Abstract
Introduction
Nuclear medicine shuntograms using the radiotracer technetium-99m diethylenetriaminepentaacetic acid have been used for many years as an additional method to assess shunt patency and performance.
Methods
The medical records of all children who had shuntograms performed at the Children’s Hospital of Eastern Ontario between January 13, 2000, and January 10, 2003, were retrospectively reviewed. There was a total of 68 procedures in 56 patients with an average age of 9 years 3 months. During the same period there were 123 shunt revisions.
Results
Forty-two shuntograms were reported as normal. Of these, ten were identified to be false negative. Two children with fractured shunts had shuntograms performed in order to assess for cerebrospinal fluid flow patency; the shuntograms were identified to be normal, confirming shunt dependence, and the shunt replaced. Twenty-six shuntograms were reported as abnormal in 24 patients; 17 went on to have surgery and the shunt malfunction was confirmed. Seven patients did not require surgery: five were declared shunt independent, two patients clinically improved after severe constipation was treated.
Conclusions
Approximately one fourth of all shuntograms reported as normal are not (false-negative rate=25%). Review of five other major studies between 1980 and 2003 have reported false-negative rates between 2 and 36%, which may be explained by variations in shuntogram protocols. A standardized method is proposed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Shuntograms have been introduced to assess shunt patency when clinical and other neuroimaging studies cannot ascertain a shunt malfunction requiring surgical correction. Both iodinated contrast material and radiotracers have been used for this purpose. The latter are more popular and very small volumes are required to perform the procedure. Different types of radionuclides have been used: iodine 131 (131I) serum albumin (RISA 131) was introduced in 1959 [2], technetium 99m (99mTc)-DTPA in 1966 [7], and indium 111 (111In)-DTPA in 1973 [9].
99mTc-DTPA is the radionuclide of choice for shuntogram studies. It is injected into the shunt reservoir and followed along its passage through the shunt. Both proximal and distal shunt patency can be established, especially when clinical symptomatology and standard neuroimaging [i.e., brain computed tomography (CT), shunt survey] have not been conclusive in suggesting a shunt malfunction. Shuntograms, however, have been reported to have false-negatives rates ranging between 2 and 36% [8, 10, 13, 14, 16]. It was decided to audit the shuntograms performed at Children’s Hospital of Eastern Ontario (CHEO) in order to determine if these procedures have yielded useful information with respect to evaluating shunt patency and the need to perform surgery.
Methods
The medical records of all children who underwent shuntograms in a 3-year period between January 13, 2000, and January 10, 2003, were identified and reviewed. The information extracted from the charts included the etiology of the hydrocephalus, the type of shunt system and valve, presenting symptoms, preliminary shunt investigation results (i.e., brain CT, shunt survey), shuntogram results, and the surgical findings.
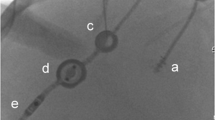
Patients undergoing shuntograms at the Children’s Hospital of Eastern Ontario (CHEO) fast for 3 h with no position or movement restrictions before the procedure. These are children who are suspected of having a shunt malfunction and are fasting either because they have been vomiting or surgery is being anticipated. The shuntogram protocol at CHEO was developed by the radiology department. The patients are placed either in the supine or prone position with the head turned away from the shunt site. The scalp overlying the valve is slightly shaved, the area prepped using proviodine, and a small sterile drape applied. The reservoir portion of the valve is punctured with a 25-gauge needle without distal compression. Return of cerebrospinal fluid (CSF) into the needle hub is considered an indication of a correct puncture and ventricular catheter patency. There is no attempt to actively withdraw any CSF. A syringe containing 1 mCi of 99mTc-DTPA (equivalent to 37 MBq), with an average volume of 0.10 ml, is then inserted into the needle hub and the radiotracer injected. The tracer is imaged by a gamma camera every 30 s and the tracer followed along its path down the shunt. The children are kept in the same position. The time of peritoneal spillage, if any, is recorded. If there is no peritoneal spill noted at 20 min, the patients are allowed to sit for 5 min, and then reimaged. This repositioning procedure may be repeated until peritoneal spillage occurs, or it is clear that it is not going to occur.
Two pediatric radiologists performed the procedure and interpreted the results. Based on their reports, shuntograms were categorized as either normal or abnormal. A normal shuntogram would be one with the spontaneous appearance of CSF within the needle hub and peritoneal spillage within 20 min. Then, depending on the course of events, the designations of false negative, true negative, or true positive were applied. In false-negative studies, the shuntogram was reported as normal; however, surgery was performed because of persisting symptoms, and a shunt malfunction was identified. If the symptoms spontaneously subsided or later were identified not to be shunt related and there were no further concerns during the years 2000–2003, then the shuntogram was designated as a true-negative study. The true positive category was used if the shuntogram demonstrated a shunt malfunction and surgery confirmed the malfunction and corrected the symptoms. Patients whose shuntograms showed shunt patency, but the radiologist observed that the tracer moved “somewhat slowly”, were placed in this group. The false-positive rate could not be calculated because although there was a group of patients that demonstrated a positive shuntogram that went on to improve and stay well during the 2000–2003 period, surgery was never performed. For the same reason, any diagnostic outcome measures (i.e., sensitivity, specificity, positive or negative predictive values) have no validity because not every shuntogram was followed by the “gold standard” of surgery.
Shunt surgery consisted of first exploring the shunt system in the operating room while the patient was under general anesthesia. The ventricular catheter was disconnected from the valve, and both the proximal and distal ends manometrically assessed. Depending on the pressures and flows obtained, the site of shunt malfunction was documented and the shunt revised.
Results
Sixty-eight shuntograms were performed in 56 patients. During the same 3-year period there were 123 shunt revisions. Age ranged between 5 months and 20 years at the time of shuntogram, with a mean of 9 years 3 months and a median of 10 years. The most common population of patients with hydrocephalus requiring shuntogram evaluation consisted of those with spina bifida and ventriculoperitoneal shunts (Tables 1 and 2). In the 68 shuntograms, there were 58 shunts tested with pressure differential valves without antisphoning devices (PS Medical, Medtronic) and ten with Delta valves.
Forty-two shuntograms were reported as normal and 26 as abnormal. Two of the 42 normal shuntograms were performed to assess for patency of CSF flow in asymptomatic patients with fractured shunts; CSF flow through the shunt seemed patent and surgery was performed. Ten out of remaining normal studies were classified as false negative after surgery identified shunt malfunctions (false-negative rate=25%). There were seven distal revisions and three proximal revisions. All of these were associated with pressure differential valves without antisiphoning devices.
Out of the 26 abnormal shuntograms, surgery was required in 17 cases and all were confirmed to have shunt malfunctions (true-positive rate=100%). Seven patients had proximal revisions, four had distal revisions, two had their valves changed only, one had a disconnected “Y” catheter reconnected, two had complete shunt replacements, and one had the conversion of a ventriculoperitoneal to a ventriculopleural shunt. The 17 cases operated on included two patients with abnormal shuntograms that were initially observed because of resolution of symptoms; when the symptoms recurred, the shuntograms were repeated and surgery performed. In the remaining seven patients with abnormal shuntograms that did not go on to have surgery, three patients had symptoms that resolved and never recurred; two of these patients had constipation treated and their symptoms eventually resolved once the constipation was managed. There were four asymptomatic patients that had shuntograms performed (subsequently identified to be abnormal) because of brain CT or shunt survey changes; these patients have remained well. Five of the seven patients with abnormal shuntograms seem to be shunt independent, but they will continue to be followed. The total of 29 patients who underwent surgery are presented in Table 3 along with the shuntogram results, type of surgery performed, and presenting symptoms.
Discussion
Since the report of Di Chiro and Grove in 1966, shuntograms using 99mTc-DTPA have evolved [7, 8]. The fundamental goal of this procedure, however, has remained the same: to determine whether or not a shunt is working. With pressure differential valves, CSF drains more rapidly from ventricles when the patient is active (standing, moving around, or crying) [8]. Even after cessation of activity, CSF may continue to drain more rapidly for a small period even if the patient is lying down, because of siphoning. This increase in flow may possibly overcome some partial shunt obstruction. For this reason, some centres insist that their patients remain supine and inactive for up to an hour before being tested [3, 15, 16]. Flow-regulated valves and those that possess antisiphoning mechanisms are less susceptible to changes in pressure and gravity influences.
Some centres use shunt systems containing reservoir antechambers proximal to the valve for CSF access [14–16]. In these instances, ventricular reflux is easier to assess with the valve completely compressed during the shuntogram procedure; this is the closest one can come to non-invasively administering the radiotracer directly into the ventricular system [8]. Otherwise, the radiotracer may travel directly down the distal catheter without any ventricular reflux.
Although the presence of CSF flowing out of the reservoir portion of the valve after being punctured with the 25-gauge needle indicates some flow from the proximal catheter, it cannot entirely rule out a partial proximal catheter obstruction. Some studies report active aspiration between 1 and 3 ml of CSF, primarily for analysis [1, 8, 10, 15]. Although, this may ascertain some degree of ventricular patency, a partial malfunction may be missed. Identification of CSF in the needle hub indicates a correct puncture; however, further assessment by the continuation of flow observation may assist in improving the identification of shunts with proximal malfunctions.
In those patients who do not have a proximal antechamber reservoir, the radiotracer is injected into the reservoir portion of the valve while either the distal end of the valve or the peritoneal catheter immediately distal to the valve is compressed. It is difficult to compress the distal portion of the valve and inject proximally, especially in small valves or in older children with increased subcutaneous tissue. It is even more difficult to locate and immobilize the distal tubing, let alone completely compress it.
99mTc-DTPA is a very efficient radiotracer with volumes as little as 0.05 ml required to conduct a shuntogram. This diminishes the problem of a large pressure increase as a result of the radiotracer volume injected, which may transiently overcome a partial proximal shunt obstruction. For example, an 11-cm ventricular catheter with a diameter of 1.5 mm has a volumetric capacity of 1.9 ml; proximal injection of such a volume may overcome a partial shunt malfunction and falsely suggest a functioning shunt. Some centres continue to perform shuntograms using iodinated contrast material [1, 3]. Disadvantages include the higher injection volumes (i.e., 2–3 ml) required, the risk of possible allergic reactions, and the requirement of X-rays. Radiotracer shuntograms have largely replaced iodinated contrast studies for these reasons. However, centres performing radiotracer shuntograms are using volumes up to 1 ml, usually after an attempted withdrawal of a similar or larger volume [8, 10, 13–16]. The lowest recorded volume used at CHEO was 0.07 ml and the highest 0.17 ml, the variability depending on the time of day the radiotracer was used in order to achieve an activity of 1 mCi. Thus, the studies at CHEO have been purely diagnostic, and not therapeutic by using a larger volume in order to obtain ventricular reflux, and by doing so possibly overcoming a partial shunt malfunction.
Shuntograms visually track the flow of CSF associated with the radiotracer; however, it may be difficult to ascertain whether or not it is moving fast enough unless one has a basis for comparison with a normally functioning shunt with a similar valve system. Although most shuntograms performed at CHEO were those in children with spina bifida with ventriculoperitoneal shunts and pressure differential valves, the influence of other shunt systems and valves is unknown. It was usually left up to the radiologist to provide that interpretation. Calculation of the CSF clearance half-time via construction of a time–activity curve has been reported to be a quantitative depiction of shunt function [15, 16]. The shape of the curve has also been reported to be useful in diagnosing distal obstruction, although it may be misleading when investigating proximal obstruction [16]. The construction of the time–activity curve depends on the gamma counts emitted by the radiotracer at the injection site. Rapid clearance may be a result of losing radioactivity from ventricular reflux occurring simultaneously with distal radiotracer flow. Caution should therefore be applied when interpreting time–activity curves, especially with different shunt and valve systems.
Although all patients are initially lying down when the tracer is being administered, that same position may not be maintained for the duration of the study. If peritoneal spillage does not occur by a certain time, some centres allow patients to sit up, move around, or even have their shunts pumped in order to facilitate the flow of CSF [1, 8, 10, 13, 16]. Although this practice may enhance the radiotracer flow, in order to ascertain that the shunt is not completely blocked, it does not mimic regular shunt function and a partial malfunction may be missed. If a shunt only functions well when it is pumped or the patient is sitting up, then it is most likely not working properly [8]. In pressure differential valves, not only the intraventricular pressure, but also gravity and siphoning, affect the flow of CSF [16].
Ideally, false negatives should only be determined after surgery is performed to identify a malfunctioning shunt when the shuntogram was reported as normal. However, unless there are persistent neurological symptoms, a shunt with a normal shuntogram would not be explored. It is assumed, therefore, that if a patient has a normal shuntogram, resolution of symptoms, and does not require further investigation, that the shunt is not at fault. Some centres factor in all of the patients who had shuntograms, as opposed to including only the normal studies in the denominator, which artificially reduces their false-negative rate [14]. In addition, it is important to be careful in classifying shuntograms as normal in patients that were allowed to sit up or have their shunts pumped.
The most accurate shuntogram procedures would be those with the lowest false-negative rates. Compared with other shuntogram studies (Table 4) our false-negative rate of 25% is high [10, 13, 14, 16]. At CHEO, patient positioning and movements are not restricted before the test, so the theoretical possibility remains that siphoning may still be occurring for a short period. Antechamber reservoirs proximal to the valve are not used. Correct puncture and some degree of ventricular patency is ascertained by the free flow of CSF into the needle hub. A very small volume of radiotracer is injected directly into the reservoir portion of the valve, without distal compression, and static images are acquired by a gamma camera at 5-min intervals without quantitative flow analysis.
Four out of the five major series in the literature [10, 13, 14, 16] injected the radiotracer into antechambers with distal compression in order to attain ventricular reflux. This may be correlated with the lowest false-negative rates (2, 11, 14, and 14%). French et al. used a variety of shunt systems, some with and others without a reservoir antechamber; they reported the highest false-negative rate (36%) [8]. Unless forced, how does the radiotracer reflux so rapidly into the ventricular system against the pressure and flow of CSF? Is it possible that the radiotracer dilutes into the ventricular system via a concentration gradient against the flow of CSF? If that is the case, then is the assessment of ventricular reflux of any importance? Although the presence of a proximal antechamber seems to facilitate this, is it really necessary? The ten false negatives during the 3-year study at CHEO were a result of three proximal and seven distal shunt malfunctions. If a test for ventricular reflux was successful in predicting the three proximal malfunctions, the false-negative rate would decrease from 25 to 19% (i.e., one of five false negatives instead of one of four); this was more dramatic in the report by O’Brien et al. who calculated the false-negative rate would fall from 14 to 3% [14].
CSF transit time may also vary depending on allowances to sit, stand, and walk during the shuntogram. Lack of comparison of the CSF clearance half-time with standardized curves may decrease the study’s accuracy. For example, shuntograms at CHEO were reported as “normal” by the radiologist with a peritoneal spillage at 10–15 min, whereas five patients with a similar peritoneal spillage time were reported as “a little slow.” Although shunts that are functioning properly may vary in their descent of CSF into the peritoneal cavity, in the majority of time a peritoneal spill within 10 min is considered normal [16]. An analysis of the rate of CSF flow may be able to detect subtle discrepancies and better assess if a shunt is draining too slowly, or in the case of overdrainage, too quickly [13, 15, 16]. It has been reported that the 99mTc-DTPA half-disappearance time in normally functioning shunts is 0.5–6.0 min [15]. Vernet et al. identified that tracer injection into the reservoir may be associated with rapid entry into the peritoneal cavity, even when the ventricular catheter is blocked. They concluded that rapid radionuclide clearance is useful in eliminating a distal obstruction as a possibility, but may be misleading when diagnosing a proximal malfunction [16].
Constipation, the use of a corset, pregnancy, or anything else that makes abdominal pressure exceed intracranial pressure may decrease the pressure gradient, slow the rate of CSF drainage, and cause a shunt to malfunction [15]. In fact, abdominal problems account for up to a quarter of all shunt malfunctions. Constipation affects as many as 1.5–5.7% of all healthy children; as many as 90% of children with spina bifida are chronically constipated [5]. Depending on abdominal compliance, the effect of constipation on pressure differential shunts may be variable. It would be logical to treat a child’s severe constipation first and see if the intracranial symptoms subside.
Graham et al. has reported the lowest false-negative rate of 2% [10]. Their protocol did not mention any pre-shuntogram positioning restrictions or quantitative CSF flow analysis. A small volume of CSF was first withdrawn from the antechamber reservoir and 0.1 ml of 99mTc-DTPA injected followed by an additional volume of 0.3 ml of CSF with simultaneous distal transcutaneous compression. Although the patients were allowed to move around and later be reimaged, if there was no peritoneal spillage by 45 min, the shuntograms were considered positive. Forty-five minutes for peritoneal spillage is considered by most studies to be a long transit time. Surprisingly, only two of 105 normal shuntograms were identified to have shunt malfunctions. The long-term follow-up on the remaining 103 normal shuntograms was not discussed. What were the patient symptoms attributed to, and did they subside? Was it necessary to explore the shunts a few weeks or months later? Furthermore, there was a high false-positive rate; 11 of 76 abnormal shuntograms were identified to have functioning shunts at surgery. These 11 shuntograms were declared abnormal based on the absence of ventricular reflux. The comment was that absence of ventricular reflux may occur in normal shunts. Ventricular reflux is not synonymous with the return of CSF after puncturing of the shunt reservoir; the latter is a better determinant of proximal catheter patency, especially if the spontaneous flow of CSF can be assessed.
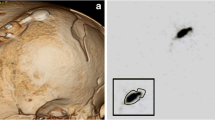
Broken shunts are usually identified on shunt surveys and may continue to function as a result of CSF tracking through a reactive epithelial fibrous sheath, which consistently forms with time around shunts [4, 6, 17]. This may yield a misleading shuntogram result, as patency is not always synonymous with adequate shunt function [4, 8]. If the shuntogram reveals no flow through the shunt, then the patient may be shunt independent [17]. Patients with spina bifida may never be diagnosed as shunt independent and almost always require shunt revisions [6]. If the shuntogram is reported as normal, even though the catheter is broken, then the shunt is usually revised electively. This is because the fibrous sheath will eventually cease to act as a conduit for the CSF and the patient may begin to experience symptoms of shunt malfunction [11, 12, 17]. It is even possible that flow through the fibrous tract may be position dependent [4].
It is important to note that although some shuntograms may yield high false-negative results, they are usually performed when other available information or imaging are negative or equivocal. Patients who obviously have shunt malfunctions or those who obviously do not, do not require shuntograms. In some way then, the false-negative rate depends on the threshold of performing the shuntogram and later surgically exploring the shunt.
The false-negative rate at CHEO during the 3-year study period indicates that one of every four shuntograms reported as normal may have an associated shunt malfunction. All of these malfunctions have been shown intraoperatively to be partial rather than complete. This may explain the equivocal clinical presentation and initial neuroimaging studies. With such a high false-negative rate, is it then worthwhile to continue performing shuntograms? Shuntograms may often be avoided by repeating the other neuroimaging studies and continuing to observe the patients’ symptoms. At times, this may require hospital admission. This contrasts with the cost of performing a shuntogram, which averages Can $250.00 at CHEO. Although clinical symptoms were present in 28 of the 29 patients that eventually went on to have shunt revisions (Table 3), surgery was not immediately offered because of the equivocal initial neuroimaging. In these cases, shuntograms may possibly be delayed or even avoided if the patients continue to be carefully monitored. Alternately, the shunt may be explored earlier with the clinical information at hand. Although there is the theoretical risk of creating a shunt malfunction or an infection during the shuntogram, there have been no complications associated with this procedure at CHEO or reported in the literature.
The misdiagnosis rate will remain high as long as a standardized method is not used. The criteria for performance of shuntograms need to be narrowed and standard transit times identified for the various shunt systems and valves available. Factors such as pre-shuntogram positioning, volume of radiotracer injected, volume and flow of CSF return into the needle hub, placement of proximal antechambers, assessment of ventricular reflux, positioning and valve pumping during the procedure, peritoneal spillage time, the construction of a time–activity curve, patient factors (i.e., pain, crying, constipation), and the length of patient follow-up can all contribute to the variable misdiagnosis rates reported in the literature. Shunts may not require surgical intervention with absent ventricular reflux or even prolonged transit times. On the other hand, there may exist a proximal shunt malfunction with the presence of ventricular reflux or even a normal transit time, or a distal shunt malfunction with a normal transit time and a normal peritoneal cavity dispersion.
The following is a proposed standardized method that may have an impact in diminishing the misdiagnosis rate. After skin preparation and insertion of a 25-gauge needle into the reservoir portion of the shunt system, assessment of the presence of CSF for proximal catheter patency is done. This can be further evaluated by attaching a 12-in. clear tubing and observing how well the CSF flows that distance spontaneously. The tubing can then be disconnected, the contents sent for laboratory assessment, and a syringe containing a small volume of radiotracer inserted into the needle hub and the contents injected (using a combined assembly butterfly needle and tubing requires a larger injection volume). This will be primarily for distal patency assessment. A peritoneal spillage time of 10–15 min could be considered normal for ventriculoperitoneal shunts without any valve pumping or patient repositioning.
The threshold for performing shuntograms can also be lowered. For example, constipation, if present, could be treated first. In the event of incidental fractured shunts in asymptomatic patents, shuntograms are useful for shunt-dependency assessment. If peritoneal spillage occurs then the shunt should be revised. If not, the child may be considered shunt independent; however, that patient should continue to be followed up and not lost to follow-up. It has been observed that such patients may present a few months or years later with symptoms of increased intracranial pressure and require surgery.
Conclusion
The necessity to perform shuntograms should be carefully evaluated in each institution. At CHEO, the discovery of a high false-negative rate of 25% will result in a change of practice, primarily in reducing the frequency of performing this procedure.
References
Bartynski WS, Valliappan S, Uselman JH, Spearman MP (2000) The adult radiographic shuntogram. Am J Neuroradiol 21:721–726
Bell RL (1959) Isotope transfer test in the diagnosis and treatment of hydrocephalus. Int J Appl Radiat 5:89–93
Benzel EC, Mirfakhraee M, Hadden TA (1991) Evaluation of CSF shunt function: value of functional examination with contrast material. Am J Neuroradiol 12:143–147
Blair K, AuCoin R, Kloiber R, Molnar CP (1989) The complementary role of plain radiographs and radionuclide shuntography in evaluating CSF-VP shunts. Clin Nucl Med 14:121–123
Bragg CL, Edwards-Beckett J, Eckle N, Principe K, Terry D (1994) Ventriculoperitoneal shunt dysfunction and constipation: a chart review. J Neurosci Nurs 26:265–269
Clyde BL, Albright AL (1995) Evidence for a patent fibrous tract in fractured, outgrown, or disconnected ventriculoperitoneal shunts. Pediatr Neurosurg 2:20–25
Di Chiro G, Grove AS Jr (1966) Evaluation of surgical and spontaneous cerebrospinal fluid shunts by isotope scanning. J Neurosurg 24:743–748
French BN, Swanson M (1981) Radionuclide-imaging shuntography for the evaluation of shunt patency. Surg Neurol 16:173–182
Gilday DL, Kellam J (1973) 111In-DTPA evaluation of CSF diversionary shunts in children. J Nucl Med 14:920–923
Graham P, Howman-Giles R, Johnston I, Besser M (1982) Evaluation of CSF shunt patency by means of technetium-99 m DTPA. J Neurosurg 57:262–266
Kazan S, Acikbas C, Rahat O, Tuncer R (2000) Proof of the patent subcutaneous fibrous tract in children with V-P shunt malfunction. Childs Nerv Syst 16:351–356
Lorber J, Pucholt V (1981) When is a shunt no longer necessary? An investigation of 300 patients with hydrocephalus and myelomeningocele: 11–22 year follow up. Z Kinderchir 34:327–329
May CH, Aurisch R, Kornrumpf D, Vogel S (1999) Evaluation of shunt function in hydrocephalic patients with the radionuclide 99mTc-pertechnetate. Childs Nerv Syst 15:239–245
O’Brien DF, Taylor M, Park TS, Ojemann JG (2003) A critical analysis of ‘normal’ radionucleotide shuntograms in patients subsequently requiring surgery. Childs Nerv Syst 19:337–341
Uvebrant P, Sixt R, Bjure J, Roos A (1992) Evaluation of cerebrospinal fluid shunt function in hydrocephalic children using 99mTc-DTPA. Childs Nerv Syst 8:76–80
Vernet O, Farmer JP, Lambert R, Montes JL (1996) Radionuclide shuntogram: adjunct to manage hydrocephalic patients. J Nucl Med 37:406–410
Vinchon M, Fichten A, Delestret I, Dhellemmes P (2003) Shunt revision for asymptomatic failure: surgical and clinical results. Neurosurgery 52:347–356
Acknowledgements
The authors would like to thank Mr. Scott Walker, technical supervisor of the Nuclear Medicine Unit at CHEO, for all of his expertise and support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vassilyadi, M., Tataryn, Z.L., Matzinger, M.A. et al. Radioisotope shuntograms at the Children’s Hospital of Eastern Ontario. Childs Nerv Syst 22, 43–49 (2006). https://doi.org/10.1007/s00381-005-1153-1
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-005-1153-1