Abstract
Object
Brain tumors are the most common solid tumors in children and their prognosis is poor. Epidemiologic data from a population-based cancer registry provide the information necessary to determine the incidence rate of pediatric brain tumors. The aim of this study was to determine the epidemiology of childhood primary intracranial tumors in Kumamoto Prefecture, Japan.
Methods
We surveyed 210 patients younger than 15 years who were diagnosed with primary intracranial tumors between 1989 and 2008; 159 (75.7%) of the tumors were confirmed microscopically.
Results
The age-adjusted annual incidence rate was 36.1 cases per million children. The boys/girls ratio was 1.31. The age-specific annual incidence rate was 28.5-, 40.9-, and 38.4 cases per million for the 0- to 4-, 5- to 9-, and 10- to 14-year age group, respectively. The incidence was highest in 10- to 14-year-old boys (53.6 per million) and lowest in 10- to 14-year-old girls (22.6 per million). The most common tumor was astrocytoma (35.7%) with an annual incidence rate of 13.2 per million, followed by germ cell tumor (14.3%, 5.0 per million), craniopharyngioma (10.5%, 3.8 per million), medulloblastoma (10.0%, 3.7 per million), and ependymoma (4.8%, 1.5 per million). The distribution of the tumor type varied with the patient age and gender. Although there were no germ cell tumors in 0- to 4-year-old boys, they were the second-most common tumor in 10- to 14-year-old boys. Conversely, while there were no medulloblastomas in 10- to 14-year-old girls, their incidence was high in 0- to 4-year-old girls.
Conclusions
In this Kumamoto survey, the incidence rate of primary intracranial tumors in children was similar to that in Western countries. However, the incidence and relative frequency of particular histological types of childhood brain tumors such as germ cell tumors and craniopharyngiomas were different between Japan and Western countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain tumors are the most common solid tumors in children younger than 15 years. According to data from cancer registries, brain tumors represent more than 20% of all childhood cancers. Although compared to other ethnicities the incidence of intracranial tumors is low in Asian populations, we reported elsewhere that the overall age-adjusted incidence rate in Western and Asian countries was almost the same [1]. On the other hand, for some types of tumor, the incidence is different in different ethnic populations. For example, the incidence of germ cell tumors is higher in Orientals than Westerners [2, 3]. To obtain an accurate population-based epidemiological survey, we investigated the incidence of intracranial tumors in Japanese children living in Kumamoto Prefecture between 1989 and 2008.
Methods
Study population
Kumamoto Prefecture (population 1,850,000) is located in the center of Kyushu Island in the southern part of Japan. Of its population, 288,000 (15.5%) are children younger than 15 years. According to the decennial census, population movement into and out of Kumamoto Prefecture is negligible. Between 1989 and 2008, 5,448 new cases of primary intracranial tumors were diagnosed at 32 hospitals in Kumamoto Prefecture. These institutions have expert professional staff and modern equipment, including computed tomography (CT)- and/or magnetic resonance imaging (MRI) scanners to diagnose and treat patients with intracranial tumors.
Summary of registered patients
Information on all new patients with primary intracranial tumors diagnosed in the 32 hospitals between 1989 and 2008 was logged. Registration information included the patient's age, sex, address, the date of diagnosis, and the pathological diagnosis. All information was carefully scrutinized to eliminate double registration. A resident was defined as any individual who lived within the physical limits of Kumamoto Prefecture for at least 1 year prior to the diagnosis. We recorded as the incidence date the first day of the hospital stay during which the diagnosis was made for inpatients; for outpatients, it was the date on which diagnostic CT or MRI scans were obtained. Tumors not verified histologically were included if clinical records and neuroimaging studies resulted in a tumor diagnosis. No diagnoses were obtained primarily at autopsy during the period covered by this study.
Incidence rate
Age-adjusted incidence rates were calculated by the direct method using 5-year age groupings, with the incidence in the total Japanese population in 2000 as the standard. Population figures were obtained from published decennial tabulations for Kumamoto Prefecture and Japan. The adjusted rates allow an overall comparison among different populations because the rates are standardized for dissimilarities in the age and sex distribution. Age-specific incidence rates were calculated for all intracranial tumors and for each type of intracranial tumor. Throughout this manuscript, incidence rates are expressed as cases per million child population (0–14 years).
Results
During the 20-year period from 1989 to 2008, 5,448 new cases of primary intracranial tumors were diagnosed in Kumamoto Prefecture. There was a constant year-to-year increase in the number of diagnosed tumors. Of the 5,448 primary intracranial tumors, 210 (3.9%) were in children younger than 15 years. The number of children with brain tumors diagnosed each year in Kumamoto Prefecture was relatively constant; among 288,000 children surveyed for the 20-year period (1989–2008), the age-adjusted annual incidence rate was 36.1 per million child population. The incidence rate was 39.3 for boys and 30.0 for girls, resulting in a boys:girls ratio of 1.31:1 (Table 1).
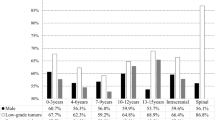
As shown in Fig. 1, the age-specific incidence of primary intracranial tumors was different among different age groups. The total incidence was 28.5, 40.9, and 38.4 in the 0–4-, 5–9-, and 10–14-year age group, respectively. There was no significant difference in the incidence rate between boys and girls in the 0–4- and 5–9-year group. However, among children in the 10–14-year group, the incidence was higher for boys than girls (53.6 vs. 22.6 per million per year).
In 159 of the 210 patients in this series (75.7%), the diagnosis was based on histological evidence. As shown in Table 2, the rate of histological confirmation of different tumor types varied (craniopharyngiomas, 95.5%; medulloblastomas, 95.2%; germ cell tumors, 73.3%). Diagnoses of germ cell tumors without histological confirmation were based on markers in serum and cerebrospinal fluid (CSF) and characteristic neuroimaging evidence in pineal and suprasellar regions.
Of the tumors, 35.7% were astrocytomas, 14.3% were germ cell tumors, 10.5% were craniopharyngiomas, 10% were medulloblastomas, and 4.8% were ependymomas. The age-adjusted incidence rate per million child populations per year was 13.2 for astrocytomas, 5.0 for germ cell tumors, 3.8 for craniopharyngiomas, 3.7 for medulloblastomas, and 1.5 for ependymomas (Table 1).
Regarding the distribution of primary intracranial tumors by gender, astrocytomas were the most common tumor in boys (36.0%; incidence rate 15.6 per million per year) and girls (35.3%, incidence rate of 10.7). In boys, the second-most common tumors were germ cell tumors (18.4%, incidence rate 7.6 per million per year), followed by craniopharyngiomas (8.0%, incidence rate 3.4), medulloblastomas (6.4%, incidence rate 2.6), and ependymomas (4.8%, incidence rate 1.7). In girls, the second-most common tumors were medulloblastomas (15.3%, incidence rate 4.8) followed by craniopharyngiomas (14.1%, incidence rate 4.2), germ cell tumors (8.2%, incidence rate 2.4), and ependymomas (4.7%, incidence rate 1.3). There was a gender difference in astrocytomas, germ cell tumors, and ependymomas; the boys:girls ratio was 1.46:1, 3.17:1, and 1.31:1, respectively.
Figure 2 shows the predominant tumor types with the patients' age at diagnosis. In all age groups and both sexes, the most common tumor type was astrocytoma; the incidence in boys in the 10–14-year age group was 18.1 per million per year. In 0–4-year-old boys, craniopharyngiomas were the second-most common tumors with an age-specific incidence of 2.3 per million per year, followed by medulloblastomas (incidence rate 1.1). No germ cell tumors were diagnosed in 0–4-year-old boys. In girls, medulloblastomas were the second-most common tumors with an age-specific incidence of 7.1 per million per year, followed by craniopharyngiomas (incidence rate 2.4), and germ cell tumors (incidence rate 1.2). In 5–9-year-old boys, germ cell tumors were the second-most common tumors with an age-specific incidence of 7.3 per million per year, followed by craniopharyngiomas and medulloblastomas (incidence rate for both = 5.2). Among girls, craniopharyngiomas and medulloblastomas were the second-most common tumors with an age-specific incidence of 7.6 per million per year, followed by germ cell tumors (incidence rate 3.3). In 10–14-year-old boys, germ cell tumors were the second-most common tumors (age-specific incidence 14.5 per million per year) followed by craniopharyngioma (incidence rate 2.7), and medulloblastoma (incidence rate 1.8). In girls, craniopharyngiomas and germ cell tumors were the second-most common tumors; the age-specific incidence was 2.8 per million per year. No medulloblastomas were diagnosed in 10–14-year-old girls.
Discussion
There are several reports documenting incidence rates of childhood primary intracranial tumors; the annual incidence of these tumors ranges from 24 to 45 per million child population [4–8]. In 2006, Peris-Bonet et al. [9] presented compiled data from the European Automated Childhood Cancer Information System Project; 59 cancer registries in 19 European countries participated in this study and 11,829 cases of primary central nervous system (CNS) tumors in children were recorded. The overall age-standardized incidence rate (ASR) of CNS tumors in European children was 29.9 per million child population, with the highest rates recorded in northern Europe (43.8 per million). According to the 2008 U.S. Central Brain Tumor Registry, the ASR in the USA (2004–2005) was 45.8 per million [10]. Lower rates were recorded for South America, Africa, and Asia [11]. The ASR we documented in 1996 for Kumamoto Prefecture was 34.3 per million [2], and our present survey indicated an ASR of 36.1 per million, almost the same as in Western countries (Table 3).
In our study, the incidence rate for intracranial tumors was male-dominant (boys:girls, 1.31:1) and close to that previously reported for other Asian countries [3, 12, 13]. In several Western countries, the gender ratio was close to 1.0; it was 1.03 according to the Swedish Registry [14], 1.08 in Canada [15], 1.15 in Denmark [4], and 1.10 in France [16]. Rorke and Schut [17] attributed the male predominance of pediatric brain tumors to the gender distribution ratio in the normal childhood population. In Kumamoto Prefecture, the gender ratio for the population younger than 15 years was 1.05 in the year 2000, indicating that the difference in the incidence rate reflects gender differences. According to our data, the male:female ratio of germ cell tumors and astrocytomas was 3.17:1 and 1.46:1, respectively.
In our study population, the incidence of intracranial tumors was lowest at 28.5 per million per year in children aged 0–4 years; it was 40.9 in 5–9-year olds, and 38.4 in the 10–14-year age group. In Shanghai, the incidence of CNS tumors was also lowest in the 0–4-year age group [7]. According to others, children in the 0–4-year age group had the highest incidence of intracranial tumors [10, 11, 18]. In our survey, the highest incidence for boys was 53.6 per million per year in the 10–14-year age group; it was 18.1 for astrocytomas and 14.5 for germ cell tumors. For girls, the incidence was highest in the 5–9-year group (38.0 per million per year); it was 14.1 for astrocytomas. These findings may explain the higher incidence of brain tumors in these age groups compared to the 0–4-year age group.
Histologically, astrocytomas were the most common tumors in our study (35.7%, annual incidence rate 13.2 per million) followed by germ cell tumors (14.3%, 5.0 per million per year), craniopharyngiomas (10.5%, 3.8 per million per year), medulloblastomas (10.0%, 3.7 per million per year), and ependymomas (4.8%, 1.5 per million per year) (Table 4). In other studies, astrocytomas were the most common tumors throughout childhood and adolescence; their incidence rate ranged from 10 to 19 per million per year [5, 6] and was similar to the rate in our survey.
The second-most common pediatric brain tumor is medulloblastoma; its reported incidence rate was 5–7 per million per year [5, 6, 10]. In our survey, its annual incidence rate was 3.7 and medulloblastomas were the 4th most common tumors. According to an international survey by the International Agency for Research on Cancer (IARC) performed in the 1980s and 1990s, Asia and South Africa manifested the lowest rate of medulloblastoma [19, 20]. More recent reports from Asian countries indicated that medulloblastoma was the 2nd or 3rd most common brain tumor in children; it was the 2nd most common tumor in Korean children (17.9%) [12] and the 3rd most common among Taiwanese children (13.2%) [3] and children surveyed in Beijing (16.6%) [13]. At present, we cannot explain the difference in the incidence rate among Asian countries.
Germ cell tumors were the second-most common tumors in our survey (14.3%, annual incidence 5.0 per million); these data are similar to reports from Taiwan (14.0%) [3] and Korea (11.2%) [12] and compared to children from Western countries where the incidence of germ cell tumors was 0.4–4.5% [20, 21], it was high in Asian countries. Furthermore, the incidence of craniopharyngioma at 10.5% was higher in our survey than in previous reports from Western countries (3.9–7.6%). The incidence in our survey (3.8 per million per year) was higher than in a Swedish study (2.2 per million) [6] and a report from Italy (1.4 per million) [22], and the USA (1.6 per million) [10]. Earlier reports suggested that craniopharyngiomas occurred more frequently in Asian and African children [12, 13, 23, 24].
Our findings indicate that there are differences between Japan and Western countries with respect to the incidence rate and relative frequency of particular histological types of childhood brain tumors such as germ cell tumors and craniopharyngiomas. Genetic and/or environmental factors may play a role in the tumorigenesis of intracranial tumors in children.
Conclusions
Epidemiologic data from a population-based cancer registry provide the information necessary to determine the incidence rate of pediatric brain tumors. However, pitfalls for population-based survey of brain tumors in children through childhood cancer registries or childhood brain tumor registries were incompleteness of patient registration that may lead to underestimation. Bias also exists for not including benign tumors or tumors without histologic verification. Since 1989, we have collected information on all new patients with primary intracranial tumors diagnosed by CT or MRI at the 32 hospitals in Kumamoto Prefecture. We surveyed 210 patients younger than 15 years between 1989 and 2008. Among them, 159 (75.7%) of the tumors were confirmed microscopically. Furthermore, in order to standardize for dissimilarities in the age and sex distribution, age-adjusted incidence rates were calculated by the direct method using 5-year age grouping in the total Japanese population in 2000 as the standard. Therefore, this survey may be data representative of primary pediatric intracranial tumors in a geographic region and allow an overall comparison among different populations.
References
Kuratsu J, Takeshima H, Ushio Y (2001) Trends in the incidence of primary intracranial tumors in Kumamoto, Japan. Int J Clin Oncol 6:183–191
Kuratsu J, Ushio Y (1996) Epidemiological study of primary intracranial tumors in childhood. A population-based survey in Kumamoto Prefecture, Japan. Pediatr Neurosurg 25:240–246, discussion 247
Wong TT, Ho DM, Chang KP, Yen SH, Guo WY, Chang FC, Liang ML, Pan HC, Chung WY (2005) Primary pediatric brain tumors: statistics of Taipei VGH, Taiwan (1975–2004). Cancer 104:2156–2167
Gjerris F, Agerlin N, Borgesen SE, Buhl L, Haase J, Klinken L, Mortensen AC, Olsen JH, Ovesen N, Reske-Nielsen E, Schmidt K (1998) Epidemiology and prognosis in children treated for intracranial tumours in Denmark 1960–1984. Childs Nerv Syst 14:302–311
Kaatsch P, Rickert CH, Kuhl J, Schuz J, Michaelis J (2001) Population-based epidemiologic data on brain tumors in German children. Cancer 92:3155–3164
Lannering B, Sandstrom PE, Holm S, Lundgren J, Pfeifer S, Samuelsson U, Stromberg B, Gustafsson G (2009) Classification, incidence and survival analyses of children with CNS tumours diagnosed in Sweden 1984–2005. Acta Paediatr 98:1620–1627
Bao PP, Zheng Y, Wang CF, Gu K, Jin F, Lu W (2009) Time trends and characteristics of childhood cancer among children age 0–14 in Shanghai. Pediatr Blood Cancer 53:13–16
Kaatsch P, Steliarova-Foucher E, Crocetti E, Magnani C, Spix C, Zambon P (2006) Time trends of cancer incidence in European children (1978–1997): report from the Automated Childhood Cancer Information System project. Eur J Cancer 42:1961–1971
Peris-Bonet R, Martinez-Garcia C, Lacour B, Petrovich S, Giner-Ripoll B, Navajas A, Steliarova-Foucher E (2006) Childhood central nervous system tumours—incidence and survival in Europe (1978–1997): report from Automated Childhood Cancer Information System project. Eur J Cancer 42:2064–2080
CBTRUS Central Brain Tumor Registry of the United States, Statistical Report 2000–2004 and Statistical Report Supplement 2004, 2008
Wohrer A, Waldhor T, Heinzl H, Hackl M, Feichtinger J, Gruber-Mosenbacher U, Kiefer A, Maier H, Motz R, Reiner-Concin A, Richling B, Idriceanu C, Scarpatetti M, Sedivy R, Bankl HC, Stiglbauer W, Preusser M, Rossler K, Hainfellner JA (2009) The Austrian Brain Tumour Registry: a cooperative way to establish a population-based brain tumour registry. J Neurooncol 95:401–411
Cho KT, Wang KC, Kim SK, Shin SH, Chi JG, Cho BK (2002) Pediatric brain tumors: statistics of SNUH, Korea (1959–2000). Childs Nerv Syst 18:30–37
Zhou D, Zhang Y, Liu H, Luo S, Luo L, Dai K (2008) Epidemiology of nervous system tumors in children: a survey of 1,485 cases in Beijing Tiantan Hospital from 2001 to 2005. Pediatr Neurosurg 44:97–103
Hjalmars U, Kulldorff M, Wahlqvist Y, Lannering B (1999) Increased incidence rates but no space-time clustering of childhood astrocytoma in Sweden, 1973–1992: a population-based study of pediatric brain tumors. Cancer 85:2077–2090
Keene DL, Hsu E, Ventureyra E (1999) Brain tumors in childhood and adolescence. Pediatr Neurol 20:198–203
Bauchet L, Rigau V, Mathieu-Daude H, Fabbro-Peray P, Palenzuela G, Figarella-Branger D, Moritz J, Puget S, Bauchet F, Pallusseau L, Duffau H, Coubes P, Tretarre B, Labrousse F, Dhellemmes P (2009) Clinical epidemiology for childhood primary central nervous system tumors. J Neurooncol 92:87–98
Rorke LB, Schut L (1989) Introductory survey of pediatric brain tumors. In: McLaurin RL, Schut L, Venes JL, Epstein F (eds) Pediatric neurosurgery, 2nd edn. WB Saunders, Philadelphia, pp 335–337
Farwell JR, Dohrmann GJ, Flannery JT (1977) Central nervous system tumors in children. Cancer 40:3123–3132
Mori K, Kurisaka M (1986) Brain tumors in childhood: statistical analysis of cases from the Brain Tumor Registry of Japan. Childs Nerv Syst 2:233–237
Stiller CA, Nectoux J (1994) International incidence of childhood brain and spinal tumours. Int J Epidemiol 23:458–464
Heiskanen O (1977) Intracranial tumors of children. Childs Brain 3:69–78
Haupt R, Magnani C, Pavanello M, Caruso S, Dama E, Garre ML (2006) Epidemiological aspects of craniopharyngioma. J Pediatr Endocrinol Metab 19(Suppl 1):289–293
Aghadiuno PU, Adeloye A, Olumide AA, Nottidge VA (1985) Intracranial neoplasms in children in Ibadan, Nigeria. Childs Nerv Syst 1:39–44
Kadri H, Mawla AA, Murad L (2005) Incidence of childhood brain tumors in Syria (1993–2002). Pediatr Neurosurg 41:173–177
Disclaimer
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Makino, K., Nakamura, H., Yano, S. et al. Population-based epidemiological study of primary intracranial tumors in childhood. Childs Nerv Syst 26, 1029–1034 (2010). https://doi.org/10.1007/s00381-010-1126-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1126-x