Abstract
Introduction
Arteriovenous malformations are not a common disease in childhood. A national survey was conducted to reveal the Danish incidence of the disease, presentation, choice of treatment, and outcome.
Materials and methods
Forty patients were admitted to any of the five neurosurgical centers during the years 2000–2008. A retrospective survey was conducted using hospital records.
Results
Twenty-three males and 17 females presented with AVM with a mean age of 11.3 (1 month–18 years). The incidence was found to be 0.4/100,000. Early fatal outcome was seen in three patients. Treatment was surgery (12), endovascular (5), radiosurgery (6), or a combination of the above (10). Four patients were treated conservatively. Complications of the treatment were seen in 27%. Occlusion rate was 74%. Good or excellent outcome was seen in 65%.
Conclusion
A national survey may give a lower rate of success than in the specialized centers accepting patients more eligible for treatment. Still, the low number of children could call for centralization and collaboration in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arteriovenous malformation (AVM) in the brain is not a common disease in the pediatric population. This frequently complex brain disease often poses a challenge for its management, so that in spite of relatively few patients, it takes a rather large proportion of resources.
Most reports on pediatric AVMs deal with disease- and treatment-specific outcome. Only a few publications measure or calculate the incidence. Any type of stroke in the pediatric age group is rare (approximately 3/100,000). Hemorrhage accounts for half of the cases in pediatric cerebrovascular disease, and almost half of these are caused by AVM rupture [5]. The incidence of ruptured AVM in children inferred from the literature is thus approximately 0.7/100,000.
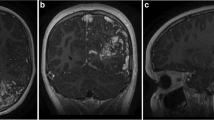
Initial symptoms range from cerebral catastrophe to vague neurological symptoms (Fig. 1). Severe symptoms caused by hematoma mass effect demand immediate action with surgical evacuation of the hematoma, often with the need to treat the AVM itself later, whereas a presentation without primary bleeding allows time for a more elaborate treatment plan.
Treatment of the AVM is performed to abolish further risk of bleeding and in some cases to treat epilepsy caused by the AVM. There are three modalities available for treatment. Surgery with complete excision of the AVM abolishes further bleeding risk and is regarded as the treatment of choice by most neurosurgeons if the surgical risk is considered acceptably low.
Surgical excision of an AVM is planned using digital subtraction angiography (DSA) with craniotomy and excision of the nidus as well as cutting feeders. Deeply located lesions or those located in eloquent areas pose the risk of damage causing neurological deficits.
Stereotactic radiation (radiosurgery) and embolization are both alternatives to surgery. The role of endovascular embolization as a first choice of treatment is debated. It is, by many neurosurgeons, considered a complimentary treatment type used to diminish the size of the AVM, especially prior to radiation. It is debated how often embolization alone is able to provide complete occlusion of a cerebral AVM [13].
Radiosurgery allows treatment in eloquent or deep areas with fewer complications than surgery. Radiosurgery for AVM is well tolerated in children [9]. Because of the delay from radiation treatment until AVM occlusion, stereotactic radiation is considered first treatment priority only in AVMs that are not surgically accessible. Radiation thus abolishes the bleeding risk in approximately 80% of patients [11] within 2 years in a mixed population of adults and children. Multimodality treatment combining two or three treatment modalities provides a broader range of possibilities for definite treatment of children with cerebral AVMs [3].
In the Danish population, the low incidence of new cases does not allow sufficient patients for all institutions to provide all three modalities. Adults of course add to the overall number but still specializations are seen. Surgical treatment was possible in all hospitals, but stereotactic radiation for pediatric brain AVMs was an option in only one institution, whereas another institution offered embolization during the study period. Consequently, there was a national collaboration and referral of patients. To give an overview of the whole Danish population, all five institutions were asked and gave consent to participate in this survey. The purpose of this paper is thus to give an overview of the treatment for AVM in the pediatric population in Denmark, the clinical presentation patterns, treatment modalities, and the overall success of treatment when administering single modality versus multimodality treatments.
Patients and methods
This retrospective study consecutively includes all patients with a cerebral AVM below 18 years of age admitted to any of the five Danish neurosurgical departments from 1 January 2000 to 31 December 2008. All neurosurgical departments completed the same survey. The survey used hospital records for clinical information on the patient, treatment, and outcome. The outcome was measured as excellent (AVM occlusion without new deficits), good (occlusion with minimal or mild new deficits), fair (occlusion with moderate new deficits), or non-occluded [4]. We required a minimum of 2 years follow-up for patients treated with stereotactic radiation
AVM data were measured and evaluated using imaging studies. All AVMs were diagnosed by DSA and stratified according to the Spetzler–Martin grading system based on the size of nidus, eloquence, and venous drainage [12].
The patients were included if the majority of questions were answered. Two patients were excluded as there were neither records nor imaging available. Information on the number of inhabitants was obtained from Statistics Denmark (Danmarks Statistik). We used descriptive statistics for demographical data. For comparison between groups, we calculated in percentages.
Patient characteristics
From 2000 to 2008, a total of 40 patients (23 male, 17 female) presented with a cerebral AVM (Table 1) with a mean age of 11.3 (range, 1 month–18 years). A total of 28 patients presented with a cerebral hemorrhage (Fig. 1). Epilepsy was another important and frequent presentation leading to diagnosis of the AVM. In eight patients, information on the symptoms leading to diagnosis was not available.
Three patients died: two were admitted with a Glasgow Coma Scale (GCS) of 3 and had immediate evacuation of the hematoma but failed to respond to treatment and died within a few days after hemorrhage. The third, a 1-year-old baby was admitted with a GCS of 3 and dilated pupils and died the same day due to another hemorrhage. All three patients were excluded from further evaluation.
Ethics
This work was a retrospective study using hospital records not having an impact on the patient or family.
Results
The number of Danish inhabitants is approximately 5.5 million. Approximately 1.2 million are children below 18 (Danmarks Statistik). The calculated incidence is the total number of AVMs/number of years in study period/number of children in the population (40/9/1.2 million) which amounted to approximately 0.4 per 100,000/year.
A total of 37 patients were evaluated for the treatment of the AVM (Fig. 2). Four of the patients were treated conservatively, one with a Spetzler grade 3 AVM and three with Spetzler grade 5 AVMs. The majority of the high-grade AVMs could not be offered any treatment although all three modalities were evaluated for applicability. At the other extreme, the majority of low-grade AVMs (1 and 2) were treated with surgery (nine patients). Approximately 25% of the patients (ten) were offered multiple treatments. In the multiple treatment group, the most common combination was embolization followed by either surgery (three) or stereotactic radio surgery (SR) (four) and, in some cases, both. SR was used in seven cases. Of the ten cases with multiple treatments, the AVM was occluded in only seven, reflecting the complexity in treating this group.
Table 2 shows the occlusion rate related to the primary treatment modality. In 10 out of 12 cases, surgery succeeded to completely abolish the AVM, whereas this was only the case for two out of five with embolization and for four out of six with SR.
The choice of treatment depends on the size and complexity of the AVM. Table 4 shows the success of treatment with respect to Spetzler grade. Occlusion of the AVM was successful in all Spetzler 1 cases, whereas none with Spetzler 5 were successfully treated, although an attempt was made in two patients. With a Spetzler grade 2, 3, or 4, occlusion was successful in two thirds.
The treatment profiles also varied between the centers (Table 3). At one institution (center 2), embolization was performed as the primary treatment in more than half of the patients (five of nine). At another institution (center 1), surgical excision of the AVM was the primary treatment in two thirds (9/15) and radiosurgery in one fourth (4/15). The third of the larger centers (center 3) did not seem to have any specific preference for any treatment.
The overall occlusion rate was 23 of 37 (62%). Excluding Spetzler grade 5 and patients treated conservatively gives a more optimistic picture with an occlusion rate of 23 of 31 (74%) (Table 4). Still, 8 of the remaining 31 patients were not offered further treatment ruling out the risk of a hemorrhage. Two of these eight patients had complications to the treatment with new neurological symptoms after only one attempt to embolize and further attempts to treat were abolished. Another three patients were only offered one type of treatment, and though there were no new symptoms, further treatments were not offered. One patient is waiting for yet another attempt to be treated.
Complications to the treatment itself were seen in 9 out of 33 patients treated with one or more of the three treatment options (Table 5). In three patients, the symptoms were transient. Complications were seen with each treatment modality, but by percentages of the total number of those patients treated, those treated with surgery had the lowest complication rate. Patients treated with embolization alone had the highest. The complication experienced by the individual patient differed in severity. In the surgical group, one patient ended up with permanent hemiparesis, whereas the other patient experienced worsening of preoperative hemiparesis lasting for months. In the embolized group, one patient had transient complications with severe nausea and two had lasting symptoms. One patient had a moderate handicap due to a brainstem lesion and the other patient did not have an occlusion of the AVM and experienced new symptoms with hemiparesis in one arm. In the group of patients treated with stereotactic radiation, one patient experienced cognitive problems 2 years after treatment and ongoing, whereas the other had immediate problems with a hemiparesis and visual field defects. The two last patients in the multiple treatment group were left with lasting epilepsy in one patient and transient aphasia in the other patient.
The outcome is defined by complications as well as the ability to occlude the AVM [10]. The outcome was excellent in 17 patients (Fig. 3), and three patients had the AVM occluded with only a minor defect. The two patients where the occlusion of the AVM was documented preoperatively were included in these numbers. Three patients had a fair outcome. Of the 14 patients with still patent AVMs, two patients had new symptoms. Therefore, good or excellent outcome was seen in 20 of 31 patients (65%).
Discussion
Epidemiology
In our study, we found the incidence of symptomatic AVM in children to be 0.4/100,000, compared to the incidence of 0.7/100,000 estimated from previous publications [5]. In order to obtain the true incidence, it would be necessary to include not only children admitted with a definite diagnosis of AVM but also those with a postmortem diagnosis of AVM. Although a congenital condition, we do not consider AVMs with presenting symptoms >18 years of age to be included in the group, and thus, clinically “silent” AVMs are excluded. As our study included only children surviving to receive treatment, we thus expect our calculated incidence to be lower than reported in the literature. It is, however, unlikely that any child in Denmark presenting with severe cerebral symptoms would not reach a neurosurgical center, and we thus believe that our estimates closely resemble to the actual rate of incidence.
The majority of pediatric cases with AVM bleed are >7 years. Most publications report a male preponderance [1, 5, 8], which is consistent with our findings (23/40 boys). Analyzing the mortality from childhood stroke in England and Wales over several decades, it was found that hemorrhage accounted for 71% of the deaths. The incidence averaged 7.5/million person years across all age groups, but it clearly peaked in late adolescence. The risk for lethal stroke was higher in boys than in girls [7]. The main observations in publications on clinical presentation and outcome are thus supported by data from mortality registers. In our material, there was an incidence of mortality with 3 out of 40 demonstrating that hemorrhage from AVMs can be severe.
Treatment and complications
Treatment with all three modalities including stereotactic radiation is only available in one of five centers. Geographical differences could thus be expected in the choice of treatment, which is shown in Table 3. In accordance with other reports, we thus observe that preference and local expertise exert considerable influence on the selection of treatment modality [2].
We found a relatively high average rate of complications (27%) compared to published data [6, 11]. Comparing the risk for complications between the treatment modalities, we found the highest rate of complications following embolization (Table 5). If the choice of treatment should be taken with respect to complication rate, one may argue that surgery should be the choice and local preponderance of treatment should be reevaluated. The size of our material does not permit stratification of complication rates with respect to Spetzler–Martin grade, hemorrhage, and general clinical presentation. We are, however, aware of the importance of these parameters, particularly the risks related to Spetzler–Martin grades 3 to 4 [6, 12].
Our rate of complication is high when compared to the adult population. Ledezma et al. [6] found a 9% complication rate with embolization. They, however, only reported clinically significant complications. In comparison, we report all occurrences, which could be defined as complications. If the four transient complications are omitted from our data, the overall risk is 15%, which is comparable to other reports. In a previous work, we found a rate of complication of 4% with stereotactic radiation in adults [11].
By using treatment combining two or three modalities when necessary, we obtain an average occlusion rate between 62% and 74%. Patients with a Spetzler–Martin grade 5 or otherwise untreatable AVMs negatively influence the average success rate. Dorfer et al. [3] report an occlusion rate of 93.3%. Part of the explanation for the discrepancy could be that we report all pediatric cases with AVMs, whereas most series report only treated cases and exclude untreatable AVMs.
Based on this, it could be inferred that children with non-occluded AVMs and no complications from the primary first treatment should be offered another attempt to abolish the bleeding risk, even if it would increase the risk of treatment complications—and that this decision should rest on and be balanced against the cumulative bleeding risk of a patent AVM. This reasoning is particularly relevant in children because of the long life expectancy. The reason for not offering this may depend on local as well as individual factors.
Conclusion
In Denmark, the calculated incidence of symptomatic AVM in children is 0.4 per 100,000 given total the average annual occurrence of 4.4 children per year. The children in the present study were treated at five different institutions. Excluding untreatable cases, we found an occlusion rate of 74% leaving a risk of permanent complications of 15%. The chance of a good or excellent outcome was 65%. We also found significant regional differences in the treatment pattern.
A national survey may give a lower rate of success than in the specialized centers accepting patients more eligible for treatment. Still, the low number of children could call for centralization and collaboration in this population.
References
Al-Jarallah A, Al-Rifai MT, Riela AR, Roach ES (2000) Nontraumatic brain hemorrhage in children: etiology and presentation. J Child Neurol 15(5):284–289
van Beijnum J et al (2008) Patterns of brain arteriovenous malformation treatment: prospective, population-based study. Stroke 39(12):3216–3221
Dorfer C, Czech T, Bavinzski G, Kitz K, Mert A, Knosp E, Gruber A (2010) Multimodality treatment of AVMs in children: a single-center 20 years experience. Childs Nerv Syst 26(5):681–687
Flickinger JC et al (2000) Development of a model to predict permanent symptomatic postradiosurgery injury for arteriovenous malformation patients. Arteriovenous Malformation Radiosurgery Study Group. Int J Radiat Biol Phys 46(5):1143–1148
Kumar RM, Shukla D, Mahapatra AK (2009) Spontaneous intracranial hemorrhage in children. Pediatr Neurosurg 45:37–45
Ledezma CJ, Hoh BL, Carter BS, Pryor JC, Putman CM, Ogilvy CS (2006) Complications of cerebral arteriovenous malformation embolization: multivariate analysis of predictive factors. Neurosurgery 58(4):602–611
Mallick AA, Ganesan V, O’Callaghan FJ (2010) Mortality from childhood stroke in England and Wales 1921–2000. Arch Dis Child 95(1):12–19
Meyer-Heim AD, Boltshauser E (2003) Spontaneous intracranial haemorrhage in children: aetiology, presentation and outcome. Brain Dev 25(6):416–421
Mirza B et al (2010) Stereotactic radiotherapy and radiosurgery in pediatric patients: analysis of indications and outcome. Childs Nerv Syst 26:1785–1793
Pollock B, Flickinger J (2002) A proposed radiosurgery-based grading system for arteriovenous malformations. J Neurosurg 96:79–85
Skjoeth-Rasmussen J, Roed H, Ohlhues L, Jespersen B, Juhler M (2010) Complications following linear accelerator based stereotactic radiation for cerebral arteriovenous malformations. Int J Radiat Oncol Biol Phys 77(2):542–547
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg 65:476–483
Weber W et al (2007) Preoperative embolization of intracranial arteriovenous malformations with onyx. J Neurosurg 61(2):244–252
Acknowledgments
We thank Deborah Anne Schut, Medical Dosimetrist, for valuable contribution in the writing process and Margret Jensdottir, Neurosurgeon, who contributed with collection of data.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skjøth-Rasmussen, J., Obbekjær, T., Birkeland, P. et al. Multimodality treatment approach in children with cerebral arteriovenous malformation—a survey in the Danish population. Childs Nerv Syst 28, 587–592 (2012). https://doi.org/10.1007/s00381-011-1640-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-011-1640-5