Abstract
Purpose
Our aim was to improve diagnosis and management of pseudotumor cerebri (PTC; also known as idiopathic intracranial hypertension) in children.
Methods
We performed a comprehensive analysis of epidemiology, diagnostic work-up, therapy, and clinical follow-up in 53 consecutive patients.
Results
We identified several important aspects to be considered in the management of these children. First, patients may present without obvious symptoms at diagnosis. Second, bilateral papilledema might not or not yet be present in symptomatic patients. Third, measurement of cerebrospinal fluid (CSF) opening pressure may not always be reliable due to drugs used for sedation, which may alter intracranial pressure. Fourth, normal CSF pressure values in childhood are not well established and diagnosis might even be justified if pressure is <20 cm H2O. Fifth, associated conditions are frequent (at least in our cohort); however, in most cases, a causative link cannot be proven. Finally, disease relapse is a serious problem (20% in our group), which stresses the importance of standardized follow-up programs.
Conclusions
PTC constitutes an important and possibly underrecognized disorder in children and adolescents. Considering the high percentage of possibly associated conditions in our study, a detailed diagnostic work-up is crucial to identify treatable underlying conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pseudotumor cerebri (PTC) is a syndrome of disturbed cerebrospinal fluid (CSF) hydrodynamics without identifiable cause [1]. By definition, patients with primary PTC have a normal CSF composition, a nonfocal neurological examination (except for abducens nerve palsy), and no evidence of hydrocephalus, cerebral mass lesion, or vascular abnormality on neuroimaging. PTC may be complicated by severe headaches and even permanent visual failure. There are several conditions that have been reported to be associated with secondary PTC [2]; however, in most of these studies, a clear proof for a causative link is missing.
Already recognized by Quincke in 1897 [3], the pathophysiology of PTC is still elusive. Different mechanisms have been hypothesized. Current theories involve (1) obstruction to CSF outflow through the arachnoid villi, (2) increased rate of CSF formation at the choroidal plexus, and (3) increased intracranial venous sinus pressure.
In addition to the unknown etiology, there is little standardization of diagnostic workup in children with PTC, and therapy is mainly based on empirical data. This particularly holds true for PTC in prepubertal children [4]. Importantly, the clinical characteristics of pediatric PTC are different compared to the typical syndrome of adulthood [4, 5]. This might indicate age-related differences in the etiology of PTC pointing to the necessity of age-adjusted diagnostic and therapeutic strategies. However, since PTC is a rare disorder in children, these problems have not been sufficiently addressed so far.
In this study, we performed a comprehensive analysis of diagnostic work-up, therapy, and clinical follow-up in 53 children and adolescents with the diagnosis of PTC. In order to present these patients in an unbiased manner, we did not subcategorize children into primary and secondary forms of PTC. However, we included and described all possibly causative conditions and summarized patients under the term PTC complex.
Materials and methods
All patients with a diagnosis of PTC complex who presented to the University Children’s Hospital, Düsseldorf, Germany, over the past 10 years from 1997 to 2007 were entered into this study.
Inclusion criteria
We defined PTC complex as follows: (1) clinical signs and/or symptoms of raised intracranial pressure (e.g., headache, visual disturbance, vomiting, papilledema) without additional abnormal neurological signs other than sixth nerve palsy, (2) normal neuroimaging studies by standard magnetic resonance imaging, (3) unremarkable examination of cerebrospinal fluid constituents, and (4) raised CSF pressure >20 cm H2O with the exception of prepubertal children with probable PTC [6]. This condition is characterized by a clinical manifestation and response to treatment consistent with PTC but a CSF opening pressure <20 cm H2O.
Children aged 11 years or younger were regarded as prepubertal. As a measure of obesity, body mass index (BMI) was expressed as kilograms per square meter. All children were defined as overweight on the basis of a BMI > 90th percentile and as obese if percentile for age and sex was >97th using the German BMI charts [7]. In all patients, a basic laboratory workup was performed (e.g., electrolytes, blood gases, red and white blood cell count, thyroid hormone status), which was extended in all oncological patients and those with atypical clinical presentation. The extent of papilledema was photodocumented at each visit. If age permitted, children were also tested for pseudopapilledema, visual acuity, and visual field defects. Lumbar puncture (LP) with measurement of CSF pressure and cellular, chemical, and microbiological examinations was performed in all patients. The opening pressure was measured in the flexed lateral decubitus position. If required moderately deep sedation with propofol was carried out.
For characterization of headaches, a simplified classification was used. We defined five types of headache according to the temporal pattern [8]: acute headache, acute recurrent headache, chronic progressive headache, chronic daily headache, and mixed headache.
Results
In total, 53 children with PTC complex were identified. An average of four newly diagnosed cases per year was observed.
Clinical presentation
The mean age at presentation was 10.4 years (range from 8 months to 17.5 years). We subclassified 32 children (13 girls, 19 boys) as prepubertal. In this subgroup, papilledema was present in all cases except two patients (nos. 1 and 9) who presented with abducens nerve palsy. The most common presenting symptom was headache (n = 16). Eleven children were symptom-free, and papilledema was found on routine eye examination. The mean CSF opening pressure in the prepubertal children was 30 cm H2O (range 18–60 cm H2O). Obesity was found in five of prepubertal children, and two patients were classified as overweight. All of these were older than 9 years. Nine patients were anemic (hemoglobin (Hb) < 12 g/l). In general, comorbidities could be identified in 16 patients (see Table 1).
Five prepubertal children were considered as “probable PTC” (see Table 1) [6]. Secondary causes were excluded in all of them. In patient nos. 1 and 26, a second LP was performed because of reoccurring abducens nerve palsy and persisting papilledema and headache demonstrating a pressure of 27 and 29 cm H2O, respectively, thus confirming true PTC.
Among the pubertal children with PTC complex (n = 21; 14 girls, seven boys), the most common clinical symptom was headache (n = 15). One patient (no. 35) had a 4-month history of chronic daily headache. However, initially papilledema was not found. After this 4-month period, papilledema became evident. LP confirmed PTC complex. Four children complained of nausea or vomiting. Five patients were asymptomatic. Papilledema was found in all but one patient. The mean CSF opening pressure in this group was 30 cm H2O (range 19–65 cm H2O). One female adolescent was considered as “probable PTC” (no. 38) as she showed prompt clinical response to pressure release and acetazolamide (ACT) with normalization of papilledema.
Obesity was found in four patients; five were classified as overweight. Among those with normal weight, there were four oncological patients under chemotherapy. Five patients were found to be anemic (Hb < 12 g/l) at time of PTC complex diagnosis. Further comorbidities are listed in Table 2.
Therapy and outcome
All patients underwent acute pressure release during an initial LP. After LP, five patients suffered from moderate to severe post-LP headache syndrome. One patient (no. 35) was bedridden for 2 weeks because of severe orthostatic headache and vertigo. In all other patients, acceptance of LP was good.
Follow-up at our institution ranged from no follow-up to 5 years (mean 19 months). One patient (no. 27) was only seen once, and no details about the further clinical outcome are available. Patient no. 34 was lost for follow-up after 2 weeks. One patient (no. 48) died during the course of bone marrow transplantation, and long-term response to treatment cannot be judged.
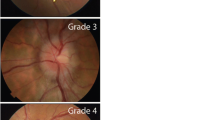
Oral ACT was the drug of first choice (target dose 25–30 mg/kg/day; maximum dose 1.5–2 g/day). Mean duration of medical treatment was 7 months (range 4–14 months). In 34 of those 50 patients (68%) who were followed for at least 4 months, this therapy led to complete and persistent resolution of papilledema and clinical symptoms. ACT was tapered thereafter. Patient no. 40 showed rapid normalization of the optic disk after cessation of growth hormone treatment in addition to ACT. Patient no. 4 did not respond to medical treatment and showed only very short-lasting improvement after LP. Therefore, CT angiography was performed, demonstrating a cerebral sinus venous thrombosis (see Fig. 1). Due to massive papilledema, reduced consciousness, and abducens nerve palsy, this patient underwent ventricular–peritoneal (VP) shunting, which led to complete remission.
Ophthalmologic and radiological findings of patient 4 (see Table 1): a right-sided abducens nerve palsy, b fundoscopy of the right and left eye, showing apparent swelling of the optic disc, and c CT angiography: lateral angiographic view showing normal dural sinuses and bridging veins. An enlarged ophthalmic vein is ostentatious indicating abnormal venous outflow. The white arrow marks the rostral part of the cavernous sinus drain via the ophthalmic vein (black arrow)
Two patients (nos. 8 and 12) showed good response to treatment as defined by persistent normalization of CSF pressure and cessation of clinical symptoms. However, in absence of any visual failure, mild to moderate papilledema was still present during a follow-up period of up to 27 months. Patient no. 50 developed chronic, persistent papilledema, which was most likely caused by drug nonadherence.
Two patients were considered as nonresponder to medical treatment (nos. 2 and 3). Both developed progressive papilledema despite treatment with ACT, furosemide (1 mg/kg/day), and prednisone (2 mg/kg/day for 2 weeks). Medication nonadherence was suspected in one patient with a difficult social situation (no. 2). In patient no. 3, serial LPs were performed which resulted in complete resolution of papilledema after 12 months time and five LPs. In patient no. 2, this approach was declined by the parents. This boy finally underwent ventricular–peritoneal shunting, which was done without complication. Ophthalmologic follow-up in both children showed a permanent reduction of optic disc swelling.
In ten out of 50 patients (20%), a relapse of PTC complex (six prepubertal and four pubertal patients) was seen. Seven patients were still under ACT treatment at that time. In all children but one (no. 35), ACT was restarted as therapy. Two of these experienced a second relapse after cessation of treatment. Again, ACT was reintroduced, and up to now, all of these patients remained symptom-free. Patient no. 35 was set on topiramate and experienced a second relapse while still under this medication. She remained relapse-free after a second LP with pressure release and a prolonged episode of post-LP headache syndrome.
Patient no. 50 experienced one relapse after 12 months of ACT. Later on, he developed chronic, persistent papilledema due to drug nonadherence.
In addition, one boy with probable PTC (no. 9) showed an immediate clinical response after the first pressure release; however, 4 months later, he experienced a relapse. Although CSF opening pressure was only 20 cm H2O, we decided to set him on ACT, which led to complete remission.
Altogether, there was no obvious association between relapse and the initial CSF opening pressure, age, sex, BMI, or Hb.
Discussion
Epidemiology
Although the design of our study is not sufficient to provide solid epidemiological data, our analysis demonstrates that PTC complex is not such a rare condition in a tertiary pediatric center. In agreement with previous studies and unlike in adulthood, we did not find any female preponderance or association with obesity in prepubertal children [9, 10]. On the contrary, overweight was frequently seen in pubertal patients. Importantly, in 43% of our patients, putative associated conditions were identified, which may appear unexpectedly high in a pediatric population. Certainly, the large proportion of cancer patients in our series has contributed to this high percentage [2]. However, beside obesity, additional associated factors have been found in our nononcological study population, which will be discussed below.
Clinical presentation
The spectrum of clinical presentation at time of diagnosis of PTC complex was broad ranging from asymptomatic papilledema to dramatic clinical presentations such as bilateral abducens palsy in an infant with reduced consciousness (no. 4).
Headache was the most frequent clinical symptom in older children and adolescents, which is in good agreement with previous studies [9]. Patients mostly reported chronic daily headache or acute onset headache, often mimicking migraine. Against this background, confusion with idiopathic headache might be a problem, and therefore, repeated evaluation for papilledema may be recommended in children with chronic daily headache. However, an important aspect of our study is the variability or even absence of papilledema in some affected patients (nos. 1, 9, and 23). Especially in very young children, this feature may be inconstant. Furthermore, there have been reports of adults with PTC in whom papilledema has not been observed. Absence of papilledema is thus not an exclusionary criterion [11]. Equally important, as observed in one patient (no. 35) with chronic daily headache, papilledema may only develop later during the clinical course of PTC complex. Therefore, a single ophthalmological examination is not necessarily conclusive and does not exclude PTC complex.
Blurred vision and abducens palsy were other relatively common features in our patient groups as well as in others [12]. No further cranial nerve palsies were found.
An important finding of our study was the high number of asymptomatic patients. Sixteen patients with PTC complex had no clinical symptoms, and papilledema was found only on routine eye examination. This is in contrast to most previous studies. One study [12] found all patients with prepubertal PTC symptomatic. Lim et al. [13] described only three out of 29 children as asymptomatic. However, more recently, asymptomatic pediatric PTC cases have been repeatedly published [14, 15]. Notably, among our asymptomatic patients, there were the five youngest children who may not have been able to articulate their complaints. This raises questions regarding the incidence of undetected cases in this age group.
Diagnostic difficulties
We have identified several diagnostic difficulties in our children with suspected PTC complex. Firstly, conduction of LP under deep sedation was sometimes necessary. However, drugs used for sedation may induce changes of the ICP. Inhalation anesthetic agents [16] and ketamine [17] have been shown to raise ICP. Therefore, we recommended the use of propofol. However, this drug has been reported to possibly lower ICP [18]. In addition, the physiological effect of hypercarbia on ICP has been recognized in intensive care and anesthesia [19]. Accordingly, CSF pressure values recorded under sedation have to be judged critically [20].
Beside technical problems, diagnostic criteria in the pediatric age group are not completely satisfactory as it is illustrated by our patients with “probable PTC”, a term only recently proposed by our group [6]. Two of these patients showed marked fluctuations of the CSF opening pressure when measured repeatedly even within a short time. While the initial pressure would have been considered normal, on repeated LP, a CSF opening pressure above 20 cm H2O was measured. This stresses the possibility of missed cases of PTC due to diurnal fluctuations of CSF opening pressure [21, 22]. The lack of age-adapted normal values for CSF opening pressure constitutes another diagnostic dilemma. In some children, clinical presentation was highly suggestive of PTC, but CSF opening pressure was measured below 20 cm H2O. However, since a clear response to pressure release and/or ACT could be documented in these cases, we would now consider a therapeutic trial in any of such cases in order to prevent permanent visual disturbances [6].
Etiology
In a considerable number of our patients, possibly associated factors that may have contributed to elevated intracranial pressure could be identified. Certainly, PTC complex may be present in a broad spectrum of hemato-oncological diseases [2]. Growth hormone treatment, probably playing a causal role in one of our patients, has repeatedly described as a secondary cause of PTC [23]. In addition, one child had sinus venous thrombosis. This important cause of secondary PTC has been found to account for 9.4% of nonpediatric patients with presumed PTC [24]. This underlines the importance of MR venography in any atypical case of PTC, including all prepubertal children.
Further comorbidities or medications, the causal role of which often remains uncertain, were found. Associated factors were l-thyroxine therapy in children with hypothyroidism, anemia, and different kinds of infection.
PTC following thyroxine replacement therapy in juvenile hypothyroidism has been described previously. Rapid correction of hypothyroidism with thyroxine may be a risk factor for altered CSF dynamics [23].
Fourteen patients were found to be moderately anemic (Hb < 12 g/l) at time of PTC complex diagnosis. This may be an important observation in the context of PTC. Different types of anemia have been associated with PTC complex [25], and it has been suggested that disturbed hemodynamics may lead to a secondary increased intracranial pressure [23]. Although differentiation of causality from coincidence may often be difficult, a check for anemia should be routine in all PTC complex patients as it may represent a treatable risk factor for relapse (patient no. 2) [23]. The number of infections in relation to PTC complex (nos. 4, 25, 29, 35, and 36) needs to be discussed in the context of our recent observation of a seasonal cluster of prepubertal PTC presentations during the typical season of pediatric viral and bacterial infections [4].
In summary, although causality is often not easy to proof in PTC complex cases, our findings give some support to the view of Friedman and Jacobson [26] who stated that a secondary cause for intracranial hypertension should be suspected in any “atypical” patient, including any prepubertal patient and any male and/or nonobese adolescent. We believe that classification as idiopathic or secondary PTC, at least in part, depends on the efforts made to identify associations that may have contributed to elevated intracranial pressure and may therefore often be arbitrary. This view is supported by recent studies, which found association of intracranial hypertension with underlying illnesses in up to 77.7% of pediatric patients with “idiopathic” PTC [10, 27].
Therapy
Some important conclusions may be drawn from our findings regarding therapy of pediatric PTC complex. First of all, we generally state a high responder rate to initial pressure release followed by ACT treatment in our population, irrespective of age, sex, or underlying etiology. During our follow-up, no patient suffered from permanent visual disturbances (with the exception of patient 50, who refused therapy). Second-line agents were only needed in three patients (nos. 2, 3, and 35). However, it is noteworthy that none of them benefited from additional furosemide, topiramate, and/or corticosteroids. Although these drugs are part of most current guidelines of management of PTC, our limited experience may point to a minor role in children not responding to high-dose ACT therapy.
In order to prevent more invasive procedures, we recommend repeated LP in nonresponsive patients. This particularly holds true when severe visual impairment or severe therapy-resistant headache is present. Unlike others [23], we still believe that serial LP is a feasible treatment option. As shown in one patient (no. 3), this may even prevent neurosurgery. Discomfort can be usually sufficiently reduced by sedation. Although it has been stated that CSF pressure may return to pretap values within hours [28], some patients may only require a single LP with pressure release to achieve complete remission (no. 34). A limiting factor for serial LP may be post-LP headache syndrome, which was seen in five of our patients. This is important to note for two reasons: (1) symptoms of lowered intracranial pressure may be misinterpreted as persistent PTC (no. 35) [29] and (2) prolonged post-LP discomfort may limit the option of serial LP thus leading to surgical approaches.
Importantly, shunt requirement was exceptional in our cohort. Unlike in previous studies, which reported the necessity of shunt therapy in up to 68% of children with PTC [30, 31], only two out of 53 patients underwent VP shunting. We believe that surgery should be reserved for patients with a particularly severe clinical course of the disease or those resistant to medication and not responding to or not tolerating repeated LP (e.g., no. 2).
Follow-up
An essential and possibly underappreciated part of PTC management is a thorough clinical follow-up. This was not standardized in our cohort before the year 2004. While some children were followed up to 6 years, others were lost already after initiation of drug therapy. In that view, it has to be considered that many of our patients were followed by primary care ophthalmologist or family doctors. Having in mind the rarity of childhood PTC complex, it is likely that some physicians will not be familiar with pediatric PTC cases. To our experience, documentation of papilledema and visual fields is often not standardized. While we have recently started to use the Frisen scale to follow papilledema [32] in addition to photo documentation, both of these are still exceptional in primary care. Moreover, assessment of visual fields, which may be the most reliable way to monitor visual function of PTC patients [12], is often not performed, and if done, interpretation can be very difficult even in experienced hands.
The importance of a standardized follow-up is highlighted by the relatively high rate of relapses (20%) in our study. Relapses occurred up to 3 years after initial presentation. This rate is higher than described in previous studies in the pediatric population [33] but is in accordance with observations of Kesler et al. [34] who found a nearly 40% relapse rate in their cohort of patients aged 14–45 years. In their study, all exacerbations occurred later than 10 months after initial presentation, indicating that late relapses are a significant risk. Importantly and unlike in their study, we found that relapses may even occur while patients were still on full-dose ACT treatment at time of relapse. Therefore, long-term monitoring of papilledema and visual status is necessary. Notably, relapses are not always indicated by recurrence of clinical symptoms (e.g., no.16).
Close monitoring in the hands of experienced pediatric ophthalmologists and pediatric neurologists may also help to improve drug adherence, another problem revealed by our study (nos. 2 and 50). One of our adolescent patients (no. 50) was reluctant to take any medication for PTC treatment. PTC complex finally resulted in persistent optical atrophy. This case reminds us that adolescents, in particular, have difficulties adhering to medication regimens in chronic diseases which can easily lead to an unfavorable outcome [35]. In keeping with this suggestion, a recent retrospective study identified puberty as a risk factor for unfavorable visual outcome in PTC [36]. This indicates that the possible role of drug adherence as a contributor to these results deserves further attention.
Conclusion
PTC complex constitutes an important and possibly underrecognized disorder in children and adolescents. Considering the high percentage of possibly associated conditions in our study, a detailed diagnostic work-up is crucial to identify treatable underlying conditions. Importantly, children may not always completely meet Dandy’s modified criteria as demonstrated by our patients with probable PTC. Since the feared consequence of PTC complex is visual loss, early diagnosis, treatment, and close follow-up are of great importance. According to our experience, initial pressure release via LP and treatment with ACT is usually effective and tolerated well. However, standardized long-term follow-up schemes are essential in order to detect cases of recurrence, even in the absence of clinical symptoms. Finally, our experience underlines the need for further clinical studies in order to better standardize diagnosis and management of PTC complex in children.
References
Ball AK, Clarke CE (2006) Idiopathic intracranial hypertension. Lancet Neurol 5:433–442
Distelmaier F, Gobel U, Vandemeulebroecke N, Mayatepek E, Rosenbaum T, Laws HJ (2007) Secondary pseudotumor cerebri in pediatric oncology and hematology: an unpredictable condition of varying etiology. Pediatric Blood Cancer 49:1029–1033
Quincke H (1897) Ueber Meningitis serosa und verwande Zustande. Dtsch Z Nervenheil 9:140–168
Distelmaier F, Tibussek D, Schneider DT, Mayatepek E (2007) Seasonal variation and atypical presentation of idiopathic intracranial hypertension in pre-pubertal children. Cephalalgia 27:1261–1264
Distelmaier F, Sengler U, Messing-Juenger M, Assmann B, Mayatepek E, Rosenbaum T (2006) Pseudotumor cerebri as an important differential diagnosis of papilledema in children. Brain Dev 28:190–195
Distelmaier F, Mayatepek E, Tibussek D (2008) Probable idiopathic intracranial hypertension in pre-pubertal children. Arch Dis Child 93:356–357
Kromeyer-Hauschild K, Wabitsch M, Kunze D (2001) Perzentile für den Body Mass Index für Kinder im Alter von 0 bis 18 Jahren. Monatszeitschrift Kinderheilkunde 149:807–818
Lewis DW (2002) Headaches in children and adolescents. Am Fam Physician 65:625–632
Babikian P, Corbett J, Bell W (1994) Idiopathic intracranial hypertension in children: the Iowa experience. J Child Neurol 9:144–149
Scott IU, Siatkowski RM, Eneyni M, Brodsky MC, Lam BL (1997) Idiopathic intracranial hypertension in children and adolescents. Am J Ophthalmol 124:253–255
Wraige E, Chandler C, Pohl KR (2002) Idiopathic intracranial hypertension: is papilloedema inevitable? Arch Dis Child 87:223–224
Cinciripini GS, Donahue S, Borchert MS (1999) Idiopathic intracranial hypertension in prepubertal paediatric patients: characteristics, treatment, and outcome. Am J Ophthalmol 127:178–182
Lim M, Kurian M, Penn A, Calver D, Lin JP (2005) Visual failure without headache in idiopathic intracranial hypertension. Arch Dis Child 90:206–210
Weig SG (2002) Asymptomatic idiopathic intracranial hypertension in young children. J Child Neurol 17:239–241
Bassan H, Berkner L, Stolovitch C, Kesler A (2008) Asymptomatic idiopathic intracranial hypertension in children. Acta Neurol Scand 118:251–255
Talke P, Caldwell JE, Richardson CA (1999) Sevoflurane increases lumbar cerebrospinal fluid pressure in normocapnic patients undergoing transsphenoidal hypophysectomy. Anesthesiology 91:127–130
Ben Yehuda Y, Watemberg N (2006) Ketamine increases opening cerebrospinal pressure in children undergoing lumbar puncture. J Child Neurol 21:441–443
Engelhard K, Werner C (2006) Inhalational or intravenous anesthetics for craniotomies? Pro inhalational. Curr Opin Anaesthesiol 19:504–508
Gallagher A, Pike M, Berg S (2004) Beware CSF pressure measured under general anaesthesia. Arch Dis Child 89:691
Mishra A, Mordekar SR, Rennie IG, Baxter PS (2007) False diagnosis of papilloedema and idiopathic intracranial hypertension. Eur J Paediatr Neurol 11:39–42
Johnston I, Paterson A (1974) Benign intracranial hypertension. II. CSF pressure and circulation. Brain 97:301–312
Gucer G, Viernstein LJ (1978) Long-term intracranial pressure recording in the management of pseudotumor cerebri. J Neurosurg 49:256–263
Rangwala LM, Liu GT (2007) Pediatric idiopathic intracranial hypertension. Surv Ophthalmol 52:597–617
Lin A, Foroozan R, Danesh-Meyer HV, De Salvo G, Savino PJ, Sergott RC (2006) Occurrence of cerebral venous sinus thrombosis in patients with presumed idiopathic intracranial hypertension. Ophthalmology 113:2281–2284
Biousse V, Rucker JC, Vignal C, Crassard I, Katz BJ, Newman NJ (2003) Anemia and papilledema. Am J Ophthalmol 135:437–446
Friedman DI, Jacobson DM (2002) Diagnostic criteria for idiopathic intracranial hypertension. Neurology 59:1492–1495
Youroukos S, Psychou F, Fryssiras S, Paikos P, Nicolaidou P (2000) Idiopathic intracranial hypertension in children. J Child Neurol 15:453–457
Soler D, Cox T, Bullock P, Calver DM, Robinson RO (1998) Diagnosis and management of benign intracranial hypertension. Arch Dis Child 78:89–94
Loh Y, Labutta RJ, Urban ES (2004) Idiopathic intracranial hypertension and postlumbar puncture headache. Headache 44:170–173
Orssaud C, Dureau P, Zerah M, Cinalli G, Sainte Rose C, Kahn AP, Dufier JL (2001) Benign childhood intracranial hypertension. J Fr Ophtalmol 24:54–59
Weiss B, Collmann H, Schropp C (2007) Idiopathic intracranial hypertension—a review over 16 cases in childhood. Presented at the Annual German Neuropediatrics Meeting, Passau, Germany, 22–25 March 2007
Frisén L (1982) Swelling of the optic nerve head: a staging scheme. J Neurol Neurosurg Psychiatry 45:13–18
Ng YT, Bodensteiner JB (2003) Idiopathic intracranial hypertension in the pediatric population. J Child Neurol 18:440
Kesler A, Hadayer A, Goldhammer Y, Almog Y, Korczyn AD (2004) Idiopathic intracranial hypertension: risk of recurrences. Neurology 63:1737–1739
Winnick S, Lucas DO, Hartman AL, Toll D (2005) How do you improve compliance? Pediatrics 115:e718–e724
Stiebel-Kalish H, Kalish Y, Lusky M, Gaton DD, Ehrlich R, Shuper A (2006) Puberty as a risk factor for less favorable visual outcome in idiopathic intracranial hypertension. Am J Ophthalmol 142:279–283
Disclosure
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tibussek, D., Schneider, D.T., Vandemeulebroecke, N. et al. Clinical spectrum of the pseudotumor cerebri complex in children. Childs Nerv Syst 26, 313–321 (2010). https://doi.org/10.1007/s00381-009-1018-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-009-1018-0