Abstract
Objectives
Craniopharyngioma during childhood poses difficulty in management because of the high incidence of surgical complications and treatment failure. In order to identify less detrimental and more effective treatment, a personal series of craniopharyngioma was reviewed in regard to various clinical factors, patient factors (age and sex), tumor factors (location and extension, relationship with chiasm, and hydrocephalus), and therapeutic modes [extent of resection and radiation therapy (RT)].
Materials and methods
Fifty-four childhood craniopharyngiomas treated from 1984 to 2003 were reviewed. Preoperative neuroimaging studies were classified depending upon tumor location and extension. In this series of 54 patients, 43 had total tumor resection and 11 had subtotal resection. Of the total resection group, ten showed evidence of residual tumor on postoperative neuroimaging studies. Following the initial resection, 46 did not have RT whereas 8 with subtotal resection received RT.
Results
There were no surgical deaths. Postoperative complications included pseudoaneurysm in 1, hemiparesis in 3, severe obesity in 5, panhypopituitarism in 50, and worsening of visual function in 7. During follow-up ranging from 12 months to 21 years, 24 patients had recurrence. Of the 33 patients with radiographic total resection, 9 (27.3%) had recurrence. Among the patients with total resection but radiographic residual and those with subtotal resection, the craniopharyngioma recurred in 90% and 100%, respectively. Three (37.5%) of eight patients with subtotal resection with RT had recurrence. Overall recurrence-free survival was 62% at 5 years and 49% at 10 years. The sex and age, location and extension of the tumor, nature of the optic chiasm, and hydrocephalus did not influence survival with statistical significance. However, the extent of surgical resection and use of RT showed significant differences for survival. Patients with total resection had a recurrence-free survival rate of 83% and 70% at 5 and 10 years, respectively. Patients with subtotal resection with RT had 71% at 5 years and 36% at 10 years. Patients who had subtotal resection or radiographically residual tumor without RT had a recurrence-free survival rate of only 9%. Among 22 patients whose recurrent tumor was treated with RT, a second recurrence-free survival rate was 90% at 5 years.
Conclusion
Total resection provided the best outcome. However, recurrence rates and surgical complications remained high following radical tumor resection. RT was effective for recurrent tumors and should be considered being the primary treatment for recurrences or difficult tumors, which are not amenable to total resections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Craniopharyngioma is one of the most representative tumors in childhood and often occurs during childhood. According to the Central Brain Tumor Registry of the United States, craniopharyngioma affects 0.13 per 100,000 children per year, with a peak at 5–9 years where annual incidence is 0.20 per 100,000 children [2]. Treatment of childhood craniopharyngioma poses an ongoing controversy as to the most effective and least detrimental therapy. Currently accepted therapies for it are either radical tumor resection or limited resection followed by radiation therapy (RT). Clearly, surgical extirpation is the ideal goal to attain the chance of cure because of this histologically benign nature. However, the craniopharyngioma’s location in or adjacent to the hypothalamus–pituitary axis, optic pathway, the circle of Willis, and the third ventricle hinders safe resection. In spite of improved diagnostic methods, microsurgical techniques, and hormonal replacement therapies, total resection is a formidable experience even to the experienced neurosurgeons. Even at attempt of total resection, the literature indicates that total surgical resection was possible at most in 70% to 90% of the children [3]. Surgical complications such as visual disturbances, neuroendocrine dysfunction, hypothalamic obesity, psychological disorder, and neurovascular trauma have been well recognized following radical tumor resection. Despite surgical total resection, some patients experience recurrence. In order to avoid these complications and recurrences, some strongly advocated that these children should be treated with limited resection followed by RT or intracavitary therapy with radioisotope or chemotherapeutic agents. However, the efficacy of these conservative treatments and their long-term side effects remain undetermined. In this communication, the author’s personal series of childhood craniopharyngiomas were reviewed and analyzed for their presentations, surgical approaches, adjuvant therapy, and outcome.
Materials and methods
From 1984 to 2003, 54 children with craniopharyngiomas were diagnosed and treated at Children’s Memorial Hospital. All available information was collected through medical records, and pertinent neuroimaging tests were reviewed personally. This retrospective study was approved by the Internal Review Board of Children’s Memorial Hospital.
Clinical information constituted sex, age at diagnosis, and presenting symptoms including neurological, ophthalmologic, and endocrine dysfunctions. Neuroimaging including computed tomography (CT) and magnetic resonance imaging (MRI) were reviewed in order to identify the characters such as calcifications, cyst formations, coexisting hydrocephalus, and location and extension of the tumor and cyst(s).
Operative notes were reviewed to identify surgical approaches and extent of tumor resection. Postoperative complications were identified through medical records. Adjuvant therapies, particularly RT, were identified and recorded.
All patients had surveillance studies of a combination of CT and MRI. Following immediate postoperative imaging, they were obtained every 3 months during the first year, every 4 months during the second year, and every 6 months for the subsequent three years. After 5 years, annual surveillance neuroimaging were obtained up to 10 years. Follow-up evaluations were completed in all patients. Time of recurrence and treatments of recurrences were recorded when occurred. Kaplan–Meyer survival analysis was conducted in order to identify factors influencing patient survivals using STATISTICA (Tulsa, OK).
Results
Patient population
There were 28 males and 26 females. The age at diagnosis ranged from 11 months to 16 years, with median average of 8.2 years. Figure 1 shows the distribution of ages at diagnosis with a peak at 6–8 years and another peak at 14–16 years.
Presenting symptoms
Presenting symptoms are shown in Table 1, which indicates headaches and visual changes as the most common. Visual function at diagnosis showed that 31 patients were normal whereas 23 had abnormal vision. Of the latter, 13 had decreased visual acuity (10 monocular, 11 biocular) and two had visual field defects. Endocrine dysfunction was noted in 22 patients: short statute in ten, inappropriate secretion of antidiuretic hormone in three, diabetes insipidus in three, delayed puberty in three, precocious puberty in two, and Cushing’s disease in one.
Nature and classification of craniopharyngioma
All patients had head CT and 45 had MRI. Calcifications were noted in 52 and cyst formation in 50. Solid craniopharyngiomas were noted in four patients. Based upon the neuroimaging and surgical findings, four types of craniopharyngiomas were identified according to location and extension of tumor and cyst(s). They were classified into (1) third ventricle without sella, (2) third ventricle with sella, (3) sella with suprasella, and (4) intrasella type. The third ventricle without sella type showed that the primary tumor location was mostly within the third ventricle. They had a small sella turcica, and the pituitary gland was depressed at the sella floor (Fig. 2a). Strictly, third ventricle location was rare, but the tumor or cyst often extended into the posterior fossa (Fig. 2b,c). The third ventricle with sella type showed tumor and/or cyst(s) extending from the sella turcica to the third ventricle cavity (Fig. 3a). The cyst(s) may extend to subfrontal or posterior fossa location (Fig. 3b). Once the tumor was removed, there was a defect in the floor of the third ventricle (Fig. 4a,b). The sella with suprasella type had tumor extending from the sella turcica to the suprasella location. In this type, the sella turcica was often enlarged and the tumor displaced the third ventricle floor upward (Fig. 5a,b). The cyst(s) extended anteriorly to the subfrontal location, posteriorly to the posterior fossa, or laterally to the middle cranial fossa (Fig. 5c). Following tumor resection, most of the third ventricle floor was preserved in this type (Fig. 6a–d). The intrasella type showed the tumor primarily present in the sella turcica. There were 9 (16.7%) third ventricle without sella types, 22 (40.7%) third ventricle with sella types, 20 (37%) with sella with suprasella types, and 3 (5%) intrasella types.
Midsagittal MR images before (a) and after (b) resection of craniopharyngioma of sella with suprasella type. Midsagittal MR images before (c) and after (d) of giant craniopharyngioma of sella with suprasella type in another patient. Note preserved floor of the third ventricle following tumor resection in both patient
Hydrocephalus
Hydrocephalus due to obstruction of the third ventricle was present in 27 (50%) patients. Seven patients had ventriculoperitoneal shunts placed: six early in this series and another at outlying hospital before transfer. Other 20 patients had intraoperative ventriculostomy, which was converted postoperative external ventricular drainage. Twelve patients had cyst drainage done by stereotaxy in two and endoscopy in ten. The cyst drainage was done a few weeks prior to tumor resection in six with the Ommaya reservoir placement. All these six had resolution of hydrocephalus. The remaining six patients had endoscopic cyst drainage at EVD placement during tumor surgery. All these 12 patients had successful cyst drainage. In another patient, an attempt of cyst drainage by endoscope was unsuccessful due to a firm capsule. Two of the precraniotomy shunt were removed, and hydrocephalus in all others resolved following tumor resection.
Tumor resection
All patients had surgical resection of craniopharyngioma. Surgical total resection was intended in all except for three patients. The last three who had craniopharyngioma with third ventricle without sella had an intentional subtotal resection and received planned postoperative RT.
Surgical approaches used included craniotomy in 51 patients and transsphenoidal approach in 3 (all with intrasella type). Of craniotomies, the most common was unilateral frontotemporal craniotomy with a combined subfrontal/pterional approach in 44. Two had a bifrontal craniotomy for tumors with large cysts extending to the bifrontal location. Two patients had a posterior frontal craniotomy, and tumor resection was done through the interhemispheric transcallosal approach. The remaining three patients had a staged resection of tumor, first using the interhemispheric transcallosal approach, and then through a subfrontal/pterional approach.
Through the subfrontal/pterional approach, craniotomy was made at its inferior border as close as possible to the superior orbital edge. A few patients had the orbital edge removed together with the craniotomy flap in order to attain a better angle to look into the third ventricle [34]. The suprasellar cistern was reached along the sphenoidal wing and the cistern was opened with cerebrospinal fluid (CSF) drainage, which led to the brain relaxation. The proximal Sylvian fissure was also opened to allow wider exposure of the suprasella cistern. At the inspection of the chiasm in 51 patients, it was noted that 36 were postfixed chiasm whereas 15 were prefixed. All of the craniopharyngiomas with the third ventricle without sella type had prefixed chiasm. Preoperative midsagittal magnetic resonance (MR) was useful to predict postfixed vs prefixed chiasm based upon the location of the anterior cerebral artery and optic chiasm; they are elevated in the former (Fig. 7a) and depressed in the latter (Fig. 7b). For the case of postfixed chiasm, the primary resection was through the prechiasmal space and the space between the optic nerve and internal carotid artery (opticocarotid space). In the case of prefixed chiasm, the primary rout was through the lamina terminalis and the opticocarotid space. Tumor resection consisted of cyst drainage, internal debulking, and removal of the cyst capsule. The cyst from the third ventricle was decompressed in recent cases by transventricular endoscopic drainage. Following cyst decompression, the dome of the cyst was brought downward because craniopharyngiomas of this type originate invariably in the tuber cinereum. Following the cyst decompression and internal decompression, the prechiasmal and opticocarotid space became wider.
The carotid arteries and optic nerves and chiasm did not adhere to the tumor capsule. The basilar artery and brainstem also did not directly adhere to the tumor. These structures became identifiable through the opticocarotid space or the third ventricle following tumor resection. The floor of the third ventricle was displaced and the craniopharyngioma directly extended into the third ventricle. However, at the anterior inferior third ventricle, the capsule tended to be adherent in various degrees to the ventricular wall (hypothalamus). Identification and preservation of the pituitary stalk was attempted but often unsuccessful as the pituitary stalk was often involved by the tumor. In the case of deep sella, it was difficult to visualize and remove the anterior inferior portion of the tumor via the subfrontal/pterional approach. A dental mirror was helpful to identify residual tumor deep in the sella turcica. In three cases, the planum sphenoidale was drilled and the sphenoid sinus was entered. The tuberculum sellae and the anterior wall of the sella turcica were removed by rongeur, and the dura of the sella was opened in order to remove this portion of the tumor.
At the interhemispheric transcallosal approach, the enlarged foramen of Monro was entered, and the cyst was drained and removed from the third ventricle. The tumor capsule was only adherent to the inferior wall of the third ventricle and was sharply dissected from it under direct vision. Anteriorly, the optic chiasm was identified and carefully protected. Difficulty was encountered when accessing the undersurface of the chiasm through this approach.
Extent of tumor resection and adjuvant therapy
Surgical total resection was attained in 43 patients (79.6%). Out of these 43 patients, total resection was confirmed in 33 (76.7%) by postoperative CT and MRI, whereas 10 (23.3%) showed small radiographic residual tumor or calcifications: six on the floor of the sella turcica, two in the third ventricle, one in the prepontine space, and one in the frontal lobe. In the remaining 11 patients, subtotal resection (20.4%) was performed and noted by postoperative imaging: eight in the third ventricle, one in the hypothalamus, one in the temporal lobe, and one in the sella turcica.
Table 2 shows the correlation of extent of tumor resection with the location and extension of tumor. Of nine patients, craniopharyngioma of the third ventricle without sella type had total resection in only three, one of which had radiographic evidence of residual. Nineteen of 22 craniopharyngioma of the third ventricle with sella type and 18 of 20 craniopharyngioma of the sella with suprasella type had surgical total resection, whereas four of the former and five of the latter had radiographic residual tumors. All the intrasella tumors had total resection.
Following the initial resection, 46 did not have adjuvant therapy. Eight, who had subtotal resection, received RT.
Surgical complications
Neurological complications
Intraoperative complication occurred in one patient. This 5-year-old boy had a third ventricular craniopharyngioma (Fig. 8), which had endoscopic cyst drainage and subsequent tumor resection through the lamina terminalis. During the resection, abrupt arterial hemorrhage occurred from deep in the third ventricle during the retraction of the tumor capsule. The hemorrhage was controlled by packing the partially resected tumor cavity with hemostatic agents. Postoperative CT showed intraventricular and subarachnoid hemorrhages, and CT angiography showed a pseudoaneurysm at the posterior cerebral artery (Fig. 9a,b). The patient made uneventful recovery, and the pseudoaneurysm reduced in size spontaneously over 9 months.
Three patients had postoperative hemiparesis. One was due to postoperative hemorrhage into the tumor-resected cavity, and others were due to infarct of the perforating artery in the distribution of the basal ganglia in one and of the cerebral peduncle in another.
Three patients had transient short-term memory loss. One patient had transient oculomotor nerve palsy, in which the third nerve was intimately adherent to the tumor capsule.
One of the three patients who had a subfrontal transsphenoidal approach developed CSF rhinorrhea postoperatively, which was then treated using transnasal packing of the sphenoid sinus.
Endocrine complications
Postoperative panhypopituitarism occurred in 50 (92.6%) requiring multiple hormonal replacement therapy. Diabetes insipidus occurred in 50 patients, 3 of which were transient. Of the 47 patients with permanent diabetes insipidus, 39 developed within 48 h of surgery, and 8 developed from 5 to 60 postoperative days. Hypothalamic obesity was noted in 15 patients (27.8%), of which 5 had severe obesity with insulin-resistant diabetes.
Visual complications
Postoperative visual evaluations showed normal in 33 patients. Ten patients had monoocular visual dysfunction, and four had biocular visual dysfunction. Five showed temporal or homonymous hemianopia. Two had monoocular visual dysfunction with contralateral hemianopia. When compared with pre- and postoperative visual functions, 36 patients did not show changes, 11 showed improvement, and 7 showed worsening.
Recurrences
During the time of follow-up ranging from 12 months to 21 years, 24 had tumor recurrence. Of the 33 patients who had radiographic total resection, 9 (27.3%) had recurrence, whereas 9 (90%) of the 10 who had surgical total resection but radiographic evidence of residual tumor had recurrence. Of the 11 patient with subtotal resection, all 3 patients who did not have RT and 3 of 8 with postoperative RT had recurrence.
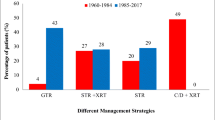
Overall recurrence-free survival was 62% at 5 years and 49% at 10 years (Fig. 10). The recurrence-free survivals were correlated with patient’s sex, age at diagnosis, nature of the chiasm, tumor extension, hydrocephalus, and extent of tumor resection. There were no statistical differences between male and female, though female had better survival than male (Fig. 11). According to the age groups, the patients diagnosed at 4–7 years had a worse survival rate than other age groups, though there were no statistical differences (Fig. 12). There was no statistical difference between groups with postfixed and prefixed chiasm (Fig. 13). Patients with craniopharyngiomas extending to or localized in the third ventricle seemed to have poorer recurrence-free survival than craniopharyngioma located in the sella or suprasellar region, but there was no statistical difference (Fig. 14). The patients with hydrocephalus showed poorer recurrence-free survival than those without hydrocephalus, as the former had high propensity of third ventricle involvement (Fig. 15). The extent of tumor resection influenced the recurrence-free survival (Fig. 16). Patients with total resection had recurrence-free survival rate of 83% and 70% at 5 and 10 years, respectively. Patients with subtotal resection with RT had 71% at 5 years and 36% at 10 years. Patients who had subtotal resection or radiographically residual tumor without RT had a recurrence-free survival rate of only 9%.
Recurrence-free survival of childhood craniopharyngioma comparing types of tumor location. Patients with craniopharyngiomas extending to or localized in the third ventricle seemed to have poorer recurrence-free survival than craniopharyngioma located in the sella or suprasellar region, but there was no statistical difference (p=0.66244)
Recurrence-free survival of childhood craniopharyngioma by extent of tumor resection and adjuvant RT. Patients with total resection had recurrence-free survival rate of 83% and 70% at 5 and 10 years, respectively. Patients with subtotal resection with RT had 71% at 5 years, and 36% at 10 years. Patients who had subtotal resection without RT had a recurrence-free survival rate of only 9% at 5 years. There was a statistical significance (p=0.00000)
Of the 24 patients with recurrence, 14 patients had reoperation: 12 with subtotal resection followed by RT, and 2 with total resection only for recurrent tumors. The remaining 10 patients with small recurrence less than 1 cm3 had RT without tumor resection. One of the patients with recurrent tumor had a severe adhesion to the internal carotid artery and had hemorrhage from it during the resection. Figure 17 shows recurrence-free survival following RT for recurrent craniopharyngioma with or without surgical resection in 22 patients. A second recurrence of craniopharyngiomas was noted in only two patients, and a 5-year second recurrence-free survival rate following RT for recurrent craniopharyngioma was 90%. Figure 18 shows overall recurrence-free survival following RT for primary or recurrent craniopharyngioma: the recurrence-free survival rates at 5 and 10 years were 90% and 70%, respectively.
Case mortality
Four patients died; two patients died of tumor progression, 3.5 and 8.5 years, respectively. One patient died of addisonian crisis without tumor recurrence 4 years and 3 months postoperatively, which occurred in the earlier stage of this study. Another patient died of acute viral hepatitis 2 months postoperatively during RT. Figure 19 shows overall survival: 93% at 5 years and 90% at 10 years.
Discussion
Craniopharyngiomas have been classified based upon location and extension as they influence the surgical approach and difficulty in tumor removal. Hoffman classified them as sellar, prechiasmatic, postchiasmatic, and giant types [11]. The sellar craniopharyngiomas are limited to the sella turcica with no or little suprasellar extension. The prechiasmal type shows a growth forward into the prechiasmal space displacing the chiasm posteriorly and elevating the A1 segment upward. The postchiasmal tumor pushes the chiasm anteriorly against the tuberculum sellae, and the direction of the growth is toward the third ventricle and often present with obstructive hydrocephalus. Steno et al. [31] classified supradiaphragmatic craniopharyngiomas into suprasellar extraventricular, intraventricular/extraventricular, and intraventricular dependent upon the relationship with the third ventricle. They noted intraventricular/extraventricular type as far more common (14/18 cases) in children, whereas the incidence of suprasellar extraventricular and extraventricular/intraventricular types are about equal in adults. True intraventricular craniopharyngioma with an intact floor of the third ventricle is exceedingly rare.
In the present series, the classifications of craniopharyngiomas are made based upon third ventricle and sella turcica involvement. The third ventricle without sella type in this series invariably showed association with prefixed chiasm, and all presented with hydrocephalus. They had a small sella turcica, and the pituitary gland is well preserved on MRI. They often extend into the interpeduncular cistern and the posterior fossa. Although true intraventricular craniopharyngiomas with intact sella floor were reported [22], it is difficult to conclude even based upon MR and surgical observation in most cases as to the presence of intact ependymal layer at the floor. Craniopharyngiomas of the third ventricle with sella type, which consisted of 40.7% of the cases in this series, had prefixed chiasm in six cases. Craniopharyngiomas of sella with suprasella type had elevation of third ventricle floor with elevation of the A1 segment of the anterior cerebral artery, and only two had a prefixed chiasm. The origin of the tumor would dictate the direction of the growth, which would dictate the nature of optic chiasm [34]. Wang et al. [38] postulated that the tumor origin above or below the diaphragma sellae dictates the direction of the tumor growth.
Surgical resection of childhood craniopharyngioma remains a great challenge in most of cases. Involvement of the optic pathway, hypothalamus, third ventricle, and the circle of Willis often hinder the surgeon’s ability to attain total resection. Various approaches have been practiced to achieve the goal of total resection. However, each approach has its own advantage and disadvantage.
When using the skull base approach, a slack brain is mandatory. Brain relaxation is achieved by intraoperative release of the CSF either by ventriculostomy or opening the suprasellar cistern. Endoscopic drainage of the cyst from the third ventricle facilitates brain relaxation and also allows less manipulation of the third ventricle at tumor resection. One may use mannitol to attain the brain relaxation, but it often creates difficulty in fluid management and detection of diabetes incipidus (DI) during and following surgery. Hydrocephalus associated with childhood craniopharyngioma is due to obstruction at the third ventricle, thus, it is relieved following successful reduction of the mass in the third ventricle. Use of a ventriculoperitoneal shunt should be avoided as it may lead to an upward shift of the tumor under the optic chiasm, causing acute visual changes [34]. Use of endoscopic cyst drainage prior to surgery eliminates hydrocephalus or improves vision when it is rapidly deteriorating. Placement of an Ommaya reservoir using the endoscopic approach provides for future treatment options while awaiting definitive treatment. Endoscopic drainage failed in only 1 of 12 patients in this series due to a firm tumor capsule. Pierre-Kahn et al. [24] described similar findings where 3 of 16 cystic craniopharyngiomas in children were impossible to perforate due to a thick capsule.
One should access the shortest distance to the parasellar structures as well as attain their greatest surgical view. The optic nerve, chiasm, and carotid arteries are often separated from the tumor capsule. Also, the basilar artery is separated from the tumor capsule by the arachnoid membrane. However, these structures are manipulated during tumor resection and demand meticulous care and techniques during dissection. It is particularly concerning at resecting a recurrent craniopharyngioma as these structures tend to adhere to the tumor capsule. At the floor of the third ventricle, the tuber cinereum is often displaced and attached by the tumor. The portion affecting the tuber cinereum is ideally resected using sharp dissection under direct vision. The optic chiasm and hypothalamus does not have definable anatomical boarders, and craniopharyngiomas of this location need to be separated away from the posterior edge of the chiasm.
In this series, most of the craniopharyngiomas were resected using a combined unilateral subfrontal and pterional approach, exploring available spaces such as prechiasmal, translamina terminalis, opticocarotid, and carotid-tentorial. A wide opening of the proximal Sylvian fissure is helpful to enlarge the suprasella view and causes less stress on the frontal lobe upon retraction. The pterional approach along the sphenoid ridge provides the shortest distance to the suprasellar location; however, it is difficult to visualize the contralateral optic nerve and carotid artery. A subfrontal approach, though it provides good visualization of the optic nerve, chiasm, and carotid system, makes it difficult to visualize the undersurface of the ipsilateral optic nerve. The combined subfrontal/pterional approach via frontotemporal craniotomy overcomes these disadvantages. For the postfixed chiasmal case, the contralateral optic nerve and carotid artery are often well visualized once the prechiasmal tumor is removed. However, the ipsilateral optic nerve or optic tract needs to be displaced to remove the tumor underneath of them, which may cause postoperative unilateral visual disturbances such as monocular or homonymous hemianopia. Also, another limitation of this approach is the portion of the tumor located in the anterior inferior portion of the deep sella turcica. The tumor extending to the third ventricle gradually retracted out of the third ventricle. At this time, the tumor capsule needs to be secured to maintain its continuity. If the capsule is broken off and the remnant is lost in the third ventricle, it is difficult to retrieve. This portion of the tumor needs to be removed through a translamina terminalis approach, though it is difficult to perform in cases of severely postfixed chiasm [34]. The subfrontal transsphenoidal approach through the planum sphenoidale and anterior wall of sella turcica [23] provides access to the sella turcica. One of the three patients in this series who had this procedure had CSF rhinorrhea.
In third ventricle craniopharyngiomas, when the prechiasmal space is not available due to prefixed chiasm, the tumor is not visualized through a subfrontal approach even when transecting the optic nerve at postmortem examination (Fig. 20). In such cases, the primary route for tumor resection is through the lamina terminalis [17] (Fig. 21). In this series, all cases with prefixed chiasm had tumor resected from the third ventricle using the translamina terminalis approach. There were no complications regarding the opening of the lamina terminalis. A wider opening between the chiasm and anterior commissure provides for good visualization of the third ventricle. However, one should take extra caution to avoid traumatizing the anterior cerebral artery and anterior communicating artery, as they tend to traverse over the lamina terminalis. The disadvantage of the pure translamina terminalis approach is that the tumor at the undersurface of the chiasm is hard to reach. This portion needs to be removed through the opticocarotid space or widening the prechiasmal space by drilling the tuberculum sellae [23].
Unfixed postmortem photographs of third ventricle craniopharyngioma. Due to a prefixed chiasm, tumor was not visualized though a subfrontal approach even when the bilateral optic nerves were transected at autopsy (a). A view of the base of the brain showing a third ventricle craniopharyngioma (b). There was a lack of normal floor of the third ventricle, and the tumor was directly exposed to the suprasellar cistern. The proximal portion of the pituitary stalk was surrounded by the craniopharyngioma. Midsagittal section of the brain showing a cystic craniopharyngioma in the third ventricle behind the chiasm (c)
The bifrontal approach provides better anatomical orientation of the optic pathway and the anterior circle of Willis over the unilateral approach. Removal of the orbital rims provides improved vision of the suprasellar location and the third ventricle. The concerns when using the bifrontal approach are frontal lobe trauma from forcible retraction and bilateral olfactory nerve traction and severance. The olfactory nerves should be carefully dissected and protected during frontal lobe elevation. When using the frontobasal interhemispheric approach, transaction of the anterior falx lessens frontal lobe and olfactory damage [29, 30]. However, this approach, the portion of craniopharyngioma extending laterally, may be difficult to reach.
The interhemispheric transcallosal approach through the enlarged foramen of Monro caused by hydrocephalus provides the easiest access to the dome of the craniopharyngioma within the third ventricle (Fig. 22). This approach is suitable for a third ventricle craniopharyngioma as it does not manipulate the optic pathway or carotid artery. By perforating the septum pellucidum, access to the third ventricle is possible through the bilateral foramen of Monro (Fig. 23a–c). The craniopharyngioma capsule, which is severely attached to the inferior wall of the third ventricle, is detached by sharp dissection under direct vision. The disadvantage of this approach is that it needs an enlarged ventricle and may potentially damage the fornix during manipulation. Also, the portion of the tumor undersurface of the chiasm is hard to access.
Intraoperative photographs of third ventricle craniopharyngioma resected through transcallosal approach. Through the open septum pellucidum, bilateral foramina of Monro were inspected (a). Note a craniopharyngioma cyst in the third ventricle. Following the resection of the third ventricle craniopharyngioma, the posterior floor of the third ventricle was free from the tumor (b). An arrowhead indicating the aqueduct of Sylvius. At the anterior third ventricle, the optic chiasm (arrowhead) anteriorly and the basilar artery and brain stem through the membrane of Liliquist (arrow) posteriorly were visualized (c)
The transnasal transsphenoidal approach used in three patients of this series attained total resection without causing additional visual or endocrinological complications. Although transsphenoidal resection of craniopharyngiomas has been limited to those of subdiaphragmatic tumor type, some advocate this approach for those extending beyond the diaphragma sellae [1, 13, 16, 18]. However, the pediatric population, small nasal structure, and less pneumatized sphenoid sinus may limit adequate exposure of the sella turcica lesion. Also, there is a concern of traumatizing the normal pituitary gland, which is often displaced ventrally at transsphenoidal resection of the craniopharyngioma. Dumbbell-shaped craniopharyngiomas extending to the suprasellar location are often difficult or hazardous to remove completely. By the experienced hand, however, craniopharyngiomas with a large suprasellar extension are removed with minimum morbidity. Maira et al. [18] recommended widening the opening of the sella floor by removing bone from it, the tuberculum sellae, and the posterior part of the planum sphenoidale. This facilitates the prediaphragmatic view. In their series, total resection was attained in 63% of the cases. However, the incidence of CSF rhinorrhea poses a problem and occurs in 19% to 33% of their cases. Abe and Ludecke [1] attained a total resection in 3 of 11 children with transsphenoidal approach, and 8 with subtotal resection. In the latter, the residual tumor capsule was coagulated. They stated that in the pediatric population, subtotal resection is justified in order to avoid hypothalamic damage and excessive CSF leakage.
Preservation of the pituitary stalk needs to be attempted in all cases; however, they are difficult to identify due to their displacement or total encasement by the tumor (Fig. 22). The pituitary stalk shows a reddish, longitudinal striated appearance due to the portal vessels. Pituitary stalk preservation was attained in 64% of Shibuya et al.’s [29] cases, but nearly all developed postoperative diabetes insipidus, though they required a lower dose of anterior pituitary hormone replacement. Yasargi et al. [39] preserved the pituitary stalk in only 32% of their cases, though they could identify the stalk in 56.3% of the cases. Van Effenterre and Boch [35] reported that the stalk was preserved in 52% of their cases.
In the literature, rates of successful total resection vary. Most authors reported the rates ranging from 24 to 70% for childhood craniopharyngiomas [35, 37].
Yasargi et al. [39] reported 90% total resection rates among adult and pediatric populations using multimodal approaches.
Postoperative complications are related to the manipulations of respective anatomical structures. Radical tumor resections often cause panhypopituitarism, needing hormone replacement therapy. The most affected hormone was growth hormone, which occurs in nearly all patients despite treatment modality [7]. Although the preservation of the pituitary gland and stalk provides better pituitary function postoperatively, it does not necessarily guarantee postoperative pituitary function. It is worth preserving the pituitary stalk, but if it hinders total resection, we prefer to remove the stalk. Hormone deficits appeared to be less common among patients following less aggressive surgery with RT or transsphenoidal resection.
One of the major goals of surgery for craniopharyngioma is to preserve or improve visual function of the child. Patients with progressive visual deterioration often improve following surgical decompression; however, although less, a significant number of patients experience visual deterioration following craniopharyngioma resection [24, 34, 39]. Most of the visual deterioration occurs in the ipsilateral side from the surgical approach, due to manipulating the optic nerve or optic tract upon resecting the tumor under these structures or approaching the opticocarotid space. Pierre-Kahn et al. [24] suggested decompression of the cyst and waiting for visual function to return or become stable before tumor resection, as postoperative visual deterioration is more frequent when visual compromise is profound.
Vascular complications related to surgical resection are relatively uncommon. Arterial spasmus due to manipulation of the carotid artery or major branches are often observed. It can be treated by application of topical papaverine. Small perforating artery trauma causing hemiplegia postoperatively may be unrecognized during the tumor resection as occurred in three patients of this series. The most devastating vascular complication is intraoperative rupture of the major artery as occurred in one patient in this series. De Vile et al. [4] reported a high incidence of arterial or venous hemorrhage intraoperatively in their 63 patients; carotid bifurcation hemorrhage in nine, damage of the middle cerebral artery in one, significant spasmus of carotid artery in two, and profuse venous hemorrhage in six. Sutton reported late fusiform aneurysm formation in the carotid artery, which was assumed due to damage of the adventitia [33]. The fusiform aneurysms developed between 6 and 9 years after surgery, and none hemorrhaged.
Signs of postoperative hypothalamic damage, particularly development of serious obesity and disturbances of memory and behavior, are relatively common [3, 5, 12, 21]. Because of the intimate attachment of the craniopharyngioma to the ventromedial nucleus, surgical manipulation creates hyperphagia. According to the literature, hypothalamic obesity occurred in more than half of the patients [4, 25], of which 15% was severe [5]. According to the German Multicenter Study, 44% of 185 children with craniopharyngioma developed severe obesity, lowering their quality of life [21]. Carpentieri et al. [3] reported, based on 16 children following total or subtotal resection without RT, that significant memory disturbances, particularly difficulty in the retrieval of learned information, was noted following surgical resection despite well-preserved full scale intelligence quota (IQ). On the other hand, Merchant et al. [19] compared full-scale IQ between groups with surgery alone and limited surgery and RT. They noted that the former groups lost a mean of 9.8 points in full-scale IQ, whereas the latter lost only 1.25 points.
The extent of tumor resection influences recurrence rates in childhood craniopharyngiomas [4, 35]. Despite total resection, craniopharyngiomas often recur. Recurrence rates after total resection range from 10 to 53% in the reported series [12, 24, 35, 40]. De Vile et al. [4] reported that recurrence-free survival rates at 5 and 10 years after complete resection in children were 89% and 78%, respectively. In a series combining pediatric and adult craniopharyngiomas, Van Effenterre and Boch [35] reported they were 95% and 75%, respectively. However, Kim et al. [14] reported a much lower recurrence-free survival rate of 55% at 5 years. Recurrences usually occur within 3 years of radical tumor resection. One of the recurrences in this series occurred 13 years after surgery. Microscopic residual cells isolated from the main tumor in the surrounding gliotic tissue were considered the source of recurrence after what appeared to be total resection [20]. Residual calcifications noted on the postoperative CT is highly suspicious for residual tumor, and these patients need close follow-up [34]. Residual craniopharyngiomas prelude future recurrences. Following subtotal resection without RT, the recurrence rates were 80–100%, though one report showed only 33% recurrence rate after subtotal resection [35].
Growing bodies of publications are available to support radio responsiveness of craniopharyngiomas. It is commonly accepted to provide RT for the patient with incompletely resected craniopharyngioma. The literature indicates variable response rates to RT in children. Hetelekidis et al. [10] reported that the 10-year progression-free survival for surgery-alone group was 31% compared with 100% for children with RT only and 86% for children with surgery plus RT. Rajan et al. [27] reported the 10- and 20-year progression-free survival rates following RT with or without surgery in 173 patients, 45% of which were children, were 83% and 79%. Stripp et al. [32] reported that the 10-year local control rate of craniopharyngioma was 42% after surgery alone and 84% after subtotal resection followed by RT. Others reported that children with radical resection alone showed a recurrence rate of 17.6%, whereas those with limited resection with RT had a recurrence rate of 42.8% [37]. Two cohorts, one with total resection and the other with subtotal resection and RT, showed comparable results [4]. In our series, a similar finding was noted for 5-year recurrence-free survival, 83% and 71%, respectively. RT for recurrent craniopharyngiomas showed excellent tumor control in this series; of the 22 patients with recurrent craniopharyngioma with or without surgical resection, the 5- and 10-year recurrence-free rates were 90% and 80%, respectively. Van Effenterre and Boch [35] demonstrated a similar result in which only 1 patient of 16 who had RT for recurrent tumor had a second recurrence.
On the other hand, early recurrence was noted even during or shortly after RT. Enlargement of solid component or cyst expansion, however, does not necessarily represent tumor progression. These regrowths are temporary and start to reduce in size over time. However, they need watchful observations [4, 9, 28].
However, a majority of reports concerning RT for craniopharyngiomas show no serious side effects referable to irradiation to the sellar location. Particularly, advances in radiation oncology technique utilize more focused irradiation to the tumor avoiding surrounding structures using image-guided conformal irradiation, fractionated stereotactic radiosurgery, intensity modulated RT, gamma knife radiosurgery, or proton beam therapy. Also, intracavitary beta-irradiation for cystic craniopharyngioma has been used. Despite these advanced techniques, two concerns remain when irradiating the pediatric brain of children: they are optic neuropathy [6, 36] and secondary tumor growth or malignant transformation [8, 15].
Although growth hormone replacement therapy is widely used, the concern that it provokes recurrence of the craniopharyngioma remains. However, a large study in 488 patients with craniopharyngioma showed that growth hormone therapy did not show a significant increase in the rate of recurrences [26].
Conclusion
Even after total surgical resection, craniopharyngiomas recur in a significant percent of the patients, approximately 30% in this series. When there is evidence of residual tumor on postoperative neuroimaging studies, their recurrence is invariably unavoidable. Complications associated with aggressive surgical resection in endocrinological, ophthalmological, and neurological functions are substantial. However, certain groups of craniopharyngiomas, particularly those with a readily accessible location in the sella or suprasellar location, and with a smaller size tumor, are resectable with minimum morbidity. It should be noted that the size of the mass of large cystic craniopharyngiomas is significantly reduced by drainage of the cyst using endoscopic procedures.
The effectiveness of RT for craniopharyngioma for tumor control is undeniable. The tumor control with RT for primary and recurrent craniopharyngiomas is comparable with that after total resection without RT: 70% recurrence-free survival rate at 10 years for both. Although the side effects of RT must be scrutinized, one should cautiously evaluate the pros and cons of each treatment: radical tumor resection vs limited resection with RT.
Searching for safe and effective therapy for childhood craniopharyngiomas continues, and multicenter trials need to be done. Meanwhile, each patient should be evaluated individually for a definitive treatment plan.
References
Abe T, Ludecke DK (1999) Transnasal surgery for infradiaphragmatic craniopharyngiomas in pediatric patients. Neurosurgery 44:957–966
CBTRUS (2004) Statistical report: primary brain tumors in the United States, 1997–2001. Central Brain Tumor Registry of the United States, Chicago, IL
Carpentieri SC, Waber DP, Scott RM, Goumnerova LC, Kieran MW, Cohen LE, Kim F (2001) Memory deficits among children with craniopharyngiomas. Neurosurgery 49:1053–1057
De Vile CJ, Grant DB, Kendal BE, Neville BGR, Stanhope R, Watkins KE, Hayward RD (1996) Management of childhood craniopharyngioma: can the morbidity of radical surgery be predicted? J Neurosurg 85:73–81
Poretti A, Grotzer MA, Ribi K, Schonle E, Boltshauser E (2004) Outcome of craniopharyngioma in children: long-term complications and quality of life. Dev Med Child Neurol 46:220–229
Flickinger JC, Lunsford LD, Singer J, Cano ER, Deutsch M (1990) Megavoltage external beam irradiation of craniopharyngiomas: analysis of tumor control and morbidity. Int J Radiat Oncol Biol Phys 19:117–122
Gonc EN, Yordam N, Ozon A, Alikasifoglu A, Kandemir N (2004) Endocrinological options in children with craniopharyngioma: a retrospective analysis of 66 cases. Pediatr Neurosurg 40:112–119
Habrand JL, Gantry O, Couanet D, Rouxel V, Levy-Piedbois C, Pierre-Kahn A, Kalifa C (1999) The role of radiation therapy in the management of craniopharyngioma: a 25-year experience and review of the literature. Int J Radiat Oncol Biol Phys 44:255–263
Hamamoto Y, Niino K, Adachi M, Hosoya T (2002) MR and CT findings of craniopharyngioma during and after radiation therapy. Neuroradiology 44:118–122
Hetelekidis S, Barnes PD, Tao ML, Fischer EG, Schneider L, Scott RM, Tarbell NJ (1993) 20-year experience in childhood craniopharyngioma. Int J Radiat Oncol Biol Phys 27:471–475
Hoffman HJ (1994) Surgical management of craniopharyngioma. Pediatr Neurosurg 21(Suppl 1):44–49
Hoffman HJ, De Silva M, Humphreys RP, Drake JM, Smith ML, Blaser SI (1992) Aggressive surgical management of craniopharyngiomas in children. J Neurosurg 76:47–52
Im SH, Wang KC, Kim SK, Chung YN, Kim HS, Lee CH, Cho BK (2003) Transsphenoidal microsurgery for pediatric craniopharyngioma: special considerations regarding indications and method. Pediatr Neurosurg 39:97–103
Kim SK, Wang KC, Shin SH, Choe G, Chi JG, Cho BK (2001) Radical resection of pediatric craniopharyngioma: recurrence pattern and prognostic factors. Childs Nerv Syst 17:531–536
Kristopaitis T, Thomas C, Petruzzelli GJ, Lee JM (2000) Malignant craniopharyngioma. Arch Pathol Lab Med 124:1356–1360
Laws ER (1994) Transsphenoidal removal of craniopharyngioma. Pediatr Neurosurg 21(Suppl 1):57–63
Maira G, Anile C, Colosimo C, Cabezas D (2000) Craniopharyngioma of the third ventricle: trans-lamina terminalis approach. Neurosurgery 47:857–865
Maira G, Anile C, Albanese A, Cabezas D, Pardi F, Vignati A (2004) The role of transsphenoidal surgery in the treatment of craniopharyngiomas. J Neurosurg 100:445–451
Merchant TE, Kiehna EN, Sanford RA, Mulhern RK, Thompson SJ, Wilson MW, Lustig RH, Kun LE (2002) Craniopharyngioma: St. Jude children’s research hospital experience 1984–2001. Int J Radiat Oncol Biol Phys 53:533–542
Miller DC (1994) Pathology of craniopharyngiomas: clinical import of pathological findings. Pediatr Neurosurg 21(Suppl 1):11–17
Muller HL, Bueb K, Bartels U, Roth C, Harz K, Graf N, Korinthenberg R, Bettendorf M, Kuhl J, Gutjahr P, Sorensen N, Calaminus G (2001) Obesity after childhood craniopharyngioma—German multicenter study on pre-operative risk factors and quality of life. Klin Padiatr 213:244–249
Pascual JM, Gonzalez-Llanos F, Roda JM (2004) Intraventricular craniopharyngiomas: topographic classification and surgical approach selection based on an extensive overview. Acta Neurochir (Wien) 146:785–802
Patterson RH Jr, Danylevich A (1980) Surgical removal of craniopharyngiomas by a transsphenoidal approach through the lamina terminalis and sphenoid sinus. Neurosurgery 7:111–117
Pierre-Kahn A, Sainte-Rose C, Renier D (1994) Surgical approach to children with craniopharyngiomas and severely impaired vision: special considerations. Pediatr Neurosurg 21(Suppl 1):50–56
Poretti A, Grotzer MA, Ribi K, Schonle E, Boltshauser E (2004) Outcome of craniopharyngioma in children: long-term complications and quality of life. Dev Med Child Neurol 46:220–229
Price DA, Wilton P, Jonsson P, Albertsson-Wikland K, Chatelain P, Cutfield W, Ranke MB (1998) Efficacy and safety of growth hormone treatment in children with prior craniopharyngioma: an analysis of the Pharmacia and Upjohn International Growth Database (KIGS) from 1988 to 1996. Horm Res 49:91–97
Rajan B, Ashley S, Gorman C, Jose CC, Horwich A, Bloom HJ, Marsh H, Brada M (1993) Craniopharyngioma—a long-term results following limited surgery and radiotherapy. Radiother Oncol 26:1–10
Rajan B, Ashley S, Thomas DG, Marsh H, Britton J, Brada M (1997) Craniopharyngioma: improving outcome by early recognition and treatment of acute complications. Int J Radiat Oncol Biol Phys 37:517–521
Shibuya M, Takayasu M, Suzuki Y, Saito K, Sugita K (1996) Bifrontal basal interhemispheric approach to craniopharyngioma resection with or without division of the anterior communicating artery. J Neurosurg 84:951–956
Srinivasa J, Dailey AT, Berger MS (1999) The bifrontal olfactory nerve-sparing approach to lesions of the suprasellar region in children. Pediatr Neurosurg 30:245–252
Steno J, Malacek M, Bizik I (2004) Tumor-third ventricular relationships in supradiaphragmatic craniopharyngiomas: correlation of morphological, magnetic resonance imaging, and operative findings. Neurosurgery 54:1051–1060
Stripp DC, Maity A, Janss AJ, Belasco JB, Tochner ZA, Goldwein JW, Moshang T, Rorke LB, Phillips PC, Sutton LN, Shu HK (2004) Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. Int J Radiat Oncol Biol Phys 58:714–720
Sutton LN (1994) Vascular complications of surgery for craniopharyngioma and hypothalamic glioma. Pediatr Neurosurg 21(Suppl 1):124–128
Tomita T, McLone DG (1993) Radical resections of childhood craniopharyngiomas. Pediatr Neurosurg 19:6–14
Van Effenterre R, Boch A-L (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97:3–11
Van Effenterre R, Boch AL (1993) Radionecrosis of the optic chiasm. A clinical and radiological study of 3 cases. Neurochirurgie 39:75–84
Villani RM, Tomei G, Bello L, Sganzerla E, Ambrosi B, Re T, Giovanelli Barilari M (1997) Long-term results of treatment for craniopharyngioma in children. Childs Nerv Syst 13:397–405
Wang KC, Kim SK, Choe G, Chi JG, Cho BK (2002) Growth patterns of craniopharyngioma in children: role of the diaphragma sellae and its surgical implication. Surg Neurol 57:25–33
Yasargi MG, Curcic M, Kis S, Siegenthaler G, Teddy PJ, Roth P (1990) Total removal of craniopharyngiomas. Approaches and long-term results in 144 patients. J Neurosurg 73:3–11
Zuccaro G, Jaimovich R, Mantese B et al (1996) Complications in paediatric craniopharyngioma treatment. Childs Nerv Syst 12:385–391
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tomita, T., Bowman, R.M. Craniopharyngiomas in children: surgical experience at Children’s Memorial Hospital. Childs Nerv Syst 21, 729–746 (2005). https://doi.org/10.1007/s00381-005-1202-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-005-1202-9