Abstract
Objective
Brainstem tumor models are required to advance the treatment for diffuse pontine gliomas in children. The feasibility of creating an experimental rodent model by inoculating newborn pups with tumor cells was examined. The study was performed to create an animal model for diffuse brainstem tumors.
Methods
Eighty-two Fischer rat pups aged 12–24 h were anesthetized by hypothermia. The brainstem was injected with saline to identify anatomical coordinates for subsequent tumor cell challenges. The newborn pups were then inoculated with F98 (n=30) or 9L (n=30) glioma cells. Animals were returned to their mother for nursing. Tumor growth was assessed by survival and histopathology.
Results
Twenty-one percent of the saline-treated animals (17 out of 82) and 5% of the tumor cell-challenged pups (3 out of 60) were eliminated by their mothers. Inoculations with 9L and F98 cells produced brainstem tumors in 83% (24 out of 29) and 93% of animals (26 out of 28) respectively that were evaluated.
Conclusions
Our results demonstrate that neonatal rat models for brainstem tumors can be prepared using known injection coordinates and orthotopic cell lines. Decreasing rates of maternal removal during the course of the work suggests that the method involves a learning curve.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
New methods are required to treat brainstem tumors in children. The need is critical for these tumors in the central nervous system (CNS), which are shielded from systemic drug therapies by the blood–brain barrier. To investigate intratumoral drug treatments, we developed experimental models of brainstem tumors in adult rodents [12]. A neonatal model would more closely resemble the pediatric disease and accelerate clinical investigations.
Experimental neonatal tumors have been expressed by treating pregnant animals with carcinogenic agents, or by inoculating newborn animals with tumor cells. The former technique is less suited to studies of drug efficacy for several reasons [8]. The carcinogens may have variable in utero distribution and produce different types of tumors. Some litter mates may be unaffected, while others may have small or large tumors. Although direct inoculations can achieve highly uniform tumor doses, the capacity of the developing brainstem to tolerate inoculations and tumor cell challenges is unknown. There is a significant risk of surgical morbidity because the brainstem, unlike the cerebral cortex, has little functional redundancy [5]. A second question to be answered was whether the tumor cell-challenged animals could be returned to the mother for nursing. We have a clinical impression that female Fischer rats, which are commonly used in studies of brain tumor therapy, reject pups that have been marked by experimental manipulations.
Several studies involving neonatal inoculations in the cerebral cortex of mice and rats have used hypothermia for anesthesia [8, 10]. These results suggest that the method may be adapted to the preparation of brainstem models. The present study demonstrates that the neonatal brainstem can be inoculated with orthotopic tumor cells.
Materials and methods
Animals
Pregnant female Fischer 344 rats were obtained from Harlan (Indianapolis, IN, USA). Once these rats delivered the pups, the newborn pups were caged with their mothers and allowed to nurse freely. Pups 12 to 24 h old were used for the inoculations. All procedures were conducted according to established Institutional and Federal guidelines and with the prior approval of the Johns Hopkins Animal Care and Use Committee.
Induction of anesthesia
Pups were anesthetized by hypothermia [10]. Animals were removed from their mother, placed in a gauze-lined box, and placed in a −30°C chamber for 20 min. Upon removal from the box, the animals remained anesthetized for about 10 min, during which time the animals were inoculated with saline or tumor cells.
Intracranial injections of saline and cells
Implantation procedures were carried out in a clean but non-sterile environment. Prior to injection, the injection site was painted with a cotton tip applicator containing sufficient Betadine solution to cover a skin area approximately 3 mm in diameter around the injection site.
Initially, a 5- to 6-mm midline incision was made to expose the skull surface for injections through the cartilaginous plate. This procedure was discontinued when it appeared to be associated with a high rate of maternal rejection. Subsequently, animals were injected with 2 μl of saline or cell suspensions through the Betadine-painted skin using a 10-μl Hamilton syringe (Hamilton, Reno, NV, USA). The needle was covered with a plastic sleeve to permit an injection depth of 3.0 mm from the skin. Injections were 1 mm to either side of the midline, and 1 mm posterior to the interaural line. The suture could be visualized with a strong light. The needle was withdrawn 15 s after injection of the cell suspension (Fig. 1) . Light pressure was then applied to the injection site for a further 15 s. The pups were transferred to a room-temperature sterile surface until they regained consciousness and then returned to their mother.
Survival
Pups were observed at least once daily. Animals showing signs of distress or neglect were removed and euthanized by intraperitoneal sodium pentobarbital (1 g/kg) after an initial dose of intraperitoneal ketamine (10 mg/kg). Animals removed by the mother and those who survived for more than 60 days were not counted in the tumor survival analysis. Survival analysis was then calculated using JMP (SAS Institution, Cary, NC, USA). Values of p<0.05 were considered statistically significant.
Histology
Immediately following the initial dose of anesthesia for euthanasia, animals were perfused with saline and 4% buffered formalin solution. The skull was opened and examined for tumor growth. The brainstem was sectioned to estimate tumor location and size. Tumor volumes were calculated by measuring length and width parameters with calipers. Sections were stained with hematoxylin–eosin (H&E) solutions for examination by light microscopy.
Results
Surgery
In an initial set of experiments, a 5- to 6-mm midline incision was made through the skin to allow exposure of the skull surface. Saline solutions and cells were injected using permissive coordinates similar to those listed in Table 1. Fifteen animals were injected with 2 μl of saline and 15 were injected with 2 μl of 9L cells. Although there was little evidence of trauma from the injections, 4 pups in the saline group and 6 in the cell group were removed by the mother within 2–4 days. In subsequent experiments, injections were made directly through the skin. The results reported here describe only the latter experiments.
Injection coordinates in rats
A posterior midline approach through the cerebellum and fourth ventricle was used to measure coordinates for injections of saline into the neonatal brainstems. Mothers eliminated 17 of the 82 pups (21%) injected with 2 μl of saline. Injections approximately 1 mm to either side of the midline were well tolerated in the neonatal rat. There appeared to be no long-term consequences of the saline injections. The animals were observed for at least 30 days. The cohort of animals that were not eliminated by their mother demonstrated no indication of increased morbidity or mortality from this treatment (Fig. 2).
Tumor cell injections
Thirty rats received intracranial (IC) implantation of F98 tumor cells and 30 received IC implants of 9L cells. The mothers eliminated 2 pups in the 9L group and 1 in the F98 cohort. Survival in the remaining animals appeared to be dose dependent. As shown in Table 2, median survival rates decreased from 25 days in animals injected with 1×104 9L cells to 18 days in pups injected with 1×106 cells. Similar results were observed in animals injected with increasing amounts of F98 tumor cells. The decrease in survival with increasing number of cell inoculations were significant for both types of tumor cells (p<0.05).
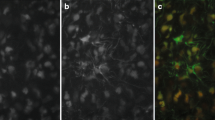
The development of neurologic symptoms in tumor-challenged animals is consistent with the effect on centers of respiration and consciousness. Figure 3 shows the histology of a brainstem implanted with F98 glioma on day 16. Morbidity generally was similar to that seen in adult brainstem tumor models [12]. The pups developed mild to moderate limb paralysis in the 24 h preceding death. The pups then became lethargic, lapsed into a coma, and died within 12–24 h.
Tumor volume
When 1×106 9L cells were injected into neonatal rat brainstems, tumors 4–5 mm in diameter occurred in 8 out of 10 animals within 21 days. When 1×105 cells were implanted, 6 out of 10 animals had tumors 4–5 mm in diameter at 21 days. After implantation of 1×104 cells 2 out of 10 animals had tumors larger than 4 mm at 21 days, and 20% of animals died within 21 days. At the time of death from the tumor, there was no significant difference in the tumor size among rats injected with 1×106, 1×105, and 1×104 cells. Similar results were obtained following implantation of F98 cells. Tumor growth was generally confined to the brainstem.
Discussion
The present report demonstrates that the newborn rat brainstem can be inoculated with tumor cells to afford an experimental neonatal brainstem tumor model. Two strategies were used to minimize trauma. First, the injection field was confined to the sites that have been determined to be tolerant in adults [12]. Little or no morbidity was observed with injections that ranged from the midline to approximately 1 mm lateral. An injection depth of 3–3.5 mm appeared safe. Sites more rostral or caudal than 1 mm posterior to the intraural line were not explored. It is reasonable to assume that additional sites could be injected safely, although such exploration was beyond the scope of the present effort. Second, the use of hypothermia, as described by Tamargo and coworkers [10], rather than chemical anesthesia, allowed minimal handling of the animals. Nonetheless, a learning curve undoubtedly is associated with this method. In the first section of the study, determination of injection coordinates, mothers removed 17 of the 82 (21%) pups injected with saline. In the second section, only 3 of the 60 (5%) pups injected with tumor cells were eliminated. Although we cannot quantitatively describe a technical difference, it seems likely that experience led to less trauma to provoke maternal rejections. We may also assume that the high morbidity we observed in the preliminary animal groups with incision to expose the skull landmarks reflected this learning curve.
The data shown in Table 2 demonstrate that survival was proportional to the number of cells injected. These data may be biased by an unblinded observer removing animals showing early signs of morbidity, yet the overall pattern suggests that the model could be used for efficacy studies. Tumor growth was generally centered in the brainstem, but both cell types show promiscuous growth into the fourth ventricle and brainstem. The maximum size of the tumors measured at autopsy was 4–5 mm in diameter regardless of the number of cells injected. This result suggests that morbidity was related to the mass of the tumor, an effect that is similar to the involvement of human and non-human primate brainstem lesions in reticular-activating centers [1, 3].
Diffuse pontine gliomas predominantly affect infants and children. There is a consensus among the neuro-oncology community that further efforts to promote systemic therapy without radiation are unlikely to be successful. Fortunately, experimental animal models are becoming available to examine several hypotheses that may account for the lack of progress. New xenographic models, in which human tumor cells have been injected into mouse and rat brains, have been described [11, 13], and more resources have been applied to transgenic mouse studies. A second hypothesis is that the blood–brain barrier prevents most systemic therapies from getting into brain tumors before the drugs impose intolerable side effects. This idea has been supported by tests measuring CNS levels of systemically administered drugs [4], and by studies in animal models demonstrating that local therapy significantly extends survival compared with systemic delivery [2]. We have demonstrated that chronically infused small drug therapy significantly prolongs survival in experimental models of adult rat brainstem tumors [2]. Studies have suggested that high molecular weight compounds, which are paradigms for targeted-toxin cancer chemotherapy, also can be infused safely into the rodent brainstem [6, 9]. The continued development of these models affords several opportunities for new approaches to brainstem tumor therapy.
Conclusion
We have developed a model in which brainstem tumors are efficiently and reproducibly established in neonatal rats. This approach should be useful for studies of new therapies to treat brainstem lesions.
References
Abbott R, Goh KYC (1999) Brainstem gliomas. In: Albright L, Pollack I, Adelson D (eds) Principles and practices of pediatric neurosurgery. Thieme, New York, pp 629–640
Carson BSS, Guarnieri M (2002) Local therapy for brain tumors. Adv Clin Neurosci 12:89–99
Fisher PG, Carson BS (1996) Management of brainstem gliomas in children. Contemp Neurosurg 18:1–7
Groothuis DR (2000) The blood-brain and blood-tumor barriers: a review of strategies for increasing drug delivery. Neurooncology 2:45–59
Klopp LS, Simpson ST, Sorjonen DC, Lenz SD (2000) Ventral surgical approach to the caudal brain stem in dogs. Vet Surg 29:533–542
Occhiogrosso G, Edgar MA, Sandberg DI, Souweidane MM (2003) Prolonged convection-enhanced delivery into the rat brainstem. Neurosurgery 52:388–394
Paxinos G, Watson C (1986) The rat brain in stereotaxic coordinates. Academic, Orlando
Peterson DL, Sheridan PJ, Brown WEJ (1994) Animal models for brain tumors: historical perspectives and future directions. J Neurosurg 80:865–876
Sandberg DI, Edgar MA, Souweidane MM (2002) Convection-enhanced delivery into the rat brainstem. J Neurosurg 96:885–891
Tamargo RJ, Epstein JI, Brem H (1988) Heterotransplantation of malignant human gliomas in neonatal rats. J Neurosurgery 69:928–933
Wetmore C, Eberhart DE, Curran T (2001) Loss of p53 but not ARF accelerates medulloblastoma in mice heterozygous for patched. Cancer Res 61:513–516
Wu Q, Tyler B, Sukay L, Rhines L, DiMeco F, Clatterbuck RE, Guarnieri M, Carson BS Sr (2002) Experimental rodent models of brainstem tumors. Vet Pathol 39:293–299
Xiao A, Wu H, Pandolfi PP, Louis DN, VanDyke T (2002) Astrocyte inactivation of the pRb pathway predisposes mice to malignant astrocytoma development that is accelerated by PTEN mutation. Cancer Cell 1:157–168
Acknowledgements
This work was supported by funds from the Children’s Cancer Foundation, Baltimore, MD, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jallo, G.I., Penno, M., Sukay, L. et al. Experimental models of brainstem tumors: development of a neonatal rat model. Childs Nerv Syst 21, 399–403 (2005). https://doi.org/10.1007/s00381-004-1100-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-004-1100-6