Abstract
Purpose
Hemorrhage from an arteriovenous malformation (AVM) is the commonest cause of childhood stroke. Management options for children include observation and medical management, surgical resection, endovascular embolization, or stereotactic radiosurgery, alone or in combination.
Methods
Radiosurgery is used for high-risk malformations in critical brain locations. While this goal is being achieved, there should be limited morbidity and hopefully no mortality from hemorrhage or radiation-induced brain injury.
Results
Physicians who consider AVM radiosurgery cite one or more of the following: (1) that radiosurgery is an effective therapy required for the management of deep-brain AVMs; (2) that radiosurgery is an effective therapy for residual AVMs after subtotal resection; (3) that radiosurgery is worthwhile in an attempt to lower management risks for AVMs in functional brain locations; (4) since embolization does not cure most AVMs, additional therapy such as radiosurgery may be required; and (5) microsurgical resection may not be the best choice for some children.
Conclusion
Radiosurgery is the first and only biologic AVM therapy; it represents the beginnings of future cellular approaches to vascular malformation diseases. For this reason, the future of radiosurgery may be impacted positively by the development of other biologic strategies such as brain protection or endothelial sensitization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemorrhage from an arteriovenous malformation (AVM) is the commonest cause of childhood stroke. Management options for children include observation and medical management, surgical resection, endovascular embolization, or stereotactic radiosurgery, alone or in combination. Typically, radiosurgery is used for high-risk malformations in critical brain locations. Successful AVM radiosurgery is dependent upon achievement of the outcome of complete AVM nidus obliteration that leads to elimination of the future hemorrhage risk [1–3]. While this goal is being achieved, there should be limited morbidity and hopefully no mortality from hemorrhage or radiation-induced brain injury. Physicians who consider AVM radiosurgery cite one or more of the following: (1) that radiosurgery is an effective therapy required for the management of deep-brain AVMs; (2) that radiosurgery is an effective therapy for residual AVMs after subtotal resection; (3) that radiosurgery is worthwhile in an attempt to lower management risks for AVMs in functional brain locations; (4) since embolization does not cure most AVMs, additional therapy such as radiosurgery may be required; and (5) microsurgical resection may not be the best choice for some children. Since radiosurgery is the first and only biologic AVM therapy, it represents the beginnings of future cellular approaches to vascular malformation diseases. For this reason, the future of radiosurgery may be impacted positively by the development of other biologic strategies such as brain protection or endothelial sensitization. In this report, we reviewed our experience in the use of stereotactic radiosurgery for children with AVMs.
When to consider radiosurgery
The following criticisms have been leveled against the use of radiosurgery (1) that radiosurgery does not always work especially when only partial AVM obliteration is achieved [4]; (2) that brain hemorrhage may occur during the time it takes for radiosurgery to work; (3) that radiation-related morbidity may cause functional neurologic deficits; (4) that there may exist “long-term” problems after brain irradiation [5]; and (5) that resection may be a more cost-effective treatment over the long term [6]. Though all these points can be argued, most neurosurgeons agree that the role of radiosurgery is greatest for patients with small-volume, deep-brain AVMs [2, 7–9]. In children, irradiation of the developing brain is an important consideration. For that reason, radiosurgery is uncommon below the age of three. It has a lesser role for children with larger and surgically accessible AVMs. In between these two extremes, there exists much debate. The role of radiosurgery for patients with small and yet accessible AVMs is growing steadily [10]. For patients with large-volume yet deeply located AVMs, multi-modality management often is required. Thus, whether radiosurgery should be considered in the management of an individual patient depends upon the factors of AVM volume, brain location, prior hemorrhage history, patient age, and surgical resectability. These factors have been studied in detail by different groups towards predicting successful AVM outcomes or reasons for radiosurgery failure [3, 11–14].
The radiobiological effects
Radiosurgery is effective because the use of highly conformed and selective focused irradiation leads to endothelial cell and myofibroblast proliferation with the targeted AVM blood vessel [8, 15–17]. Stereotactic definition of the AVM target ensures that these radiobiologic effects are limited to the malformation. Conformal radiosurgery allows irradiation of only a small volume of surrounding normal tissue in the region of radiation dose fall-off [2, 18]. Dose-prescription formulae are used to help select an appropriate radiation dose depending on imaging and clinical factors [19, 20].
The immediate effect of radiosurgery is to damage the endothelial cells of the AVM vessels. Release of tissue-specific cytokines common to other forms of radiation-induced injury are likely to mediate such acute effects. Inflammatory cells mediate tissue repair in response to irradiation. Later, chronic inflammation consists of the ingrowth of granulation tissue that contains fibroblasts and new capillaries. These events may explain the delayed imaging changes sometimes observed after radiosurgery. Szeifert et al. identified the presence of actin-producing fibroblasts, so called myofibroblasts that are hypothesized to exert contractile properties and facilitate AVM obliteration [21]. It is common that contrast-enhanced MRI studies at this late stage after obliteration show enhancement of the obliterated AVM. This finding does not indicate a “patent” AVM, but we believe a marker for the newly formed capillary network within the scarred AVM tissue remnant. Several reports have noted the rare, late finding of cyst formation at the AVM site which probably represents expansion of the extracellular fluid space within the fibrosis [5, 22]. Radiosurgery may impact on seizure control through irradiation of epileptogenic tissue or through correction of abnormal hemodynamic conditions [23–25].
In younger children, it is important to remember that the AVM may still be in a developmental stage during initial clinical presentation. There are reports of “recurrent” AVMs after confirmed complete angiographic removal, only to have new AVM tissue form. This appears to occur in response to vascular endothelial growth factor. Such recurrence can also occur after AVM radiosurgery. Thus, delayed angiographic assessments can be important for children.
Results of stereotactic radiosurgery
Clinical experience
At the University of Pittsburgh, 1,129 AVM patients had gamma knife radiosurgery during a 20-year interval. One hundred thirty-nine pediatric AVM patients (≤18 years old) underwent a single session procedure. The median patient age was 12 years (range 2–18). Prior intracranial hemorrhage was reported in 66% of patients (n = 92), headaches in 11%, seizures in 14%, incidental in 4%, and neurological symptoms or signs without bleeding in 5%. In this pediatric AVM series, the rate of patients with a prior symptomatic hemorrhage was much higher than in our adult series (66% in pediatric vs. 42% in adult). The wide variety of different clinical presentations ensures discussion of the different treatment options in all patients. All referred vascular malformation cases are discussed at a weekly multidisciplinary conference. Intravascular embolization was performed in 22 patients (16%) before radiosurgery. Eighteen patients (13%) had already undergone one or more surgical procedures prior to radiosurgery. Four underwent craniotomy and hematoma removal, and six patients underwent ventricular shunt placement. The median AVM volume was 2.2 ml (range 0.1–18.3 ml). The 50% isodose was used as the margin isodose in 78% of patients. No patients were treated below the 50% isodose.
The Spetzler–Martin grading system was used to classify all AVMs according to size, critical location, and venous drainage. The most commonly referred patient was one with a small-volume, deeply located AVM (grade III, n = 60, 43%). The most infrequent patient had an AVM (n = 3, 2%) that was small, superficial, and non-critical in location (grade I). In such patients, we first recommend a resection. Nineteen percent of patients (n = 27) had a grade VI AVM. The AVM was located totally within the parenchyma of the brainstem or thalamus. The Spetzler–Martin grades II, IV, and V patients were 24% (n = 34), 11% (n = 15), and 0%, respectively. The median dose delivered to the AVM margin was 20 Gy (range, 15–25 Gy), and the median maximum dose was 34 Gy (range, 22.2–50 Gy). Although there is no such thing as an “inoperable” AVM, we consider an AVM to be associated with an acceptably high risk for resection when located completely within the parenchyma of the brainstem, thalamus, or basal ganglia. In our series, 12 patients had brainstem AVMs, 26 had thalamic AVMs, and 17 had basal ganglia malformations.
When radiosurgery did not lead to complete AVM obliteration, further discussion occurred over the merits of repeat radiosurgery or resection. Fifteen patients underwent repeat radiosurgery for a persistent AVM nidus, at least 3 years after a first procedure. If after 3 to 4 years, a residual AVM nidus with early venous drainage remains, then a second radiosurgical procedure should be performed [26]. We do not recommend additional management for patients who harbor only an early draining vein as this feature resolves over an additional observation interval [27]. In addition, we know of no patient who sustained a later hemorrhage when only an early draining vein was present. Some patients will have an angiogram that shows some abnormal-appearing vessels in the region of the irradiated AVM, without early venous drainage. This fine vascular blush may indicate the neocapillary network within the scarred malformation. Such findings also require no additional therapy.
In most series, repeat radiosurgery is associated with an approximate 70% probability of obliteration [4, 28]. At the second procedure, only the small remnant need be irradiated, usually at a dose higher than the first dose delivered (especially if the intial AVM was large and the remnant is small, depending on location) (Figs. 1 and 2).
Angiogram before radiosurgery showing a ponto-medullary AVM in a 13-year-old boy who presented with hemorrhage (a, b). MRI before radiosurgery showing the brainstem AVM (volume 2.0 cc, prescription dose 15 Gy) (c, d). Three years later, the vertebral angiogram and MRI scan show complete AVM obliteration (e, f, g, h)
AVM nidus targeting
AVM obliteration is dependent on several factors and perhaps most importantly, proper stereotactic nidus definition followed by delivery of an adequate radiosurgery dose [29]. A complete analysis of 197 AVM patients with up to 3 year angiographic follow-up showed an overall complete obliteration rate of 72% after a single procedure. These results were stratified by volume. In 20 of 197 patients (10%), the targeted AVM nidus failed to obliterate totally. The most important reason for lack of complete obliteration was incomplete targeting [28]. An additional 35 patients (18%) had a residual AVM that was not included in the original treatment volume. Many of these patients then underwent a second radiosurgery procedure. Important obliteration factors were identified in this study: incomplete imaging definition of the AVM; reappearance of AVM after initial compression by hematoma; and recanalization of a previously embolized nidus. We and others advocate the use of multi-modality imaging (MRI, MRA, and conventional stereotactic angiography) to obtain the best results [30, 31]. For the smallest AVM (less than 1.3 ml), 90% of patients had complete obliteration (45 of 50), and 98% had obliteration of the target (49 of 50). For AVMs between 1.4 and 3 ml, 41 of 49 patients had complete obliteration (84%) and 47 of 49 had obliteration of the included target (96%). These data indicate that the radiosurgical dose will achieve our goal with a high likelihood if we can accurately tailor it to the entire lesion margin.
In a separate analysis of our data, we reported a multi-variate analysis of AVM obliteration as related to dose and volume [29]. A clear dose response up to 25 Gy was identified. We concluded that large AVMs have low obliteration rates because of the combination of lower treatment doses used and the greater problems encountered with target definition. An analysis of 95 patients with thalamic or basal ganglia AVMs found similar obliteration rates when stratified by volume; overall, 80% of patients were cured after a single procedure. Thus, AVM volume not only means that more tissue exists to undergo obliteration, but that there may be additional challenges in stereotactic targeting. It is interesting to speculate as to whether the AVM radiosurgery response in a child is different from in an adult. Some investigators believe that children respond faster, and there is anecdotal evidence that this may be true. We have seen complete angiography-confirmed AVM in a child 4 months following radiosurgery.
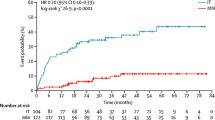
Does subtotal obliteration confer protection from hemorrhage? Liscak et al. reported that AVM obliteration was achieved in 222 (74%) of 330 patients after the initial stereotactic radiosurgery (SRS) and in 47 (69%) of 68 patients who underwent repeat SRS. Final angiography verified complete obliteration by 12 to 96 months (median, 25 months). Smaller volume AVMs and the application of a higher margin dose resulted in a higher chance of obliteration. The risk of rebleeding after SRS was 2.1% annually until full obliteration. The risks of permanent morbidity after the initial and repeat SRS were 2.7% and 2.9%, respectively [32]. Subtotal obliteration of AVMs after SRS implies a complete angiographic disappearance of the AVM nidus but persistence of an early filling draining vein, indicating that residual shunting is still present; hence, per definition, there is still a patent AVM, and the risk of bleeding is not eliminated.
The persistent risk of hemorrhage during the obliteration latency interval remains one of the strongest arguments against radiosurgery in some cases. Although Karlsson et al. reported protection from re-hemorrhage in the interval prior to complete obliteration, neither the Pittsburgh nor the University of Florida series identified such a benefit [13, 14, 37]. Maruyama et al. did a retrospective analysis involving 500 patients who had undergone radiosurgery noted a decrease of the bleeding risk by 54% during the latency period and by 88% after obliteration. They did not include the number of bleeding and analyzed one hemorrhage event after SRS for each patient because the Cox-proportional hazard method which they used in their series can allow one event for each patient. It would have affected their outcomes [38]. Yen et al. reported that there was no case of bleeding after the diagnosis of subtotally obliterated 159 AVMs (16 of 159 subtotally obliterated AVM patients underwent repeat SRS) at mean follow-up of 3.9 years after diagnosis of subtotally obliterated AVM [33]. The fact that none of the patients with subtotally obliterated AVMs suffered a rupture is not compatible with the assumption of an unchanged risk of hemorrhage for these lesions, and implies that the protection from rebleeding in patients with subtotal obliteration may be significant. Subtotal obliteration does not necessarily seem to be a stage of an ongoing obliteration. At least in some cases, it represents an end point of this process, with no subsequent obliteration occurring. This observation requires further confirmation by long-term follow-up imaging.
Most children with a symptomatic AVM present with hemorrhage. The timing between the bleed and radiosurgery can be important. Our decision on timing relates to our ability to identify the target AVM tissue on imaging, free from hematoma compression. If a hematoma obscures identification of the nidus, then several months should elapse for blood to resorb. Maruyama et al. retrospectively studied 211 patients with AVMs who presented with hemorrhage and underwent gamma knife surgery (GKS) as the initial treatment. Patients were categorized into three groups according to the interval between the time of first hemorrhage and GKS, as follows: group 1, 0–3 months (70 patients); group 2, 3–6 months (62 patients); and group 3, >6 months (79 patients). After a median follow-up of 6.3 years, the rates of obliteration, hemorrhage after treatment, and complication were not significantly different between the three groups even though the patients with a longer interval before GKS (group 3) had more AVMs in eloquent areas and neurological deficits. However, the number of patients with preoperative hemorrhage in the interval before GKS was significantly higher in group 3 (1, 3, and 20 patients in groups 1, 2, and 3, respectively). These results were similar in the analyses of 127 patients presenting with intracerebral hemorrhage (ICH). They concluded that no benefit was detected in waiting for hematoma absorption until GKS after hemorrhage from AVM. Because of higher hemorrhagic risk until GKS > 6 months after hemorrhage, the authors recommend GKS within 6 months after hemorrhage [34].
Pikus et al. argued that the high rate of complete microsurgical resection in their 72 patient AVM series (99%), with 8% rate of new permanent neurological deficts, substantiated their belief that resection was better than radiosurgery for small AVMs [35]. However, only three of their patients (4%) had AVMs in the basal ganglia, thalamus, or brainstem. Porter et al. constructed a decision analysis model based on obliteration estimates and morbidity rates for resection and radiosurgery [6]. They concluded that resection conferred a clinical benefit because of early protection from hemorrhage. Radiosurgery became a superior treatment if the surgical morbidity rate exceeded 12%. They did not factor the use of second stage or repeat radiosurgery into their model, choosing to leave patients with subtotally obliterated AVMs “unprotected” for the rest of their expected life. This outcome is rare since most patients achieve complete obliteration but may require more than one procedure. Thus, how obliteration data is used and from where it is obtained (brain locations) is paramount to construct a proper argument on the use of different techniques.
Post-radiosurgery morbidity
Since immediate post-radiosurgery complications are rare, many patients and physicians choose radiosurgery because of rapid return to activities and employment. The risk of radiation effects with a permanent neurological deficit is 2% to 3% in most reports [32, 36]. Post-radiosurgery seizures are rare when we administer therapeutic levels of anti-convulsant medication to patients with supratentorial lobar AVMs. One must consider the chance for delayed morbidity after radiosurgery that corresponds with the time course for AVM obliteration. We found that the rate of developing any post-radiosurgery imaging change between 2 and 7 years after radiosurgery is 30% [12]. We believe that the majority of these changes are hemodynamic or inflammatory. Most do not cause neurologic symptoms. Symptomatic imaging changes are found in 10%. A multi-variate analysis of imaging changes with various radiosurgical parameters found that the only significant independent correlation was the total volume of tissue that received ≥12 Gy [11]. These changes resolve in half the patients within 3 years of onset as compared to a 95% resolution rate in patients with asymptomatic imaging findings.
Options for large AVMs: staged volume radiosurgery and embolization
We prospectively began to stage anatomic components in order to deliver higher single doses to symptomatic AVMs >15 ml in volume. The experience of this approach in children has been limited. Twenty-eight patients (adults and children) with a large AVM underwent staged SRS at median follow-up of 50 months after the last SRS. Of 14 patients followed for more than 3 years, seven (50%) had total, four (29%) near total, and three (21%) had moderate AVM obliteration [39]. We now consider prospective staged radiosurgery for larger AVMs (volume staging) especially for patients who present with hemorrhage and who are not suitable for resection. We separate the AVM radiosurgeries by 4 to 6 months to allow repair of sub-lethal deoxyribonucleic acid damage in normal brain [40]. There is evidence to suggest that even incompletely obliterated AVMs may become easier to resect after a period of several years. Perhaps prophylactic staged radiosurgery may facilitate eventual resection of AVMs previously considered untreatable [41]. This approach is a relatively new one, and outcomes are being evaluated currently.
In selected cases, endovascular embolization can reduce the volume of the AVM nidus in preparation for eventual radiosurgery, usually 4 to 6 weeks later. In some patients, this strategy proved effective, and permanent occlusion of both of the embolized portion and the irradiated portion was the result. We continue to perform embolization if there is a high likelihood of significant volume reduction following that procedure. Embolization must also be performed with a reasonable risk to benefit ratio. If our neurointerventional team does not believe that significant feeding artery and nidus occlusion is likely, we consider a staged radiosurgery approach. There is no substantive data to suggest that incomplete embolization reduces the risk of a bleeding event during the latency interval after radiosurgey.
Differences between pediatric AVM and adult AVM patients
Compared with adults, children with AVMs are more likely to present with hemorrhage, and mortality rates from bleeding as high as 25% have been reported in our previous series [42]. The annual bleeding rate may also be slightly higher in children than in adults [43]. Children who undergo angiographic micro- or radiosurgical obliteration of their AVMs are at an increased risk for future recurrence of the condition. Immature, angiographically undetectable vessels left untreated in the periphery of the treated AVM may have the potential for growth and possibly recanalization of the AVM [44]. In addition, recanalization of the thrombosed vessels after radiosurgery may account for AVM regrowth [45]. Nicolato, et al. [46] performed radiosurgery in 63 pediatric patients. The majority (79%) presented after a hemorrhage; 47 patients (75%) had AVMs located in critical or deep locations. Using a mean AVM margin dose of 21.6 Gy, the 4-year actuarial obliteration rate was 77%. No patient experienced bleeding after radiosurgery, and the radiation-related complication rate was 2%. Authors of other studies have confirmed these findings, reporting obliteration rates from 61% to 87% and radiation-related morbidity rates from 0% to 2.5% [47–50]. Pan et al. reported that 105 pediatric AVM patients who underwent SRS had total obliteration rate of 65% at 4 years and had 8% morbidity rate and <1% mortality rate [51]. In their series, post-treatment hemorrhage occurred in four (4%) of 105 patients. Obliteration rates at 48 months of small and extremely large (>20 ml) AVMs were similar in the pediatric and adult groups, whereas AVMs between 3 and 10 ml responded less efficaciously in children. The AVMs with volumes ranging from 10 to 20 ml were also associated with a lower obliteration rate in children at 48 months, but statistical significance was not reached.
Summary
AVM radiosurgery has been in practice for over 40 years and is now a common method to manage properly selected patients with brain AVMs. The techniques have been refined along with our understanding of the expected response. It is this understanding of expected outcomes that should allow a rational discussion of the pertinent issues for management of patients with AVMs. Some patients will require multi-modality approaches. Although not commonly performed at present, children whose AVMs were obliterated after radiosurgery should consider repeat angiography after they reach adulthood to rule out the possibility of a recurrent nidus that would expose them to an ongoing risk of hemorrhage.
References
Friedman W, Bova F (1992) Linear accelerator radiosurgery for arteriovenous malformations. J Neurosurg 77:832–841
Lunsford LD, Kondziolka D, Flickinger J, Bissonette D, Jungreis CA, Horton JA, Maitz AH, Coffey RJ (1991) Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg 75:512–524
Pollock B, Flickinger JC, Lunsford LD, Maitz A, Kondziolka D (1998) Factors associated with successful arteriovenous malformation radiosurgery. Neurosurgery 42:1239–1247
Maesawa S, Flickinger JC, Kondziolka D, Lunsford LD (2000) Repeated radiosurgery for incompletely obliterated arteriovenous malformations. J Neurosurg 92:961–970
Yamamoto M, Jimbo M, Hara M, Saito I, Mori K (1996) Gamma knife radiosurgery for arteriovenous malformations: long-term follow-up results focusing on complications occurring more than 5 years after irradiation. Neurosurgery 38:906–914
Porter P, Shin A, Detsky A et al (1997) Surgery versus radiosurgery for small, operable cerebral arteriovenous malformations: a clinical and cost comparison. Neurosurgery 41:757–766
Betti O, Munari C, Rosler R (1989) Stereotactic radiosurgery with the linear accelerator: treatment of arteriovenous malformations. Neurosurgery 24:311–321
Colombo F, Benedetti A, Pozza F, Marchetti C, Chierego G (1989) Linear accelerator radiosurgery of cerebral arteriovenous malformations. Neurosurgery 24:833–840
Yamamoto Y, Coffey R, Nichols B, Shaw EG (1995) Interim report on the radiosurgical treatment of cerebral arteriovenous malformations. J Neurosurg 83:832–837
Pollock BE, Lunsford LD, Kondziolka D, Maitz A, Flickinger JC (1994) Patient outcomes after stereotactic radiosurgery for “operable” arteriovenous malformations. Neurosurgery 35:1–8
Flickinger JC, Kondziolka D, Pollock B, Maitz A, Lunsford LD (1997) Complications from arteriovenous malformation radiosurgery: multivariate analysis and risk modeling. Int J Radiat Oncol Biol Phys 38:485–490
Flickinger JC, Kondziolka D, Maitz A, Lunsford LD (1998) Analysis of neurological sequelae from radiosurgery of arteriovenous malformations: how location affects outcome. Int J Radiat Oncol Biol Phys 40:273–278
Friedman W, Blatt D, Bova F, Buatti J, Mendenhall W, Kubilis P (1996) The risk of hemorrhage after radiosurgery for arteriovenous malformations. J Neurosurg 84:912–919
Karlsson B, Lindquist C, Steiner L (1996) Effect of gamma knife surgery on the risk of rupture prior to AVM obliteration. Minim Invasive Neurosurg 39:21–27
Flickinger JC, Kondziolka D, Lunsford LD, Pollock B, Yamamoto M, Gorman D, Sneed P, Larson D, Smith V, McDermott M, Miyawaki L, Chilton J, Morantz R, Young B, Jokura H, Liscak R (1999) A multi-institutional analysis of complication outcomes after arteriovenous malformation radiosurgery. Int J Radiat Oncol Biol Phys 44:67–74
Schneider B, Eberhard D, Steiner L (1997) Histopathology of arteriovenous malformations after gamma knife radiosurgery. J Neurosurg 87:352–357
Wu A, Lindner G, Maitz A, Kalend AM, Lunsford LD, Flickinger JC, Bloomer WD (1990) Physics of gamma knife approach on convergent beams in stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 18:941–949
Kondziolka D, Lunsford LD (1993) Intraparenchymal brainstem radiosurgery. Neurosurg Clin N Am 4:469–479
Flickinger JC (1989) An integrated logistic formula for prediction of complications from radiosurgery. Int J Radiat Oncol Biol Phys 17:879–885
Flickinger JC, Lunsford LD, Kondziolka D (1992) Dose prescription and dose volume effects in radiosurgery. Neurosurg Clin N Am 3:51–59
Szeifert GT, Kemeny AA, Timperley W, Walter R, Forster D (1997) The potential role of myofibroblasts in the obliteration of arteriovenous malformations after radiosurgery. Neurosurgery 40:61–66
Hara M, Nakamura M, Shiokawa Y, Sawa H, Sato E, Koyasu H, Saito I (1998) Delayed cyst formation after radiosurgery for cerebral arteriovenous malformation: two case reports. Minim Invasive Neurosurg 41:40–45
Gerszten PC, Adelson PD, Kondziolka D, Flickinger J, Lunsford D (1996) Seizure outcome in children treated for arteriovenous malformations after gamma knife radiosurgery. Ped Neurosurg 24:139–144
Huang CF, Somaza S, Lunsford LD, Kondziolka D, Flickinger J (1996) Radiosurgery in the management of epilepsy associated with arteriovenous malformations. Radiosurgery 1:19–200
Steiner L, Lindquist C, Adler JR, Torner J, Alves W, Steiner M (1992) Clinical outcome of radiosurgery for cerebral arteriovenous malformations. J Neurosurg 77:1–8
Karlsson B, Kihlstrom L, Lindquist C, Steiner L (1998) Gamma knife surgery for previously irradiated arteriovenous malformations. Neurosurgery 42:1–6
Karlsson B, Lindquist M, Lindquist C (1996) Long-term angiographic outcome of arteriovenous malformations responding incompletely to gamma knife surgery. Radiosurgery 1:188–194
Pollock BE, Kondziolka D, Lunsford LD, Bissonette D, Flickinger J (1996) Repeat stereotactic radiosurgery of arteriovenous malformations: factors associated with incomplete obliteration. Neurosurgery 38:318–324
Flickinger JC, Pollock BE, Kondziolka D, Lunsford LD (1996) A dose-response analysis of arteriovenous malformation obliteration after radiosurgery. Int J Radiat Oncol Biol Phys 36:873–879
Friedman W, Bova F, Mendenhall W (1995) Linear accelerator radiosurgery for arteriovenous malformations: the relationship of size to outcome. J Neurosurg 82:180–189
Kondziolka D, Lunsford LD, Kanal E, Talagala L (1994) Stereotactic magnetic resonance angiography for targeting in arteriovenous malformation radiosurgery. Neurosurgery 35:585–591
Lišcák R, Vladyka V, Šimonová G, Urgošík D, Novotný J, Janoušková L, Vymazal J (2007) Arteriovenous malformations after Leksell gamma knife radiosurgery: rate of obliteration and complications. Neurosurgery 60:1005–1014
Yen CP, Varady P, Sheehan J, Steiner M, Steiner L (2007) Subtotal obliteration of cerebral arteriovenous malformations after gamma knife surgery. J Neurosurg 106:361–369
Maruyama K, Koga T, Shin M, Igaki H, Tago M, Saito N (2008) Optimal timing for gamma knife surgery after hemorrhage from brain arteriovenous malformations. J Neurosurg 109(Suppl):73–76
Pikus H, Beach ML, Harbaugh R (1998) Microsurgical treatment of arteriovenous malformations: analysis and comparison to stereotactic radiosurgery. J Neurosurg 88:641–646
Pollock BE, Meyer FB (2004) Radiosurgery for arteriovenous malformations. J Neurosurg 101:390–392
Pollock BE, Flickinger JC, Lunsford LD, Bissonette D, Kondziolka D (1996) Hemorrhage risk after radiosurgery for arteriovenous malformations. Neurosurgery 38:652–661
Maruyama K, Kawahara N, Shin M, Tago M, Kishimoto J, Kurita H, Kawamoto S, Morita A, Kirino T (2005) The risk of hemorrhage after radiosurgery for cerebral arteriovenous malformations. N Engl J Med 352:146–153
Sirin S, Kondziolka D, Niranjan A, Flickinger JC, Maitz A, Lunsford LD (2006) Prospective staged volume radiosurgery for large arteriovenous malformations: indications and outcomes in otherwise untreatable patients. Neurosurgery 58:17–27
Firlik A, Levy E, Kondziolka D, Yonas H (1998) Staged volume radiosurgery and resection: a new treatment for a giant arteriovenous malformation. Neurosurgery 43:1223–1228
Steinberg G, Chang S, Levy R, Marks M, Frankel K, Marcellus M (1996) Surgical resection of large incompletely treated intracranial arteriovenous malformations following stereotactic radiosurgery. J Neurosurg 84:920–928
Kondziolka D, Humphreys RP, Hoffman HJ, Hendrick EB, Drake JM (1992) Arteriovenous malformations of the brain in children: a forty year experience. Can J Neurol Sci 19:40–45
Smith ER, Butler WE, Ogilvy CS (2002) Surgical approaches to vascular anomalies of the child's brain. Curr Opin Neurol 15:165–171
Rodríguez-Arias C, Martínez R, Rey G, Bravo G (2000) Recurrence in a different location of a cerebral arteriovenous malformation in a child after radiosurgery. Childs Nerv Syst 16:363–365
Lindqvist M, Karlsson B, Guo WY, Kihlström L, Lippitz B, Yamamoto M (2000) Angiographic long-term follow-up data for arteriovenous malformations previously proven to be obliterated after gamma knife radiosurgery. Neurosurgery 46:803–808
Nicolato A, Foroni R, Seghedoni A, Martines V, Lupidi F, Zampieri P, Sandri M, Ricci U, Mazza C, Beltramello A, Gerosa M, Bricolo A (2005) Leksell gamma knife radiosurgery for cerebral arteriovenous malformations in pediatric patients. Childs Nerv Syst 21:301–307
Levy EI, Niranjan A, Thompson TP, Scarrow AM, Kondziolka D, Flickinger JC, Lunsford LD (2000) Radiosurgery for childhood intracranial arteriovenous malformations. Neurosurgery 47:834–842
Nataf F, Schlienger M, Lefkopoulos D, Merienne L, Ghossoub M, Foulqier JN, Deniaud-Alexandre A, Mammar H, Meder JF, Turak B, Huart J, Touboul E, Roux RF (2003) Radiosurgery of cerebral arteriovenous malformations in children: a series of 57 cases. Int J Radiat Oncol Biol Phys 57:184–195
Shin M, Kawamoto S, Kurita H, Tago M, Sasaki T, Morita A, Ueki K, Kirino T (2002) Retrospective analysis of a 10-year experience of stereotactic radiosurgery for arteriovenous malformations in children and adolescence. J Neurosurg 97:779–784
Cohen-Gadol AA, Pollock BE (2006) Radiosurgery for arteriovenous malformation in children. J Neurosurg Pediatr 104:388–391
Pan DH, Kuo YH, Guo Wu, Chung WY, Wu HM, Liu KD, Chang YC, Wang LW, Wong TT (2008) Gamma knife surgery for cerebral arteriovenous malformations in children: a 13-year experience. J Neurosurg Pediatr 1:296–304
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kondziolka, D., Kano, H., Yang, Hc. et al. Radiosurgical management of pediatric arteriovenous malformations. Childs Nerv Syst 26, 1359–1366 (2010). https://doi.org/10.1007/s00381-010-1207-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1207-x