Abstract
Objective
The aim of this prospective study was to analyze the changes in cerebrospinal fluid (CSF) distribution after endoscopic third ventriculocisternostomy (ETV).
Methods
Twenty-two hydrocephalic children (eight boys, aged 3 months to 17 years) candidates for ETV were studied by preoperative brain magnetic resonance (MR) and repeated post-ETV MRs at established time intervals. A volumetric analysis of CSF distribution after ETV was performed using a specific software.
Results
Fifteen children had an uneventful follow-up, whereas four required a second ETV due to a secondary closure of the stoma, one died of acute intracranial hypertension, and two needed an extrathecal shunt. A progressive reduction in the volume of the ventricles was found in case of successful ETV during the follow-up period. The ventricular volumes were reduced in average of 76 % of the initial volume at day 3, 69 % at 2 weeks, 42 % at 2 months, and 40 % at 6 months. This finding was associated with an enlargement of subarachnoid spaces which increased in case of successful ETV (192 % of initial volume at day 3; 210 % at day 15; 428 % at 2 months; and 468 % at 6 months). In case of secondary closure of the stoma, the distribution of intra- and extraventricular CSF tended to go back to the preoperative status.
Conclusion
Volume variations of the ventricles and the subarachnoid spaces are a good indicator of the efficacy of the ETV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endoscopic third ventriculostomy (ETV) is nowadays the first choice procedure in pediatric hydrocephalus whenever an obstacle is identified at the level of the posterior fossa on magnetic resonance (MR) imaging. ETV is preferred to extrathecal shunt because it is supposed to restore a pseudo-physiological cerebrospinal fluid (CSF) circulation [1, 2]. However, compared to extrathecal shunts, the variations in the ventricular volumes are more subtle after ETV and might be difficult to evidentiate on 2D MR images.
ETV has a high success rate which remains relatively stable over time. The success rates at 1 year and 2 years are 80 and 75 %, respectively [3]. A late failure can, however, occur despite an initial success due to a secondary closure of the stoma [4–6]. The clinical symptomatology may recur either acutely or progressively. In the last case, neither clinical evidence nor radiological changes in ventricular volumes on 2D planes might be recognizable in an early phase. Cases of sudden death in apparently healthy children after a successful ETV have also been reported in the literature [7].
Radiological criteria to follow on operated children are thus of paramount importance. Unfortunately, criteria for predicting that an apparently successful ETV will remain effective in the long run are lacking. The aim of this study was to analyze prospectively the changes in intracranial CSF on MR imaging after ETV and correlate them to the clinical response.
Patients and methods
Twenty-two children operated between January 2006 and April 2008 at the Paediatric Neurosurgical Department of Necker Enfants Malades Hospital, Paris, by an ETV for obstructive hydrocephalus with an intrinsic or extrinsic aqueductal stenosis were considered for this study. Exclusion criteria were: (a) hydrocephalus related to posterior fossa tumors because of the changes in CSF volumes related to the surgical treatment of the tumor and (b) children referred to our department with printed MR imaging studies done elsewhere without an available digital axial T2 weighted images (WI) study to assess the CSF volume. Children were studied by a preoperative brain MR and repeated postoperative MR at established time intervals (D1, D3, D15, D60 ± 3 days, and D180 ± 3 days).
MRI was performed with a 1.5-T (Signa General Electric®) scanner using the following sequences: 3D T1-weighted FSPGR sequence, axial FSE T2-weighted imaging (TR/TE, 6,000/120; 4-mm slices; 0.5-mm gap), and sagittal FSE T2 (TR/TE, 5,000/108; 3-mm slices; 0.3-mm gap) and if necessary coronal FLAIR sequences (TR/TETI, 10,000/150/2,250; 4-mm slices; 1-mm gap) and in more recent cases using a 3DT2-weighted imaging. Premedication (5 mg/kg of sodium pentobarbital, intrarectal) was used for uncooperative children.
Volumetric quantification of subarachnoid and ventricular CSF was performed on the axial T2 sequence using the “reformat” software from General Electric®. The operator—a well-experienced neuroradiologist—doing the measurement was blind for the clinical result of the ETV, though possibly aware of the success of the procedure of the grounds of the voiding signal on postoperative MRs.
On T2 sequences, the CSF appears much brighter than brain tissue. The operator enters threshold values to select exclusively CSF spaces, thus eliminating all other structures. Total CSF area (including ventricular and subarachnoid spaces) was calculated on a 3D image (volume rendering) by the software on one click. When necessary, other fluid-filled spaces like ocular globes and others were cut off with the same software. Whole intraventricular CSF volume was evaluated by eliminating the subarachnoid spaces in selecting the ventricles on a specific window of the software (“keep the object”).
The total CSF volume and the intraventricular volumes (lateral, third, and fourth) were thus measured and the extraventricular volumes could be calculated. The percentage between each measured volume at a given time and the initial volume were calculated (Vx / V°) to compensate for gender and age differences [8]. The preoperative volume was considered as a reference.
The differences between each measurement and the preoperative MR volumes were also calculated. The ratio of each difference to the preoperative volume was expressed as a percentage (Vx − V°) / V°. The statistical analysis was performed using SPSS(®) software.
Patency of the ventriculocisternostomy was evaluated on the presence or absence of a flow void phenomenon in the region of the floor of the third ventricle on the sagittal T2-weighted images (and on axial images also in doubtful cases, e.g., in case of large third ventricle).
Results
Population
Twenty-two children were included. Hydrocephalus was due to a malformative congenital aqueductal stenosis (12 cases), secondary to a stenosis of the aqueduct due to a tectal plate lesion (eight cases), and post-inflammatory changes secondary to intracranial hemorrhage (two cases).
Four children had already been operated on by an endoscopic third ventriculocisternostomy before the beginning of the study. However, in all of them, after an initial good response, the hydrocephalus had recurred and a redo ETV had been indicated. The children were included in this study at that point. The MR at the time of the clinical failure was considered as the “initial MR” for the study. The delay between the first ETV and the recurrence was more than 1 year in all the cases.
Clinical results: early and late failures
The ETV was successful in the immediate postoperative period in all but two children. These two cases were two newborns under 6 months of age that had a post-hemorrhagic hydrocephalus with progressive macrocrania. At MR, an aqueduct stenosis was found on sagittal T2WI. For this reason, an ETV was attempted. Despite a technically successful stoma, the head circumference continued to grow. A ventriculoperitoneal shunt was placed in both children 5 and 7 days after the ETV.
Among the remaining 20 cases, 15 had an uneventful follow-up period, whereas five presented a recurrence of the symptomatology:
-
Four of them required a redo ETV during the follow-up period due to a secondary closure of the stoma. Clinically, they all presented with signs of raised intracranial pressure. The closure was suspected on MR imaging (absence of flow void artefact phenomenon) and confirmed by a direct vision during a second endoscopy. In one child, among them, affected by a primary aqueduct stenosis, the closure occurred acutely within the first postoperative month. In this case, the early MR controls had documented a flow void signal through the third ventricular floor and a reduction in the volume of the ventricles. In the other three children who all had a tectal plate lesion, the recurrence occurred between 8 and 24 months after ETV. One child presented with acute hypertension, whereas in two, the symptoms and signs recurred progressively. All these cases responded to the redo ETV.
-
One child of the series died during the follow-up period. This girl developed an acute intracranial hypertension 8 months after a successful ETV at home becoming severely drowsy in a short time. When admitted to the hospital, she was comatous with bilateral mydriasis. An external drainage was established in emergency, but the child did not recover and died a few hours later.
MR and volumetric results
-
Successful ETV
-
Ventricles
A reduction of the volume of the ventricles was found in all the children after surgery. The ventricles in average reduced in size compared to the initial volumes (78 and 76 % of the initial volumes at D1 and D3, respectively; Fig. 1). However, the onset of this reduction could be slow. In three children after an initial decrease at D1, the ventricular volumes became slightly higher at D3, but then they started again to diminish. During the follow-up period, the reduction continued progressively after a successful ETV (69 % at D15, 42 % at D60, and 40 % at D180; Fig. 1). When comparing the evolution of the difference between the measured volume after ETV and the preoperative volume, the measurements were indexed on the initial volume, in order to decrease the bias which could derive from excessive differences in preoperative volumes (e.g., very large ventricles compared to large ones). At D3, the mean reduction so evaluated was of 19 %. At 2 weeks, it was about 28 %. At 2 months, it was about 40 %, and at D180, it was about 57 %.
-
Subarachnoid spaces
Conversely, in all patients with clinical successful ETV, the general trend was a gradual inflation of the subarachnoid spaces. However, this observation was certainly questionable at D1. In fact, besides the changes possibly induced by the surgical procedure in some children, the measurement of extraventricular spaces in the immediate postoperative MR of D1 could be flawed by the presence of subdural CSF effusions (four cases). The effusions were usually resolved already on the MR carried out at D3. At that time, the volume of subarachnoid volumes nearly doubled in the majority of the cases (mean increase of 192 %). The volume remained stable over time at 2 weeks (210 %) and increased further at 2 months (428 %) and at D180 (468 %) in successful cases (Fig. 2).
When comparing the differences of the ratio in postoperative subarachnoid spaces volumes referred to the initial volumes, there was again a more obvious increase at D1 than at D3 (178 % compared to 83 %) even in children without subdural effusion. Then, the volumes further increased in successful uncomplicated cases (185 % at 2 months; 325 % at 6 months).
-
-
Failures
In the two cases of unsuccessful ETV with an early failure on control MR, the ventricular volumes increased without significant changes in the subarachnoid spaces. After the shunt placement, they reduced in size as expected.
In the four children with a secondary closure of the stoma occurring during the follow-up period, seriated control MR showed a reduction in the volume of the subarachnoid spaces at MR. In these cases, despite an initial good response, with a mean increase in the volume of the compressed subarachnoid spaces of 148 % at D1, 203 % at D3, and a 217 % at D15, the extraventricular volumes returned almost to their initial values (mean 168 %) at the time of the failure (Fig. 3). In two of them, the reduction of subarachnoid spaces was concomitant with an enlargement of the ventricular volume and t3052248he recurrence of the clinical signs. In two children, the reduction of subarachnoid spaces was observed before the clinical signs (and before the enlargement of the ventricles in one of these two children). These changes were then reversed after the redo ETV.
Discussion
The fate of CSF after ETV
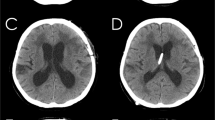
After a successful ETV, the volumes of ventricles decrease progressively [9–13]. The modifications in volumes are less spectacular than after CSF shunt placement (Fig. 5). The reduction in size of the ventricles varies from one case to the other. It may be limited, especially in chronic hydrocephalus; sometimes changes are so subtle that is difficult to perceive them on 2D images and they can only be assessed by detailed measurements [9] (Fig. 5). It is probably for such a reason that it has been stated that a reduction in volume is usually found in only a minority of operated on patients [1].
Our computerized analysis shows that changes in volumes are constant even if they might be delayed in some cases in the first postoperative days [14]. The proportion of patients showing the decrease in volume increases progressively in time with the volumetric reduction continuing in case of a successful procedure (19 % at D3 and 40 % at 2 months).
Kulkarni et al. demonstrated retrospectively that CSF over the cerebral hemispheres increased after ETV [11]. However, the pattern of such change was not analyzed.
In the present study, we prospectively assessed the modifications in CSF distribution after ETV. The analysis of the data obtained by an expert neuroradiologist using adapted software showed that the CSF in the subarachnoid spaces increases progressively after a successful ETV, whereas the volume of intraventricular CSF decreases progressively (Fig. 1). On the first postoperative day, the results may be flawed by the operation itself (amount of fluid replacement during the procedure as well as by some delay of the anatomofunctional structures responsible for CSF absorption within the subarachnoid spaces of the cerebral convexities in coping with the increased CSF flow) and in some cases by transient postoperative subdural effusions. However, already at the third day after surgery, the induced changes in volumes of subarachnoid spaces could be considered reliable as the successive trend appeared constantly towards a progressive increase in all successful cases. In fact, the MR studies carried out at 2 weeks postoperatively and at 2 months postoperative time interval showed a clear increase of the amount of CSF in the subarachnoid spaces.
During the first days following an ETV, it has been shown by previous studies that the ICP might remain elevated or even increased [2, 15]. These observations associated to our findings demonstrate that the first modifications following ETV consist in a redistribution of the CSF volumes that reduces the preexisting pressure gradient between the ventricular and extraventricular spaces. This redistribution of CSF explains why the overall ICP might remain elevated whereas it will decrease successively with the reduction of CSF total volumes. In our opinion, it is possible to propound a delay in the capability of the subarachnoid spaces to absorb the “new” flow of CSF in the first postoperative days.
Long term follow-up MR imaging showed also that the reduction in volume of the total CSF and ventricular volumes could continue to decrease even after several months. However, the proportion between intraventricular CSF and extraventricular CSF would remain almost constant (Fig. 1).
The correlation with clinical delayed failure and radiological criteria of success of ETV
During the follow-up, four children presented a clinical recurrence. In two children, at the moment of the acute clinical manifestations, the ventricular volumes were enlarged, the subarachnoid spaces were reduced, and the flow void signal through the third ventricle floor was absent on the MR examination. These findings were obviously highly suggestive of closure of the stoma which was confirmed by direct vision at surgery during the redo ETV. However, the analysis of the last control MR study before the acute episode as well as the MR of the children with an ETV failure showed that the subarachnoid spaces were reduced already before the clinical manifestations (Fig. 4) despite unchanged ventricular volumes and the presence of an uncertain flow void signal.
These data suggest that the modifications in subarachnoid spaces might be an early sign of a late closure of the stoma. Interestingly, these late failures were more common in the subgroup of children presenting a tectal plate lesion, without any apparent change in the tectal lesion itself. More in general, the prospective study we performed indicates that children with tectal lesions appear to be more prone to a late closure of the ETV stoma than children with congenital aqueductal stenosis. In summary, on the grounds of this experience, though limited by the still low number of cases, the three main criteria on postoperative MR T2-weighted images which may help in analyzing the success of an ETV are: (1) a reduction in volume of cerebral ventricular volume; (2) the presence of a flow void signal on sagittal images; and (3) an increase in volume of subarachnoid spaces (Fig. 5).
Limitations of the method
Despite the promising usefulness of such method, there are still important limitations that have to be stressed for the wide application in the clinical practice. The threshold to select the CSF intensity has to be determined manually to analyze different MRI of the same patient; the same threshold has to be selected in order to have comparable measurements. The evaluation needs an experienced neuroradiologist to measure the changes in CSF volumes and to compare them in the seriated studies performed with comparable technical standards. For this reason, in our series, the volumes were calculated on MR studies performed in the same institution and by the same radiologist blinded for the clinical status of the patients.
Conclusions
In conclusion, in all successful cases, a reduction of the total amount of CSF was found following ETV. Whilst the subarachnoid spaces were enlarged, the ventricular volume decreased progressively.
In the case of secondary closure of the stoma, the distribution of intra- and extraventricular CSF tended to go back to the preoperative status. Consequently, from a radiological standpoint, three elements should be verified on postoperative MR T2 images: (a) the presence of a flow void signal on sagittal images; (b) the reduction in volume of ventricular volume; and (c) the increase in volume of subarachnoid spaces.
References
Goumnerova LC, Frim DM (1997) Treatment of hydrocephalus with third ventriculocisternostomy: outcome and CSF flow patterns. Pediatr Neurosurg 27(3):149–152
Nishiyama K, Mori H, Tanaka R (2003) Changes in cerebrospinal fluid hydrodynamics following endoscopic third ventriculostomy for shunt-dependent noncommunicating hydrocephalus. J Neurosurg 98(5):1027–1031
Feng H, Huang G, Liao X, Fu K, Tan H, Pu H, Cheng Y, Liu W, Zhao D (2004) Endoscopic third ventriculostomy in the management of obstructive hydrocephalus: an outcome analysis. J Neurosurg 100(4):626–633
Erşahin Y, Arslan D (2008) Complications of endoscopic third ventriculostomy. Childs Nerv Syst 24(8):943–948
Kadrian D, van Gelder J, Florida D, Jones R, Vonau M, Teo C, Stening W, Kwok B (2005) Long-term reliability of endoscopic third ventriculostomy. Neurosurgery 56(6):1271–1278
Navarro R, Gil-Parra R, Reitman AJ, Olavarria G, Grant JA, Tomita T (2006) Endoscopic third ventriculostomy in children: early and late complications and their avoidance. Childs Nerv Syst 22(5):506–513
Drake JM (2007) Canadian Pediatric Neurosurgery Study Group. Endoscopic third ventriculostomy in pediatric patients: the Canadian experience. Neurosurgery 60(5):881–886
Xenos C, Sgouros S, Natarajan K (2002) Ventricular volume change in childhood. J Neurosurg 97(3):584–590
Bargalló N, Olondo L, Garcia AI, Capurro S, Caral L, Rumia J (2005) Functional analysis of third ventriculostomy patency by quantification of CSF stroke volume by using cine phase-contrast MR imaging. AJNR Am J Neuroradiol 26(10):2514–2521
Buxton N, Turner B, Ramli N, Vloeberghs M (2002) Changes in third ventricular size with neuroendoscopic third ventriculostomy: a blinded study. J Neurol Neurosurg Psychiatry 72(3):385–387
Kulkarni AV, Drake JM, Armstrong DC, Dirks PB (2000) Imaging correlates of successful endoscopic third ventriculostomy. J Neurosurg 92:915–919
Schwartz TH, Ho B, Prestigiacomo CJ, Bruce JN, Feldstein NA, Goodman RR (1999) Ventricular volume following third ventriculostomy. J Neurosurg 91(1):20–25
St George E, Natarajan K, Sgouros S (2004) Changes in ventricular volume in hydrocephalic children following successful endoscopic third ventriculostomy. Childs Nerv Syst 20(11–12):834–838
Preul C, Tittgemeyer M, Lindner D, Trantakis C, Meixensberger J (2004) Quantitative assessment of parenchymal and ventricular readjustment to intracranial pressure relief. AJNR Am J Neuroradiol 25(3):377–381
Cinalli G, Sainte-Rose C, Chumas P, Zerah M, Brunelle F, Lot G, Pierre-Kahn A, Renier D (1999) Failure of third ventriculostomy in the treatment of aqueductal stenosis in children. J Neurosurg 90(3):448–454
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Di Rocco, F., Grevent, D., Drake, J.M. et al. Changes in intracranial CSF distribution after ETV. Childs Nerv Syst 28, 997–1002 (2012). https://doi.org/10.1007/s00381-012-1752-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1752-6