Abstract
Introduction
Penetrating injuries of the gravid uterus are rare complications of pregnancy with gunshot wounds most common than stab wounds. Fetal head injury is an unusual sequela of these penetrating traumas.
Materials and methods
We describe the case of a 20-year-old pregnant woman stabbed at the lower abdomen at 30th weeks of gestation. She was nonsurgically managed by serial examination and continuous fetal monitoring.
Results
Spontaneous vaginal delivery occurred at term with good maternal and fetal outcome. The newborn examination revealed a right temporal swelling interpreted as a subcutaneus hemangioma. At 2 years and 6 months of life, the child was led to our attention with a pulsating bulge in the right temporal region. Clinical examination and imaging were indicative of a typical growing skull fracture. The child underwent neurosurgical procedure for repairing of the dural tear and bone defect according to the senior author's personal technique, described in details, with a good neurological and esthetic outcome.
Conclusion
Thirty-two cases of stab wounds to the pregnant uterus have been reported to date in medical literature with two cases of fetal head injury.Growing skull fractures are rare complications of head injury and only one case has been described in the perinatal period following blunt trauma to the mother's abdomen 2–3 weeks before birth.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Penetrating abdominal trauma is an uncommon complication during pregnancy, with gunshot wounds much more common than stab wound [1]. Although it is rare for a maternal death to occur from uterine injury since the uterus is not a vital organ and may be, after the first trimester, protective of other abdominal contents, the fetal death rate in both gunshot and stab injuries is appreciable: 71% and 42%, respectively [2, 3]. Intrauterine penetrating fetal head injury following gunshot wound has been reported and the outcome is usually lethal, depending upon the severity of the intracranial insult and the gestational period of the mother [4–8]. The fetus, if it survives, is at high risk of developing encephalopathy, cerebral palsy, and long term cognitive and developmental delay [9]. At our best knowledge, intrauterine penetrating direct fetal head trauma due to stab wounds has been described in literature two times only [10, 11].
We present here a case of fetal head-penetrating injury following a stab wound to the mother's abdomen during the 30th week of gestation resulting in a growing skull fracture. A complete review of the medical literature regarding stab wounds to the pregnant uterus has been done.
Case history
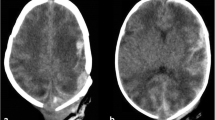
A 2.5-year-old child, adopted from Colombia, with a previous, referred, diagnosis of subcutaneous hemangioma, was led to our attention by pediatricians. He presented with a pulsating bulge in the right temporal region. Neurological examination disclosed, in addition, a mild left hemiparesis. A computed tomographic (CT) scan, including bone windows and 3D reconstruction, revealed a large right temporal bone defect (Figs. 1 and 2). Magnetic resonance imaging (MRI) showed herniation of the cicatricial cerebral tissue through the skull defect and a mild “blow out” of the homolateral temporal ventricular horn (Figs. 3, 4 and 5). Neuropsichological evaluation and EEG were within normal limits.
As clinical examination and imaging were indicative of a typical growing skull fracture (GSF) and no history of head trauma was known to the adoptive parents, we asked the Colombian institution, where the child was born, more information about pregnancy and birth.
According to the Colombian institution's medical records, pregnancy was complicated, during the 30th week of gestation, by a knife stab wound in the lower abdomen, that the mother, a 20-year-old woman, received from her partner with the intention to harm the unborn child.
The woman was managed nonsurgically by serial examinations and continuous fetal monitoring. Spontaneous vaginal delivery occurred at 40th week of gestation, with good maternal and fetal outcome.
The newborn examination revealed a right temporal swelling that was interpreted as a subcutaneous hemangioma. This diagnosis was confirmed when the child was adopted in Italy.
At our institution, the child underwent neurosurgical procedure for repairing of the dural tear and bone defect. In the operating room, while positioning the patient, a very thin scar was noted on the bulging skin on the right temporal region (Figs. 6 and 7).
Skin incision was designed to allow for complete access to the edges of the dura mater that, as they usually happens, were retracted for some distance back from the bone edges that were involved with intense and white cerebro-meningeal scarring (Fig. 8). After a careful dissection of these adhesions, bone was removed piecemeal from the edges of the cranial defect until the dural edge was identified. Hence, we made a watertight duroplasty with deproteinized equine pericardium affixing fibrin glue on dural boundaries (Fig. 9). Cranioplasty was finally performed using hydroxyapatite granules mixed with autologous blood between two meshs of absorbable material, in a sandwich fashion (Figs. 10 and 11). Follow-up skull X-rays 1 year after surgery showed a good regrowth of the skull to fill the bony defect (Fig. 12). Neurological examination was within limits.
Discussion
The incidence of trauma occurring during pregnancy has been reported to be about 6% to 7% and increasing [12, 13]. Most pregnancy injuries are due to blunt trauma as the result of motor vehicle accidents, accidental falls, and violence. In this case, the most common cause of fetal death is maternal death [14] although direct injury to the fetus in the absence of uterine injury has been reported [15]. The occurrence of fetal skull's fracture following blunt trauma to the mother's abdomen is the most common fracture encountered [12, 16] and is well described in the literature, starting from the end of the 19th century [17–19].
Alexander and Davis in 1969 provided an exhaustive review of older and recent reports on intrauterine depression fractures of the skull in infants [20]. When the position of the fetal head was documented, they found that the depressed fracture occurred as the result of the contact of the skull against the promontory of the sacrum in all except one of the cases reported in their series, as previously supposed by others [17–19].
Less frequent than blunt trauma, penetrating wounds of the abdomen during pregnancy are usually manifestations of gunshot and stab wounds. Other causes are extremely rare. They have higher risk of injury both to the maternal viscera and the fetus [21]. Bullet wounds are the most common type of penetrating injuries during pregnancy [3]. Stab wounds have a better maternal prognosis due to the absence of shock waves, the ability of visceral organs to slide away from the advancing knife blade, and the protective shield of the uterus.
The maternal death rate from gunshot wounds to the abdomen is reported to be two thirds less than in nonpregnant victims (3.9% vs 12.5%). The death rate from abdominal stab wounds is also diminished by the so-called protective effects of the uterus.
A detailed review of the literature disclosed 32 cases of stab wounds of the uterus in pregnancy, 33 if we consider our case (Table 1). Guadagnini reported the first case of stab wound of the gravid uterus in 1930 [22]. Several authors reported isolated cases [2, 10, 11, 23–29]. The typical patient stabbed in pregnancy is between 18 and 28 years of age. She is usually in the early or late part of the third trimester (26 out of 30 cases). All of the patients who were stabbed in the abdomen had uterine wounds varying from 2 to 5 cm in length. The angle of penetration and the length of the knife have a direct correlation to the depth of the inflicted injury. A stab wound of the gravid uterus with proper intervention has a good prognosis for the mother (only one died, but she received about 25 knife injuries in her head, neck, thorax, and extremities in addition to the abdomen) [29]. However the fetus suffers. Twenty-four out of the 33 fetus survived (72.7%). Seventeen out of 33 patients had vaginal delivery with 76.4% fetal survival [Table 1].
Only two fetus, excluding our case, suffered head injury following intrauterine knife stab [10, 11]. Grubb reports a case of a 26 year-old Hispanic woman, at 30 weeks of gestation in her first pregnancy, brought to the hospital with multiple stab wounds to the abdomen and upper extremities inflicted by her husband with a steak knife. On the admission, the patient was hemodynamically stable and the fetal heart rate was 140 beats/min. Obstetric ultrasonography revealed a single fetus in a breech presentation, with an estimated fetal weight of 1,928 gm, and no evidence of fetal injury. The fetal head was directly below one of the wounds. There was a normal amniotic fluid volume, and the placenta was anterior with no evidence of retroplacental blood clot. Continuous fetal heart rate monitoring, serial hematocrit determinations, and serial abdominal examinations were undertaken. The patient was then observed in the hospital for an additional 48 h. No signs of infection developed, and she was discharged from the hospital. At 34 weeks of gestation, she was admitted to the hospital in labor. On rupture of the membranes, the fluid was noted to be dark brown with particulate matter present. A vigorous female infant weighing 2,540 gm with Apgar scores of 8 at 1 min and 8 at 5 min was delivered spontaneously. The uterus was explored manually and was intact. A poorly healed laceration, about 5 mm long, was noted over the infant's left parietal bone and closed spontaneously on the second day of life.
Schulz et al. describe a case of a 19-year-old woman in her 29th week of pregnancy who was stabbed in the lower abdomen during a robbery. Two hours later, an emergency cesarean delivery was performed. Blood was present in the amniotic fluid. The Apgar scores were 2/5/6 at 1.5 and 10 min, respectively. Above the right ear was a 2-cm-long bleeding wound. The neonate had stable respiratory and hemodynamic functions. The cerebral sonogram showed an extensive intracerebral hemorrhage in the region of the right thalamus and temporal lobe with a visible 5 to 6-cm long incision channel stretching about 1 cm beyond the midline. A large, right-sided subdural hematoma near the laceration site and intraventricular bleeding had occurred. Surgical evacuation of a subdural hematoma was undertaken. The child developed a left spastic hemiparesis.
Evaluation of the pregnant patient with either gunshot or stab wounds of the abdomen must take into consideration the physiologic changes of pregnancy while following the principles of trauma management. A patient with a gunshot wound generally requires surgical exploration, although Awwad et al. advocate conservative management in anterior abdominal entry wounds below the level of the uterine fundus [30]. Otherwise, a patient with a stab wound to the abdomen may require exploratory laparotomy only if there is evidence of intraperitoneal hemorrhage or bowel perforation. Cesarean section may be required if fetal distress ensues [31].
GSF are reported to complicate less than 1% of all skull fractures. Most cases of GSF described in the literature have occurred in children under 3 years of age, one half occur in children under 1 year of age [32]. The first report of this condition was in 1816 by John Howship who noted “partial absorption of the (right) parietal bone, arising from a blow on the head” in a child aged 9 months [33].
GSFs require a head injury severe enough to include a skull fracture, a tear in the dura mater, and brain injury. The outward driving force, such as a normally growing brain, is the mechanism underlying the formation of the growing fracture. These elements explain why the vast majority of growing fractures occur in very young children and also the very occasional report of this entity in the adult age [34–36]. As with all skull fracture, the most common location for the development of a GSF is the parietal bone, although it can occur anywhere, including in the skull base [36, 37].
Only one case of intrauterine growing skull fracture has been described in medical literature by Moss et al. in 1990 in a full-term male infant with a mother's history of a blow to the abdomen 2 or 3 weeks before birth. Abdominal ultrasound at 36 weeks of gestation did not demonstrate intracranial lesions. The newborn examination revealed a right parietal caput succedaneum and cephalohematoma. Neurosurgical consultation at 2 weeks of age revealed a linear lesion measuring 3 cm × 7 cm in the parietal bone. In this case, surgery was performed at 4 weeks of age. The typical features of a GSF were encountered [38]. In our case, it appears that the strength of the stab wound was not capable of a deep brain injury such as the case reported by Schultz et al., but only of a bony interruption and a dural tear with parenchymal injury. From this, a GSF has slowly developed. We think it is unlikely, in view of the injury noted at delivery, that earlier delivery would have improved the outcome of the infant.
Conclusion
To our knowledge, this is the first reported case of intrauterine head injury following a stab wound of the gravid uterus, resulting in a GSF. Our intraoperative findings are totally in concordance with the pathogenetic mechanism formulated for this condition by Lende and Erickson in 1960 [32]. The goals of the operation for GSF are to completely identify all the dural defects, free the adhesions, decompress the cyst, provide a watertight dural closure, and fill the bony defect with a cranioplasty. This unusual case supports literature's recommendations that injuries known to penetrate the uterus may be managed with the fetus left in utero if there is no evidence of fetal distress or amniotitis, and that exploratory laparotomy can be deferred if there is no evidence of maternal or fetal hemorrhage or bowel injury.
References
Buchsbaum HJ (1979) Penetrating injury of the abdomen. In: Buchsbaum HJ (ed) Trauma in pregnancy. WB Saunders, Philadelphia, p 82
Sakala EP, Kort DD (1988) Management of stab wounds to the pregnant uterus. A case report and review of the literature. Obstet Gynecol Surv 43:319–324
Sandy EA, Koerner M (1988) Self-inflicted gunshot wound to the pregnant abdomen: report of a case and review of the literature. Am J Perinatol 43:319–324
Browns K, Bhat R, Jonasson O, Vidyasagar D (1977) Thoraco-abdominal gunshot wound with survival of a 36-week fetus. JAMA 237:2409–2410
Edner G, Erasmie U, Gentz J, Lundell B, Schiller B (1988) Intrauterine cranial gunshot wound in a 32 week fetus. J Trauma 28:1605–1606
Franger AL, Buchsbaum HJ, Peaceman AM (1989) Abdominal gunshot wounds in pregnancy. Am J Obstet Gynecol 160:1124–1128
Iliya FA, Hajj SN, Buchsbaum HJ (1980) Gunshot wounds of the pregnant uterus: report of two cases. J Trauma 20:90–92
Weissman MN, Green BA, Morse B (1984) In-utero gunshot wound to the head. Use of intraoperative ultrasonography for localization of an intracerebral projectile. Surg Neurol 21:347–350
Muzumdar D, Higgins MJ, Ventureyra ECG (2006) Intrauterine penetrating direct fetal head trauma following gunshot injury. A case report and review of the literature. Child's Nerv Syst 22:398–402
Schultz H, Bretschneider S, Lamme W, Minda R, Canzler E (1993) Intrauterine stab injury with a knife in the head of a fetus in the 29th week of pregnancy. Kinderarztl Prax 61:215–218 (article in German)
Grubb DK (1992) Nonsurgical management of penetrating uterine trauma in pregnancy: a case report. Am J Obstet Gynecol 166(2):583–584
Baker DP (1982) Trauma in the pregnant patient. Surg Clin North Am 62(2):275–289
Esposito TJ (1994) Trauma during pregnancy. Emerg Med Clin North am 12(1):167–199 Review
Crosby WM, Costiloe JP (1971) Safety of lap-belt restraint for pregnant victims of automobile collisions. N Engl J Med 284:632–636
Hartl R, Ko K (1996) In utero skull fracture: case report. J Trauma 41:549–552
Rothenberger D, Quattlebaum FW, Perry JF Jr, Zabel J, Fischer RP (1978) Blunt maternal trauma: a review of 103 cases. J Trauma 18(3):173–179
Brinton JH (1884) Report of two cases of intrauterine fracture, with remarks on this condition. Trans Am Surg Assoc 2:425–443
Lunney G (1886) Case report. Accident to a pregnant woman, resulting in fracture of the skull of the fetus. Med Rec NY 29:359–360
Smith RR (1913) Intrauterine fracture: report of a case and review of the literature. Surg Gynecol Obstet 17:346–356
Alexander E, David CH (1969) Intrauterine fracture of the infant skull. J Neurosurg 30:446–454
Buchsbaum HJ (1968) Accidental injury complicating pregnancy. Am J Obstet Gynecol 102:752
Guadagnini A (1930) Laceration of the anterior wall of the uterus and hernation of placenta. Rev Med Latino-Am 15:1029
Degefu S, O’Quinn AG, Pernoll ML, James W (1988) Stab wound of the gravid uterus: a case report and literature update. J La State Med Soc 140(10):39–41
Raginia R (1966) A case of delivery after a stab wound of the abdomen in pregnancy with concomitant injury of the fetus. Ginekol Pol 37(11):1239–1242 (article in Polish)
Mukaramov AM, Mukaramova MU (1987) Knife wound of the abdomen with uterine and fetal injuries in a pregnant woman. Klin Khir. (2):58 (article in Russian)
Shapkin VV, Mel'nikov AV (1988) Intrauterine penetrating knife wound of the chest. Klin Khir. (6):74 (article in Russian)
Belousov AF, Romanova GN (1977) Penetrating abdominal injury with damage to the pregnant uterus and intrauterine injury to the fetus. Vestn Khir Im I I Grek 119(7):126–127 (article in Russian)
Fleming AN, Quarmby C, Hudson Don A (2001) Intrauterine stab leading to a radial nerve palsy. Ann Plast Surg 47:562–564
Yildirim C, Goksu S, Kocoglu H, Gocmen A, Akdogan M, Nurullah G (2004) Perimortem cesarean delivery following severe maternal penetrating injury. Yonsei Med J 45(3):561–563
Awwad JT, Azar GB, Seoud MA (1994) High-velocity penetrating wounds of the gravid uterus: review of 16 years of civil war. Obstet Gynecol 83:259–264
Lavin JP, Polsky SS (1983) Abdominal trauma during pregnancy. Clin Perinatol 10(2):423–438
Lende RA, Erickson TC (1961) Growing skull fracture of childhood. J Neurosurg 18:479–489
Howship J (1816) Practical observations in surgery and morbid anatomy. Longman, London, p 494
Halliday AC, Chapman PH, Heros RC (1990) Leptomeningeal cyst resulting from adulthood trauma. Case report. Neurosurgery 26:150–153
Rahman NV, Abedeen B, Tanjoom ZA, Tanjoom HB, Murshid WR (1994) Growing skull fractures. Classification and management. Br J Neurosurg 8:667–679
Gupta SK, Reddy NM, Khosla VK, Mathuriya SN, Shama BS, Pathak A, Tewari MK, Kak VK (1997) Growing skull fractures: a clinical study of 41 Patients. Acta Neurochir (Wien) 139:928–932
Byrne JV, Britten JA, Kaar G (1992) Chronic post-traumatic erosion of the skull base. Neuroradiology 34:526–531
Moss SD, Walker ML, Ostergard S, Golembeski D (1990) Intrauterine growing skull fracture. Child's Nerv Syst 6:468–470
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gallo, P., Mazza, C. & Sala, F. Intrauterine head stab wound injury resulting in a growing skull fracture: a case report and literature review. Childs Nerv Syst 26, 377–384 (2010). https://doi.org/10.1007/s00381-009-0969-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-009-0969-5