Abstract
Background
Choroid plexus tumors (CPT) are rare pediatric tumors. A population-based study on choroid plexus carcinoma (CPC) and choroid plexus papilloma (CPP) was carried out to describe the incidence, demographic, and outcome data and to identify potential prognostic factors.
Methods
The CPT population from the Canadian databank of CNS tumor in children ≤36 months diagnosed between 1990 and 2005 was reviewed
Results
Out of the 579 reported cases of CNS tumors, 37 were CPT. The annual age-adjusted incidence rate was 0.22 + 0.12 (95% CI 0.16–0.28)/100,000 children <3 years. There were 21 (56.7%) CPP and 16 (43.3.5%) CPC. Twenty patients (54%) were males. Median age at diagnosis was 7 months(range 0–30). Ten patients(62.5%) with CPC and one with CPP were metastatic at diagnosis. Twenty patients with CPP (95%) had a complete resection, whereas 6/16 CPC (37.5%) achieved a resection >90%. Fourteen CPC patients received adjuvant chemotherapy. None of the 37 patients received adjuvant radiation. At completion of survey, all CPP and five CPC were alive. Median survival time for CPC patients was 15 months (0–120). One death was related to intraoperative hemorrhage, another to chemotherapy-induced toxicity, and one to secondary AML. Age at diagnosis, degree of resection and metastatic status were not significant prognostic factors for CPC.
Conclusion
By contrast to CPC, CPP have an excellent prognosis following surgery alone. Survival of CPC remains poor. However, these data may suggest adjuvant chemotherapy can alter the aggressive natural history of CPC. As with other rare CNS tumors, international collaboration is required to identify optimal therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Choroid plexus tumors (CPT) are rare intraventricular tumors occurring mainly in very young children. With an annual incidence of 0.3 cases per million, these tumors account for 2% to 4% of all childhood brain tumor [1, 2]
Given the rarity of such tumors most of the available information comes from case reports and small series from single institution. Although efforts to analyze these tumors through the compiled cases from the literature have provided interesting information, meta-analyses may not reflect the clinical reality of such a rare group of patients [3]. The main objective of this study was to collect all cases of CPT in Canada to provide a population-based series, and examine treatment practices in this rare entity. Our secondary objective was to further identify potential prognostic factors and analyze the role of adjuvant therapies.
Method
The current study is a subgroup analysis of a larger national collaborative study on brain tumors in children less than 36 months diagnosed with a CNS tumor between 1990 and 2005, conducted in the Canadian Pediatric Brain Tumor Consortium (CPBTC) [4].
The CPBTC is a network of 17 Canadian pediatric institutions that collaborate and develop research in pediatric neurooncology. A standardized questionnaire was sent out to all participating centers to establish a Canadian infant brain tumor database. The questionnaire requested information about age at time of presentation, duration of symptoms at time of presentation, location of tumor, degree of resection, pathological diagnosis, treatment after surgery, time to event, treatment after event, and time to death. The REB of each participating institution approved the study. The subgroup analysis of patients diagnosed with CPT represents the subject of the current report.
A mean age-adjusted incidence rate per 100,000 children years was calculated using the Statistics Canada population database for the year 2000 [5]. Extent of resection was defined by postoperative imaging and reported as followed: gross total resection (GTR) for nonvisible tumor, near complete resection for resection between 90% and 95%, biopsy for resection less than 10% and partial resection in all other remaining situations.
Statistical analysis was performed using SPSP16. For descriptive statistics, continuous data was compared using Student t test. Noncontinuous data was compared using Chi-square. Estimation of event free survival and overall survival was performed using the Kaplan–Meier analysis. Overall survival was calculated from the date of diagnosis to the date of last follow-up or date of death from any cause. Event-free survival was calculated from the date of initial diagnosis to the date of earliest radiologic disease progression. Level of significance was p = 0.05.
Results
Sixteen of the 17 Canadian centers participated to the study. Of the 579 patients in the database, 37 (6.4%) were diagnosed with a choroid plexus tumor. The mean age-adjusted incidence was 0.22 + 0.12 (95% CI 0.16–0.28) per 100,000 children <3 years of age per year.
The number of news cases of CPT was higher during the initial 5 year period, and then stable over the last 10 years: 43.3% of the cases were diagnosed between 1990 and 1995, 27% between 1996 and 2000, and 29.7% between 2001 and 2005.
Twenty-one (56.7%) patients had a choroid plexus papilloma (CPP) of which one was reported atypical choroid plexus papilloma. Sixteen (43.3%) patients had choroid plexus carcinoma (CPC). Although central pathology review was not part of the current study, five of the CPC (37.5%) reported from one single institution (Hospital for Sick Children, Toronto) were retrospectively tested and stained positive for INI1, excluding the diagnosis of ATRT.
Among the 37 patients, there were 20 males and 17 females with a similar sex distribution in both tumors (Table 1).
Mean age at diagnosis in the CPP group was 7 months (range 0–28 months) and 10 months (range 1–30) for patients with CPC. Twenty-three patients (62%) were less than 12 months, 10 (27%) were aged between 12 and 23 months, and four (11%) were 24 months and older. The proportion of CPC in these age groups was, respectively, 34.7%, 40%, and 100%. CPT accounted for 11.9% of all CNS tumors diagnosed in children less than 12 months group, 4.9% in the group aged between 12 and 23 months, and 2.1% in the group 24 months and older.
The median duration of presenting symptoms prior to diagnosis was 1 week (range 0–10 weeks) for CPP and 3 weeks (range 0–28 weeks) for CPC. The vast majority of the presenting symptoms, in both subgroups, were related to increase intracranial pressure (nausea/vomiting, enlarged head circumference, and abnormal eyes movement). Thirty-three tumors (89.2%) were localized in the supratentorial compartment (Fig. 1). All four infratentorial tumors were CPC. Although information on CSF cytology was not available for 54% of the patients and staging imaging was unavailable in 30% of the cases, 10 (62.5%) patients with CPC were reported metastatic at diagnosis. Surgery was attempted in all patients. GTR was more frequently achieved in patients with CPP (95%) compared to patients with CPC (25%) (p < 0.0001). One patient with CPC died of intraoperative hemorrhage. In the CPC group, there was no significant survival benefit associated with the extent of resection. Mean survival time for the four patients with complete resection was 53.2 months (±25) compared to 37.1 months (±14; p = 0.81) for the 12 with incomplete resection.
Two patients with CPC did not receive postoperative active therapy. One of them died of intraoperative hemorrhage and the other one underwent palliative care.
The 14 remaining patients with CPC received adjuvant chemotherapy following several different so called “baby brain” protocols, the SIOP 2000 CPT protocol, or ICE chemotherapy regimen [6–8]. Information on the type of chemotherapy was missing for two patients. No patients underwent high-dose chemotherapy and stem cell support. No patient received adjuvant radiation.
Ten of the CPC patients progressed or relapsed at a median progression time of 10 months. Among them, five received further chemotherapy but eventually all died of disease progression and four patients were treated with a palliative intent at time of progression.
At completion of the survey, 26 patients were alive. All patients with CPP, including one reported metastatic at diagnosis and who did not receive any adjuvant therapy, were alive.
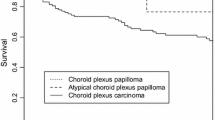
In the CPC group, five patients were alive at completion of survey, resulting in a median survival time of 15 months (range 0–120) with a projected 2 and 5 years OS of, respectively, 50% ± 12.5% and 31.3% ± 13.2% (Fig. 2). Death was related to disease progression in nine patients, to intraoperative hemorrhage in one, to chemotherapy toxicity in one, and to secondary AML in one patient.
Survivors’ age ranged from 17 to 180 months (median 70.5 months) when survey was completed. Data regarding school and academic performance were received on 18 of the 26 survivors. One of the three patients with CPC and five of the 15 with CPP were attending specialized school.
Discussion
Approaching a rare group of tumor like CPT through a population-based study highlights several aspects regarding tumor incidence and tumor management that are not reflected in small series or case reports. This for example concerns the annual incidence, the year-to-year variation in incidence, the rate of children undergoing palliation only, trends in therapeutic management in addition to contributing to better delineate prognostic factors in an unselected group of patients. Here, we analyzed the subgroup of CPT out of a large database of infants and young children diagnosed with CNS malignancies in Canada between 1990 and 2005. We found that 6.4% of all CNS tumors entered in the database were CPT. This is slightly higher than the 1–4% figure provided in the literature [2]. Our finding are likely due to our analysis that was limited to CNS tumors prior the age of 3 years as the vast majority of CPT are diagnosed before the age of 2 [9–11].
The incidence of CPT in the first 3 years of life has not been well described. From the review of 1,289 published cases of brain tumors in the first year of life, Larouche et al. estimated CPT to account for 11% of all CNS tumors. Tumors of the central nervous system in the first year of life [12]. We confirm this percentage with a higher incidence in the first year of life, decreasing by half for each subsequent 2 years. Our corresponding adjusted incidence for CPT in the Canadian population was 0.22 + 0.12 (95% CI 0.16–0.28) per 100,000 children <36 months years per year.
Our patients were diagnosed at a younger age (median 7 months) compared to previously reported studies. In the St Jude experience, the median age at diagnosis for the CPC group was 14.5 months. Mac Evoy et al. described a median age of 17 months for the CPP and 13 months for the CPC group and in the only one infant series of CPC, Duffner reported a median age at diagnosis of 17.5 months [13, 14]. The population-based approach of our study likely contributes to explain such demographic differences, as compared to patients referred to a supraregional center or patients registered in a clinical trial.
When comparing CPP and CPC groups, there were no significant differences in term of sex distribution, age at diagnosis, or tumor location. The vast majority of the tumors were located in the supratentorial compartment and no CPP were found below the tent of the cerebellum. Wolff et al. has described a shift of the age distribution from younger to older patients the more caudal the tumor was located [3]
Infants with CPP had a shorter duration of symptoms than those with CPC (respectively 2.1 weeks ± 0.6 and 5.5 weeks ± 2.03). Although the difference was not statistically significant (p = 0.063), Pencalet et al. described similar trend, without clear explanation since in his series for instance, hydrocephalus was present in 33/38 patients without distinction between benign and malignant histology [15].
Our study is of particular interest while describing the recent trend in management for these very young patients. Over the study period, the therapeutic approach has been fairly homogenous including attempt to maximal surgical resection for all CPT, adjuvant chemotherapy and notably avoidance of upfront radiation for the CPC group. In that setting, we could confirm that CPP are more often amenable to gross total resection than CPC. In the CPP group, the 5 years OS of 100% confirmed the excellent outcome after complete resection in absence of adjuvant therapy [14–16].
In CPC, the ability to achieve upfront complete resection is often hindered by their extreme vascular nature and the usual invasion to the adjacent brain, as illustrated by a rate of 27% of GTR and 40% of resection greater than 90% in our series. Despite the well-recognized prognostic value of the extent of resection in this tumor, our series failed to confirm the survival benefit associated with gross total resection [15, 17–20].
All 14 CPC patients who received postoperative treatment with intent to treat, received chemotherapy only. Whether adjuvant chemotherapy improves outcome in CPC remains controversial, especially in the setting of complete resection [21, 22]. But in our experience despite a majority of incomplete resection, and the absence of radiation, one third of CPC patients treated with various chemotherapy regimens, were alive at completion of survey, with a 5 years OS of 31.3% ± 13.2%. These results have to be interpreted in light of the absence of central pathology review to exclude ATRT associated with worst outcome than CPC. Although incomplete, at least in one third of the cases, ATRT diagnosis was ruled out. Our survival figure is in keeping with previously reported series using various combination of adjuvant therapies, in which OS ranges between 26% and 51% [3, 13, 15, 16, 23]. This may suggest that adjuvant chemotherapy can alter the natural aggressive course of this disease despite incomplete resection. In her review of published cases of CPT, Wrede et al. reported a 5-year OS of 46.4% (±6.1) for 104 CPC patients who received adjuvant chemotherapy compared to 27.6% (±4.8) for those who did not (p = 0.0004). This result was not significant anymore in subgroup analysis for patients who achieved a gross total resection [21]. Fitzpatrick also described survival benefit of adjuvant therapy (radiation in conjunction or not of chemotherapy) only in patients with incomplete resection [22].
While second look surgery is recommended to achieve gross total resection, the success of repeated surgery may remain limited by the significant risk of intraoperative bleeding. It has been shown that chemotherapy can effectively alter and reduce the vascularity of CPC and therefore facilitate gross total resection at the time of second look surgery [24].
The role of radiation in these tumors is even more a matter a debate given the very young age of the patients at diagnosis (median of 7 months in our series) [22, 25]. In this series, although postoperative chemotherapy was heterogeneous among CPC patient, no patient received adjuvant radiation. This is echoing the significant concern of the pediatric neurooncology community of severe neurocognitive damage associated with radiation in such young group of age. This is particularly relevant in CPT because of the usual large tumor size, the common supratentorial location and even more, because of the frequent chronic CSF hydraulic dysfunction associated with CPT, as well as the relative high incidence of surgical and infectious complications which contribute to neurocognitive and functional impairment even when radiation is omitted [8]. In fact, one third of the patients with CPP treated with surgery only and for whom neuro developmental information was available, did required special education.
Upcoming collaborative studies in CPC should further explore the role of adjuvant chemotherapy and carefully weigh the use of adjuvant radiation given the extreme neurotoxic susceptibility of this very young group of patients. As the incidence of these tumors is a major challenge for the development of cooperative protocols, national or better international CPT registries should be considered to improve our knowledge of this entity.
References
Jänisch W, Staneczek W (1989) Primary tumors of the choroid plexus. Frequency, localization and age. Zentralbl Allg Pathol 135:235–240
Greenberg ML (1999) Chemotherapy of choroid plexus carcinoma. Childs Nerv Syst 15:571–577
Wolff JE, Sajedi M, Brant R, Coppes MJ, Egeler RM (2002) Choroid plexus tumours. Br J Cancer 87:1086–1091
Keene D, Lafay-Cousin L, Carret AS, Crooks B, Eisenstat D, Fryer C, Johnston D, Larouche V, Mograbi A, Silva M, Wilson B, Zelcer S, Bouffet E (2008) The Canadian Pediatric Brain Tumor Consortium national survey of CNS tumors in children under 3 years of age. Neuro Oncol 10:416
Annual Demographic Statistics (2005) Statistics Canada Catalogue no. 91-213-XIB
Duffner PK, Horowitz ME, Krischer JP, Friedman HS, Burger PC, Cohen ME, Sanford RA, Mulhern RK, James HE, Freeman CR et al (1993) Postoperative chemotherapy and delayed radiation in children less than 3 years of age with malignant brain tumors. N Engl J Med 328:1725–1731
Wrede B, Hasselblatt M, Peters O, Thall PF, Kutluk T, Moghrabi A, Mahajan A, Rutkowski S, Diez B, Wang X, Pietsch T, Kortmann RD, Paulus W, Jeibmann A, Wolff JE (2009) Atypical choroid plexus papilloma: clinical experience in the CPT-SIOP-2000 study. J Neurooncol 95:383–392
Lafay-Cousin L, Mabbott DJ, Halliday W, Taylor MD, Tabori U, Kamaly-Asl ID, Kulkarni AV, Bartels U, Greenberg M, Bouffet E (2010) Use of ifosfamide, carboplatin, and etoposide chemotherapy in choroid plexus carcinoma. J Neurosurg Pediatr 5:615–621
Walker DA, Perilongo G, Punt JAG, Taylor RE (2004) Brain and spinal tumors of childhood, 1st edn. London E Arnold
Boyd MC, Steinbok P (1987) Choroid plexus tumors: problems in diagnosis and management. J Neurosurg 66:800–805
Allen J, Wisoff J, Helson L, Pearce J, Arenson E (1992) Choroid plexus carcinoma-responses to chemotherapy alone in newly diagnosed young children. J Neurooncol 12:69–74
Larouche V, Huang A, Bartels X, Bouffet E (2007) Pediatr Blood Cancer 49:1074–1082
Duffner PK, Kun LE, Burger PC, Horowitz ME, Cohen ME, Sanford RA, Krischer JP, Mulhern RK, James HE, Rekate HL, Friedmean H, the Pediatric Oncology Group et al (1995) Postoperative chemotherapy and delayed radiation in infants and very young children with choroid plexus carcinomas. Pediatr Neurosurg 22:189–196
McEvoy AW, Harding BN, Phipps KP, Ellison DW, Elsmore AJ, Thompson D, Harkness W, Hayward RD (2000) Management of choroid plexus tumours in children: 20 years experience at a single neurosurgical centre. Pediatr Neurosurg 32:192–199
Pencalet P, Sainte-Rose C, Lellouch-Tubiana A, Kalifa C, Brunelle F, Sgouros S, Meyer P, Cinalli G, Zerah M, Pierre-Kahn A, Renier D (1998) Papillomas and carcinomas of the choroid plexus in children. J Neurosurg 88:521–528
Strojan P, Popović M, Surlan K, Jereb B (2004) Choroid plexus tumors: a review of 28-year experience. Neoplasma 51:306–312
Ellenbogen RG, Winston KR, Kupsky WJ (1998) Tumors of the choroid plexus in children. Neurosurgery 42:470–475
Berger C, Thiesse P, Lellouch-Tubiana A, Kalifa C, Pierre-Kahn A, Bouffet E (1989) Choroid plexus carcinomas in childhood: clinical features and prognostic factors. Neurosurgery 25:327–335
Packer RJ, Perilongo G, Johnson D, Sutton LN, Vezina G, Zimmerman RA, Ryan J, Reaman G, Schut L (1992) Choroid plexus carcinoma of childhood. Cancer 69:580–585, Review
Wrede B, Liu P, Ater J, Wolff JE (2005) Second surgery and the prognosis of choroid plexus carcinoma—results of a meta-analysis of individual cases. Anticancer Res 25:4429–4433
Wrede B, Liu P, Wolff JE (2007) Chemotherapy improves the survival of patients with choroid plexus carcinoma: a meta-analysis of individual cases with choroid plexus tumors. J Neurooncol 85:345–351
Fitzpatrick LK, Aronson LJ, Cohen KJ (2002) Is there a requirement for adjuvant therapy for choroid plexus carcinoma that has been completely resected? J Neurooncol 57:123–126
Chow E, Reardon DA, Shah AB, Jenkins JJ, Langston J, Heideman RL, Sanford RA, Kun LE, Merchant TE (1999) Pediatric choroid plexus neoplasms. Int J Radiat Oncol Biol Phys 44:249–254
Kamaly-Asl ID, Bouffet E, Halliday W, Drake JM, Rutka JT, Dirks PB, Kulkarni AV, Taylor MD (2005) Neoadjuvant chemotherapy reduces operative haemorrhage and improves resection for choroid plexus carcinomas. Childs Nerv Syst 21:852
Mazloom A, Wolff JE, Paulino AC (2009) The impact of radiotherapy fields in the treatment of patients with choroid plexus carcinoma. Int J Radiat Oncol Biol Phys 75:S510
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lafay-Cousin, L., Keene, D., Carret, AS. et al. Choroid plexus tumors in children less than 36 months: the Canadian Pediatric Brain Tumor Consortium (CPBTC) experience. Childs Nerv Syst 27, 259–264 (2011). https://doi.org/10.1007/s00381-010-1269-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1269-9