. 4. This graph shows the percentage change in dimension as the child moves from one age group to the next. The highest percentage of change of W for the thoracic and upper lumbar levels occurs as the age range moves from group A to B, except at T10. The lower lumbar levels show fairly consistent growth over the age groups. For L, the highest percentage of growth for the thoracic and most of the lumbar spine occurs from group A to B. However, L5 shows a higher rate of growth between groups C and D.
A similar chart for females is shown in Fig. 5. The value for W shows the highest percentage of growth from group A to B at all anatomic levels. This is also true for L, although there is pronounced growth from group B to C at the L5 level.
In both genders, the thoracic W and L increase from T10 to T12. This is also true in the lumbar levels, with increasing size from L1 to L5. However, there is a transition point from T12 to L1. This is shown in Table 5. The W of T12 is larger than L1 for both genders at all age groups. This reaches statistical significance for all groups except group B in males. However, the L of L1 is longer than T12 for both genders across all age groups.
The percent of pedicles with W >4.5 mm is shown in Table 6. This provides an estimation of the level and age where a surgeon can safely place a pedicle screw. Virtually all pedicles in L3–L5 were large enough for a screw in all age groups. T12 had a higher percentage of pedicles above 4.5 mm compared to L1 in all age groups. Relatively few T10 and T11 pedicles had W >4.5 mm in group A.
Case illustration
A 9-year-old otherwise healthy female was admitted to Riley Hospital for Children in Indianapolis, Indiana for multisystem trauma resulting from a motor vehicle accident. She was a restrained passenger wearing a lap belt only.
Her initial examination was significant for severe pain in the abdomen and back. She was neurologically intact. The trauma team performed an emergent exploratory laparotomy after imaging showed a retroperitoneal hematoma and suggested bowel injury.
Spine imaging showed a flexion distraction injury at the L1–2 level, with an endplate fracture of L1. MRI showed soft tissue injury, widened facet joints, and disruption of the facet capsules (Fig. 6a, b). CT scan showed a widened interspinous distance (Fig. 6c) and “perched” facets (Fig. 6d).
We felt that the patient had an unstable injury and required surgical correction. We were also concerned about the relative lack of bony injury compared to the extensive soft tissue damage. Therefore, we felt that rigid fixation was appropriate. Since the injury was localized to the L1–L2 level, we felt we could adequately fixate with a short segment fusion. We evaluated the pedicle size, finding W to 4.5 mm at L1 and 4.8 mm at L2.
Once the patient medically stabilized, we performed an open-reduction and posterolateral fusion with pedicle screw fixation using adult cervical lateral mass screws at L1 and L2 bilaterally. The screw width was 3.5 mm. Postoperative CT scans are shown in Fig. 7 in the sagittal (A) and axial (B) planes. The patient was mobilized on postoperative day 1. She was discharged to rehab. She was pain free and neurologically intact at her follow-up examinations at 6 weeks and 3 months.
Discussion
Pedicle screw fixation has a number of advantages over other fusion techniques in the pediatric spine. Pedicle screws offer immediate stabilization, a firm anchor point, improved ability to correct deformity, ability to provide compressive force, three-column fixation, and lower pseudoarthrosis rate compared to other forms of instrumentation [2, 11, 14, 18, 23, 25, 29]. Radiographic and clinical outcomes are acceptable in the few published papers describing screw placement in young children [23, 26].
As shown in the case illustration, pedicle screws provide three-column fixation over a short segment fusion. This is an advantage over hook or wire constructs. In younger children, the neurocentral synchondrosis is a potential weak area in the transmission of force from the posterior elements to the vertebral body [26]. A laminar hook/wire requires intact posterior elements and also encroaches slightly into the spinal canal, whereas a pedicle screw contained in the cortex does not.
There are potential disadvantages to pedicle screw fixation. In younger children, properly placing the screw in anatomically small areas may be challenging. This is especially true in the thoracic spine and thoracolumbar junction. Poorly positioned screws may have diminished strength or injure critical structures [5, 9]. The risk of misplaced screws is likely underestimated in the literature, but estimates are approximately 4.2–15 % of screws [11]. Screws breaking through the anterior vertebral body wall may cause vascular injury, especially in the lower thoracic spine [13, 20, 28, 33]. Laterally malpositioned screws may have decreased strength or injure vital anatomic structures, such as the lung, segmental vessels, sympathetic chain, or aorta, depending on the level of the screw [31]. Screws breaking through the medial pedicle wall may cause a vascular injury, dural laceration, or injure nervous structures.
The pedicle is a complex, three-dimensional structure. However, there are a few basic parameters (Fig. 1) that can be used to evaluate the safety of screw placement and screw size. Note that these parameters must be individualized. Pedicles may be dilated for screw placement [23, 34]. In the thoracic spine, some surgeons will accept pedicle-rib fixation or perform an “in-out-in” technique of pedicle cannulation. However, these techniques risk injury to surrounding structures [32]. Some authors will state that there is a medial “safe zone” of approximately 2–4 mm, where a medial cortical breach is unlikely to cause neurologic injury. However, most authors (ourselves included) judge the accuracy of placement as the screw completely contained within the cortices of the pedicle [3, 15, 16].
While there are a number of anatomic or radiographic studies detailing thoracolumbar pedicle anatomy in adult patients [1, 4, 6–8, 12, 17, 19, 22, 24, 30, 35], there are few in children. Ferree [10] published a similar study examining the spine in abdominal CT images in 1992. This paper evaluated the morphometric characteristics of 203 CT scans, with scan slice thicknesses of up to 15 mm. This paper suggested that the pedicles reach their final size by approximately 16 years of age [10]. O’Brien et al. [21] examined the thoracic CT scans of 29 scoliosis patients and concluded that pedicle screw instrumentation was feasible in most thoracic levels of adolescents. Senaran et al. examined the CT images of 21 patients aged 5–10 years old. They found that the inner diameter of the pedicles allowed safe placement of commercially available screws in L4–L5 in children 5 years or older, and at L3–L5 in older children. They did not differentiate size based on the patient’s sex [27]. Zindrick et al. [36] performed an anatomic study on 75 pediatric cadaver skeletal specimens. In contrast to our data, they did not find a gender difference in the measured dimensions. They showed that the pedicle isthmus was largest at L5, but that there was a wide variation at each vertebral level.
The smallest dimension for screw consideration is the pedicle isthmus, or W. This provides an estimate of the largest diameter screw that can be used [21]. The smallest commercially available screws have a diameter of 3.5 mm. In our illustrative case, 3.5-mm adult cervical lateral mass screws were used for pedicle fixation. We estimated a 0.5-mm buffer zone on either side for safe screw placement. Therefore, we evaluated what age had a W of 4.5 mm or greater. As shown in Table 6, virtually all pedicles from L3–L5 in both males and females were large enough for a screw. By age 11 (Group C), most of the pedicles at the lower thoracic and upper lumbar levels were large enough for a screw. A high percentage of pedicles in group B were large enough for screws. At the thoracolumbar junction, T12 was large enough to hold a screw in virtually all pedicles in groups B, C, and D, and in most of the pedicles of group A. The anatomy at the thoracolumbar junction is of particular note. As shown in Table 5, the pedicle W is generally smaller in L1 compared to T12, although the L is longer.
The largest change in parameters was observed between groups A and B (Figs. 4 and 5). This was especially noticeable in females. As the age increased above 14 (groups C to D), the growth leveled in females, whereas it continued to increase in males.
The length (L) increased slightly from T10 through L5 in both genders. The angle (A) of screw placement varied with level, but remained very stable over all age groups (Figs. 2 and 3). A was approximately 10° or less from T10–L2 in both males and females. A widened toward the lower lumbar levels, reaching approximately 30 at L5.
Limitations
While most consider the CT scan to be the most accurate radiologic assessment of bony anatomy, there is a possibility that signal averaging may cause an underestimation of pedicle size. Previous papers have highlighted this concern [21]. However, these studies were generally done on older generation scanners. We feel that this is minimized with current technology. We also agree with previous authors that there is a wide variability in pedicle size. We have tried to minimize this by including a large number of patients. Our estimation of the W capable of accepting a screw is based on our preference of keeping the screw completely within the cortices. Sequential dilation of the pedicle may be performed, although this procedure has its own risks and benefits. Our study is focused on patients with “normal” anatomy. Individual analysis of patients with abnormal anatomy from scoliosis or dysraphism is necessary.
Conclusions
The pedicle anatomy is complex and three-dimensional. Parameters important to pedicle screw placement include the measurement of the pedicle isthmus or width (W). The length L allows an estimate of screw length. In our study, a high percentage of the pedicles from T10–L5 were large enough to house a 3.5-mm screw once the patient reached 8 years of age. In the youngest age group, virtually all of the lower lumbar pedicles (L3–L5) were large enough for screw placement. The highest percentage of growth across age groups occurred between groups A (5–7 years) and B (8–10 years). The anatomy of between T12 and L1 is of note. The W of L1 is consistently smaller than T12. The surgeon must take this into consideration when considering screw fixation near the thoracolumbar junction.
References
Banta CJ 2nd, King AG, Dabezies EJ, Liljeberg RL (1989) Measurement of effective pedicle diameter in the human spine. Orthopedics 12:939–942
Barr SJ, Schuette AM, Emans JB (1997) Lumbar pedicle screws versus hooks. Results in double major curves in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 22:1369–1379
Belmont PJ Jr, Klemme WR, Dhawan A, Polly DW Jr (2001) In vivo accuracy of thoracic pedicle screws. Spine (Phila Pa 1976) 26:2340–2346
Berry JL, Moran JM, Berg WS, Steffee AD (1987) A morphometric study of human lumbar and selected thoracic vertebrae. Spine (Phila Pa 1976) 12:362–367
Brown CA, Lenke LG, Bridwell KH, Geideman WM, Hasan SA, Blanke K (1998) Complications of pediatric thoracolumbar and lumbar pedicle screws. Spine (Phila Pa 1976) 23:1566–1571
Cinotti G, Gumina S, Ripani M, Postacchini F (1999) Pedicle instrumentation in the thoracic spine. A morphometric and cadaveric study for placement of screws. Spine (Phila Pa 1976) 24:114–119
Ebraheim NA, Rollins JR Jr, Xu R, Yeasting RA (1996) Projection of the lumbar pedicle and its morphometric analysis. Spine (Phila Pa 1976) 21:1296–1300
Ebraheim NA, Xu R, Ahmad M, Yeasting RA (1997) Projection of the thoracic pedicle and its morphometric analysis. Spine (Phila Pa 1976) 22:233–238
Faraj AA, Webb JK (1997) Early complications of spinal pedicle screw. Eur Spine J 6:324–326
Ferree BA (1992) Morphometric characteristics of pedicles of the immature spine. Spine (Phila Pa 1976) 17:887–891
Hicks JM, Singla A, Shen FH, Arlet V (2010) Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976) 35:E465–E470
Hou S, Hu R, Shi Y (1993) Pedicle morphology of the lower thoracic and lumbar spine in a Chinese population. Spine (Phila Pa 1976) 18:1850–1855
Kakkos SK, Shepard AD (2008) Delayed presentation of aortic injury by pedicle screws: report of two cases and review of the literature. J Vasc Surg 47:1074–1082
Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K (2004) Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:2040–2048
Kim YJ, Lenke LG, Cheh G, Riew KD (2005) Evaluation of pedicle screw placement in the deformed spine using intraoperative plain radiographs: a comparison with computerized tomography. Spine (Phila Pa 1976) 30:2084–2088
Lehman RA Jr, Lenke LG, Keeler KA, Kim YJ, Cheh G (2007) Computed tomography evaluation of pedicle screws placed in the pediatric deformed spine over an 8-year period. Spine (Phila Pa 1976) 32:2679–2684
Li B, Jiang B, Fu Z, Zhang D, Wang T (2004) Accurate determination of isthmus of lumbar pedicle: a morphometric study using reformatted computed tomographic images. Spine (Phila Pa 1976) 29:2438–2444
Liljenqvist U, Hackenberg L, Link T, Halm H (2001) Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg 67:157–163
Misenhimer GR, Peek RD, Wiltse LL, Rothman SL, Widell EH Jr (1989) Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine (Phila Pa 1976) 14:367–372
Mulpuri K, Perdios A, Reilly CW (2007) Evidence-based medicine analysis of all pedicle screw constructs in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 32:S109–S114
O’Brien MF, Lenke LG, Mardjetko S, Lowe TG, Kong Y, Eck K, Smith D (2000) Pedicle morphology in thoracic adolescent idiopathic scoliosis: is pedicle fixation an anatomically viable technique? Spine (Phila Pa 1976) 25:2285–2293
Olsewski JM, Simmons EH, Kallen FC, Mendel FC, Severin CM, Berens DL (1990) Morphometry of the lumbar spine: anatomical perspectives related to transpedicular fixation. J Bone Joint Surg Am 72:541–549
Ranade A, Samdani AF, Williams R, Barne K, McGirt MJ, Ramos G, Betz RR (2009) Feasibility and accuracy of pedicle screws in children younger than eight years of age. Spine (Phila Pa 1976) 34:2907–2911
Robertson PA, Stewart NR (2000) The radiologic anatomy of the lumbar and lumbosacral pedicles. Spine (Phila Pa 1976) 25:709–715
Rose PS, Lenke LG, Bridwell KH, Mulconrey DS, Cronen GA, Buchowski JM, Schwend RM, Sides BA (2009) Pedicle screw instrumentation for adult idiopathic scoliosis: an improvement over hook/hybrid fixation. Spine (Phila Pa 1976) 34:852–857, discussion 858
Ruf M, Harms J (2002) Pedicle screws in 1- and 2-year-old children: technique, complications, and effect on further growth. Spine (Phila Pa 1976) 27:E460–E466
Senaran H, Yazici M, Karcaaltincaba M, Alanay A, Acaroglu RE, Aksoy MC, Ariyurek M, Surat A (2002) Lumbar pedicle morphology in the immature spine: a three-dimensional study using spiral computed tomography. Spine (Phila Pa 1976) 27:2472–2476
Sokolic J, Sosa T, Ugljen R, Biocina B, Simunic S, Slobodnjak Z (1991) Extrinsic erosion of the descending aorta by a vertebral fixator. Tex Heart Inst J 18:136–139
Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB (1995) Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 20:1399–1405
Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, Cotler JM (1995) Placement of pedicle screws in the thoracic spine. Part I: morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am 77:1193–1199
Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, An HS (1995) Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Joint Surg Am 77:1200–1206
Viswanathan A, Relyea K, Whitehead WE, Curry DJ, Luerssen TG, Jea A (2008) Pneumothorax complicating “in-out-in” thoracic pedicle screw placement for kyphotic deformity correction in a child. J Neurosurg Pediatr 2:379–384
Wegener B, Birkenmaier C, Fottner A, Jansson V, Durr HR (2008) Delayed perforation of the aorta by a thoracic pedicle screw. Eur Spine J 17(Suppl 2):S351–S354
Yilmaz G, Demirkiran G, Ozkan C, Daglioglu K, Pekmezci M, Alanay A, Yazici M (2009) The effect of dilation of immature pedicles on pullout strength of the screws: Part 2: in vivo study. Spine (Phila Pa 1976) 34:2378–2383
Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, Thomas JC, Rothman SL, Fields BT (1987) Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976) 12:160–166
Zindrick MR, Knight GW, Sartori MJ, Carnevale TJ, Patwardhan AG, Lorenz MA (2000) Pedicle morphology of the immature thoracolumbar spine. Spine (Phila Pa 1976) 25:2726–2735
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shaikh, K.A., Bennett, G.M., White, I.K. et al. Computed-tomography-based anatomical study to assess feasibility of pedicle screw placement in the lumbar and lower thoracic pediatric spine. Childs Nerv Syst 28, 1743–1754 (2012). https://doi.org/10.1007/s00381-012-1783-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1783-z