Abstract
Objects
The purpose of this study was to describe the indications, surgical techniques and postoperative outcome of neuroendoscopic interventions in a heterogeneous group of intracranial cystic pathologies.
Patients and methods
Between 1992 and 2003, 127 patients with symptomatic intracranial cysts and cystic tumours underwent neuroendoscopic treatment in our department. In 22 patients indication for surgery was colloid cysts, in 9 patients pineal cysts and in 3 patients cavum vergae cysts. Twelve arachnoid cysts, 10 cystic craniopharyngiomas, 2 Rathke’s cleft cysts and 69 malignant cystic tumours were operated on. The patients’ mean age was 45 years and their clinical presentations varied from typical signs of increased intracranial pressure to focal neurological deficits.
Results
One hundred and twenty-seven patients with intracerebral cystic space-occupying lesions were operated on using stereotactic frameless or frame-based endoscopic techniques. There was no operative mortality. The operative morbidity was 3.1% including 1 memory deficit due to fornix injury, 1 hemiparesis due to postoperative haematoma after lesion biopsy, 1 aseptic meningitis and 1 subdural fluid collection.
Conclusions
Endoscopic interventions enable neurosurgeons to manage intracranial cystic lesions. Via the same approach, the obstructed CSF pathways may be restored and consequently the increased intracranial pressure diminishes. With the aid of stereotactic guidance or a neuronavigation system, access to the lesion can be gained rapidly and with high accuracy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the past few years, neuroendoscopic procedures have gained increasing significance and have been used more widely in handling intracranial lesions [29, 41, 45, 69]. Especially in the diagnosis and therapy of cystic intracranial or intracerebral pathologies, endoscopic techniques are extremely helpful [6, 38, 92]. This group of space-occupying lesions includes colloid cysts, arachnoid cysts, porencephalic cysts, pineal cysts, Rathke’s cleft cysts, cystic craniopharyngiomas and malignant tumours with cystic components. Considering operative morbidity and mortality of stereotactic microsurgical approaches to the lesions, endoscopic surgery provides the safer outcome due to direct inspection of the capsular vascularisation and consistence. Either definite or palliative treatment for the above-mentioned lesions could be achieved using neuroendoscopic techniques, depending on the histopathological diagnosis and aim of the therapeutic intervention (Fig. 1). Contrary to the benign parenchymal or intraventricular cysts, volume reduction of cystic anaplastic astrocytomas and glioblastomas as well as metastases can be accomplished using endoscopic procedures in combination with the application of reservoir systems [38].
In the present study, we describe the indications, surgical techniques, and postoperative outcome of neuroendoscopic interventions in a heterogeneous group of cystic intracranial pathologies in adults.
Patients and methods
Patients
Between 1992 and 2003, 127 patients with symptomatic intracranial cysts and cystic tumours underwent neuroendoscopic treatment in our department. In 22 patients indication for surgery was colloid cysts, in 10 patients pineal cysts, and in 3 patients cavum vergae cysts. Twelve arachnoid cysts, 10 cystic craniopharyngiomas, 2 Rathke’s cleft cysts and 69 malignant cystic tumours were operated on. The patients’ mean age was 45 years (34–78 years), and their clinical presentations varied from typical signs of increased intracranial pressure to focal neurological deficits.
Instruments
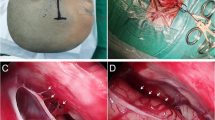
Different rigid and flexible endoscopes for neuroendoscopic interventions are available. The specifications vary and one must choose according to the preoperative approach planning and intraoperative findings. While rigid endoscopes provide brilliant pictures and offer the possibility of looking around corners due to the various angled lenses, flexible neuroendoscopes have the advantage of steerability and manoeuvrability. Flexible fiberscopes make inspections and interventions of multifocal and multiseptated cystic lesions easier [40]. At present, rigid endoscopes with two working channels and different viewing angles enable surgeons to perform a two-handed resection technique. A comprehensive set of instruments for multiple-purpose procedures are standard in our department (Fig. 2). The stability of the endoscope during the operative procedure is necessary and can be provided by the Marburg Endoscopy Fixation and Guiding System [38]. The introduction of computer-assisted navigation into neurosurgical practice led us to utilise two different guidance systems: frame-based stereotactic and image-guided neuroendoscopic procedures. Details concerning these two stereotactic systems and their applications were described in our previous report [41].
a The patient’s head is affixed in a vacuum pillow (arrow). The patient’s registration process can be performed without any technical problems and the navigation system has a high target accuracy. b Endoscopic view demonstrating biopsy of the tumour with the multipurpose bipolar forceps. c Working instruments (scissors, forceps, flexible bipolar coagulation and cutting electrode). d Rigid endoscope with two working channels enables a two-handed endoscopic technique to be performed
Operative techniques
After induction of general anaesthesia, the patient’s head is positioned and affixed either in the Mayfield head clamp or in a vacuum pillow depending on the location of the lesion and the navigation modalities (Fig. 2a) [85]. Current imaging data of the frameless system are obtained 1 day before the operation. The burr hole is localised and the trajectory to the lesions is planned. Following dural incision, the operating sheath containing the trocar is inserted with the aid of stereotactic or navigation guidance and is firmly fixed with the holding device [38]. Subsequently, the trocar is removed and the endoscope is introduced.
Neuroendoscopic technique in the treatment of intraventricular cysts
In intraventricular cystic lesions (colloid cyst, pineal cyst, cystic craniopharyngioma, Rathke’s cleft cyst), orientation of the endoscope is achieved by identifying the anatomical structures (the foramen of Monro, septal vein and thalamostriate vein). Concomitantly, the position of the endoscope is verified with its position displayed on the navigation monitor. In accordance with the combined data from endoscopic image and navigation guidance, the endoscope is then readjusted towards the target lesion. After exposure of the lesion surface, the cyst membrane is opened using the micro-scissors or micro-catheters. Thin membranes may also be fenestrated by multipurpose bipolar forceps (Fig. 2b) [76]. The colloid cystic content may be aspirated either directly through the rigid endoscope’s working channel or through an applied micro-catheter. If the content is too viscous (colloid cyst, cystic craniopharyngioma), it is aspirated by continuous rinsing. The remaining cyst capsule is vaporised using a radio-frequency probe. In colloid cyst patients or patients with craniopharyngioma, an external ventricular catheter is left in place after resection of the cyst wall in order to prevent aseptic ventriculitis that can be induced by the free-floating colloid material within the ventricular system. In the cases of pineal cysts, where the cyst is located in the posterior part of the third ventricle, a flexible endoscope is useful for approaching the lesion. The success of the intervention is confirmed intraoperatively by digital dynamic subtraction ventriculography in order to demonstrate the communication of the cystic lesion and ventricular system.
Neuroendoscopic technique in the treatment of arachnoid cysts and cystic neoplasms
Various rigid and flexible endoscopes are applied for cystostomy, cysto-ventriculostomy and cysto-cisterno-ventriculostomy. The operative procedure is performed according to the location of the lesion and the surrounding CSF space. Image guidance helps to localise the appropriate fenestration site and orientates the surgeon especially inside the arachnoid cyst. Micro-forceps and scissors are used to open and resect cystic membranes (Fig. 2c, d). In many cases, the application of electrosurgical device is necessary [39]. Coagulation probes with diameters of between 0.9 and 1.5 mm are available for both rigid and flexible endoscopes (Fig. 2c). The enlargement of stomas is performed with the aid of Fogarty balloon catheters. Digital dynamic subtraction cystography (cystoventriculography) is performed intraoperatively to display the communication of the fluid between the arachnoid cyst and the surrounding CSF compartments.
In the treatment of cystic neoplasms, localisation of the lesion is done by the navigation system and the rigid endoscope is introduced for biopsy. If necessary an Ommaya reservoir for repeated fluid aspiration is installed.
Results
From June 1992 to March 2003, 127 patients with intracerebral cystic space-occupying lesions were operated on using stereotactic frameless or frame-based endoscopic techniques. There was no operative mortality. The operative morbidity was 3.9% including 1 memory deficit due to fornix injury, 1 hemiparesis after biopsy, 1 aseptic meningitis and 1 subdural fluid collection. In this paper, we describe only some of the major lesion entities in detail.
Colloid cyst
In the early postoperative period, 22 patients had excellent outcomes, with immediately improved clinical signs. One patient who experienced intraoperative haemorrhage caused by laser application had reversible psychosis, memory deficit and third cranial palsy. Another patient remained shunt dependent caused by aseptic meningitis after the endoscopic procedure. In long-term follow-up examinations (1–10 years), 17 patients were symptom-free. One individual complained of intermittent headaches when facing stressful situations. Three other patients with preoperative memory deficits described gradual improvement. The patient who experienced intraoperative haemorrhage continued to have a slight short-term memory deficit. Follow-up imaging revealed an inconsistent decrease in ventricular size. Postoperative ciné MRI studies performed in 17 patients revealed the normal flow of CSF.
Pineal cyst
Nine cystic lesions of the pineal gland caused periodic headache and other unspecific symptoms (Fig. 3). Five preoperative neuroradiological examinations showed the cystic space-occupying lesion with enlarged ventricles. One individual revealed an obstructive hydrocephalus due to an aqueductal stenosis. All cysts were punctured and the content was aspirated using the flexible endoscope. The cystic membranous biopsies were pineal cysts in all patients. Adherent parts of the capsule were left in situ. The restoration of the CSF pathway was demonstrated intraoperatively by digital subtraction ventriculography (Fig. 3b) and postoperative MRI. All pineal cysts except one were without recurrence. Follow-up periods ranged between a few months and 10 years.
a MRI demonstrating a space-occupying lesion in the pineal region, which causes compression of the proximal aqueduct of Sylvius. b Intraoperative ventriculography revealing the flexible endoscope in the posterior part of the third ventricle and the cyst cavity filled with contrast media as a proof of patent cysto-ventriculostomy. c Postoperative T2-weighted MRI scan showing the flow-void phenomenon in the third ventricle and in the residual membrane of the pineal cyst. Note the decompressed cerebral aqueduct
Cystic craniopharyngioma and Rathke’s cleft cyst
After aspiration of the cystic content of the craniopharyngioma, the cyst wall is shrunk by laser beam or radio frequency application as much as possible. If parts of the capsule are adherent to parasellar structures, they are left in situ (Fig. 4). Eight patients are now without tumour recurrence, whereas in 2 patients, 9 and 12 months after the endoscopic intervention respectively, the remaining solid tumour portion was removed via a microsurgical technique.
a Contrast-enhanced coronal MRI shows a large cystic suprasellar lesion causing an occlusive hydrocephalus. Acute endoscopic intervention, with cyst evacuation and cystoventriculostomy, was performed due to deteriorated consciousness of the patient. Histopathological diagnosis revealed a craniopharyngioma. b Postoperative MRI examination reveals the totally evacuated cyst with the partial remnant of the tumour capsule. After patient’s condition improved, the membrane was resected via microsurgical intervention. c Preoperative T1-weighted MRI with contrast media demonstrates a cystic craniopharyngioma in a 74-year-old woman who presented with decreased visual acuity. d Postoperative T1-weighted MRI with contrast media reveals decreased size of cystic space; the remnant of the cystic wall was irradiated postoperatively
Two patients who suffered from amenorrhoea and partial hypopituitarism secondary to the intrasellar Rathke’s cleft cysts recovered nearly completely after the endoscopic surgery.
Arachnoid cyst
In 12 patients with arachnoid cysts (9 hemispherical arachnoid cysts and 3 suprasellar arachnoid cysts; Fig. 5), symptoms were relieved in 8 patients and improved in 4 patients, whereas the size of the cyst decreased in all patients. Postoperative neuroradiological evaluation confirmed the success of the endoscopic procedures. There was one subdural fluid collection but no neurological deficit during the follow-up period between 1992 and 2003.
a, b MRI scans show a suprasellar arachnoid cyst. c, d Patient underwent cysto-ventriculo-cisternostomy. Postoperative MRI studies reveal the collapsed cyst and a typical prepontine “flow-void ” phenomenon. e Upper, the endoscopic view shows the membrane of the arachnoid cyst. Middle, after endoscopic intervention the pituitary stalk and gland are seen. Lower, the membrane of Liliequist, which forms the inferior wall of the cyst toward the prepontine cistern, is fenestrated (cysto-cisternostomy)
Cystic neoplasm
The goal of a palliative cure was achieved in the 65 cystic neoplasm patients by Ommaya placement (35 cases) or postoperative radiation therapy after endoscopic biopsy of the tumour (Fig. 6). Four patients with cystic tumour lesions were followed using microsurgical resection of the solid tumour and radiotherapy. One exceptional patient developed a cystic lesion after radiation therapy for the intracranial metastatic tumour. The cyst was treated by placement of an Ommaya reservoir.
a, b A 62-year-old female presented with speech disturbance and dizziness. a MRI reveals a left parieto-occipital arachnoid cyst. After endoscopic biopsy of the cyst wall, an Ommaya reservoir was placed. b The 6-month control postoperative CT scan revealed a cyst of less than 5 mm and the patient was free of symptoms. c, d Multiple metastatic tumour in an 80-year-old patient. c Preoperative CT scan reveals a right intracerebellar cystic tumour. d Postoperative CT examination demonstrates a collapse of the cyst and the catheter of an Ommaya reservoir placed endoscopically into the cystic lesion
Discussion
Colloid cysts
In the past, either a transcortical–transventricular approach [4, 13, 14, 33] or a transcallosal approach [4, 5, 33, 42, 61] was deemed the gold standard in treatment of patients with colloid cysts. The former approach has often carried rather high operative morbidity and mortality rates [13, 65]. The latter, which may be an alternative nowadays, saves the cortex but can endanger bridging veins, the sinus and the pericallosal arteries, and may also traumatise the fornix. Gutierrez-Lara et al. [36] first performed freehand puncture and aspiration of a colloid cyst in 1975. Bosch et al. [9] performed the first stereotactic aspiration of a colloid cyst in 1978. However, for cysts with hard content, stereotactically guided aspiration often failed [52] and had the potential to injure the fornix and may cause bleeding from ependymal veins [58]. Either an endoscopic or a microsurgical procedure was required after stereotactic aspiration [53]. The long-term results of the aspiration technique also revealed a high recurrence rate [60].
During the past decade, endoscopic treatment of colloid cysts has gained increasing importance [19, 20, 22, 23, 38, 41, 58, 72, 92]. In 1963, Guiot and co-workers [35] reported the use of ventriculoscopy in a patient with a colloid cyst. In 1988, Auer et al. [6] operated on an intraventricular colloid cyst using a neodymium (yttrium-aluminium-garnet) laser. Many investigators underlined the effectiveness of neuroendoscopic approaches in the treatment of patients with colloid cysts [12, 22, 23, 58], even in long-term follow-up [1, 21, 41, 50]. Although Pollock and Huston [71] emphasised that colloid cysts have a relatively low risk of considerable growth, whether or not the cyst wall should be resected totally or some remnants left in place to reduce the surgical risk remains a matter of debate.
While the aim of endoscopic surgery for colloid cysts is the restoration of CSF blockage due to the mass at the foramina of Monro and the prevention of the recurrence, cyst evacuation as well as coagulation of the cyst wall seems to be a sufficiently effective alternative to microsurgical resection of the cyst [41]. Considering the postoperative evidence of our patients, which revealed no significant increase in the cyst size and an inconsistent decrease in ventricular size after long-term follow-up, we consider endoscopic surgery to be the treatment of choice in colloid cyst patients. However, the operating microscope should be kept ready to aid immediate microsurgical intervention in case of complications caused by the endoscopic procedure [29] or in a patient harbouring a calcified cyst when the content of the lesion cannot be aspirated [41].
Pineal cysts
Symptomatic pineal cysts are rare [27] and up to the present time, only 33 cases have been described [29, 38, 63, 66, 89]. A high degree of clinical suspicion is needed, because headaches may be the only feature. Although glial pineal cysts constitute a separate entity from pineal tumours and are common incidental findings on MRI [34, 59, 88], pineal parenchymal tumours may less frequently mimic the pineal cyst due to the cystic change of the tumour [15, 26, 67, 83].
The management of pineal cysts, as well as that of pineal tumours, has been the subject of debate in the last decade [10, 17, 43, 56]. Regarding pineal cysts, some authors advocate an open surgery technique [27, 64, 68], while others recommend stereotactic aspiration [56, 66, 75, 82]. Nowadays, the usage of endoscopy has been proposed as an alternative treatment. either by flexible [38, 86] or rigid endoscopes [29, 63], and the mortality and morbidity rates are reduced to zero [38, 63]. We used both stereotaxy [38] and neuronavigation [3] in selecting the best route for the introduction of the endoscope. This technique was found to be helpful in approaching the posterior part of the third ventricle when the foramen of Monro was narrow [3]. We agree with Michelsen and co-workers [63] that once the ventricles are reached, the direct view offered by the endoscope is most reliable.
The main indication for the operative treatment of symptomatic pineal cysts in our series is headache and imaging demonstrating enlargement of the lateral ventricles. We performed the endoscopic fenestration of cystic lesions and obtained biopsy samples using the direct view. Thus, obstructive hydrocephalus (due to the occlusion of the cerebral aqueduct), which occurred in one patient, could be resolved and verified by intraoperative ventriculography. If the flow of circulating CSF cannot be guaranteed, we agree with Gaab and Schroeder and Di Chirico et al. that third ventriculostomy may be another option for solving the problem of increased intracranial pressure [24, 28].
Cystic craniopharyngiomas and Rathke’s cleft cysts
Complete removal of a craniopharyngioma remains the treatment of first choice whenever possible. The main problem with craniopharyngioma surgery is recurrence. Even in patients who were operated on radically, the recurrence rate ranged between 7 and 24% [84, 90]. Total macroscopic removal, either using a transcranial or a transsphenoidal approach, cannot be achieved without morbidity and mortality [90]. Abdullah and Caemaert [2] and Hellwig et al. [38] have been reporting the endoscopic management of cystic craniopharyngiomas since 1995. For craniopharyngiomas that are cystic and located in or near the intraventricular area (Type D, E or F according to Yasargil et al.’s classification) [90], access via an endoscope is possible. Since craniopharyngiomas are usually subarachnoid tumours, they can be freed from the surrounding neurovascular structure [2].
Since 1995, we have applied endoscopic intervention in 10 patients, the cyst was punctured and evacuated to guarantee a sufficient inner decompression of the hypothalamus, the optic nerve and other surrounding sensitive structures. The cyst wall was vaporised and a partially solid part was taken for histological confirmation. It is our policy to treat cystic craniopharyngiomas by using endoscopic surgery in combination with microsurgery (Fig. 4a) or radiation therapy (Fig. 4b) if the patient has poor performance status. Particularly in cases of emergency such as optic nerve compression or deteriorated consciousness due to compression of the cystic craniopharyngioma, emergency endoscopic intervention may play an important role (Fig. 4a). In cases of tumour recurrence, microsurgical resection [38], irradiation [91], gamma knife radiosurgery [7, 16], and even application of a cysto-ventricular shunt or an Ommaya reservoir [37] are recommended.
Rathke’s pouch evaginates superiorly from the stomodeum of the 4-week-old human embryo. It is generally thought that persistence and enlargement of the residual cleft are responsible for the formation of Rathke’ s cleft cyst. Other explanations have suggested that the origin may be neuroepithelial cells [81], metaplastic anterior pituitary cells [74] or endodermal cells [44]. At autopsy, Shanklin found that a residual lumen between a portion of the anterior and posterior walls of the Rathke’s pouch persisted in 22 out of 100 normal pituitary glands [80]. Such cysts of Rathke’s cleft were recorded in 26% of routine autopsy series in four publications [8, 30, 62, 74]. Infrequently, these cysts enlarge enough to produce symptoms [40]; therefore, we would recommend endoscopic intervention in the symptomatic Rathke’s cleft cyst as an alternative treatment to either transsphenoidal [25, 49] or transcranial surgery [51].
Many reports also documented that it was sometimes difficult to determine the absolute pathological diagnosis of Rathke’s cyst due to the spectrum of histopathological characteristics of this cystic lesion [25, 77, 90]. This occurred in one of our patients and the neuropathologist had established the diagnosis as a Rathke’s cleft cyst but a craniopharyngioma could not be ruled out.
Arachnoid cysts
Arachnoid cysts occur throughout the neuraxis, and generally, no communication is demonstrable between the cyst and the subarachnoid space, although occasionally during surgery an arachnoid cyst is observed being filled through an apparent one-way valve [47, 78]. Arachnoid cysts may be asymptomatic throughout life and rarely they may spontaneously regress [87]. There is an ongoing discussion whether or not an asymptomatic arachnoid cyst should be operated on to prevent a hindrance to normal brain development and function [18, 55]. However, if the indication for surgery is questionable, intracranial pressure (ICP) monitoring should be performed to prove ICP elevation or pathologic pressure waves [28, 40]. In addition, electrophysiological studies and proper psychological testing may reveal subclinical neurological deficits in some of these patients [46].
Upcoming surgical options for the management of symptomatic arachnoid cysts include the endoscopic resection of the cyst wall with opening of the membranes; consequently, the communication between the cystic lesion and the ventricular CSF pathway would be established [45, 79]. Other surgical treatments are shunting, craniotomy with fenestration or resection of the cyst [18, 55, 57]. Shunting procedure may have led to shunt revisions [18]. Whereas craniotomy with the resection of the cyst may be difficult and associated with major surgical complications, simple fenestration of arachnoid cysts also poses the risk of re-closure of the fenestration site [18, 31, 70, 73].
Due to the relatively high success rate of 71–81% in other endoscopic series [11, 45, 48, 70, 79], and also in our series when compared with the microsurgical series outcome [18, 32], the authors would recommend the minimally invasive endoscopic approach as the treatment of choice in patients with arachnoid cysts. We believe that it is advisable to plan the operative approach before the endoscopic fenestration procedure, either by stereotaxy [40] or neuronavigation system [3, 85]. Although conclusions regarding the long-term outcome after endoscopic intervention in our patients cannot be reached, it is reasonable to perform a large stoma of the fenestrated cyst (10–15 mm in diameter) in order to obtain a good outcome. In cases of suprasellar arachnoid cysts, after inspection of the parasellar region, it is absolutely necessary to open the membrane of Liliequist (cysto-cisternostomy), which forms the inferior wall of the cyst towards the prepontine cistern, by using the basilar artery as a landmark (Fig. 5).
Cystic neoplasms
Endoscopic interventions for intracranial cystic neoplasms (anaplastic astrocytomas, glioblastomas, metastases) are performed less invasively to diminish the increased intracranial pressure and to establish the histopathological diagnosis. These cysts may also develop after radiation of postoperative brain metastasis or malignant glioma [54, 85]. Placement of an Ommaya reservoir can be an alternative treatment for this group of patients in cases of impaired performance status. The main goal of the treatment is to maintain the patient’s quality of life for the remaining small period. The decision to carry out a secondary microsurgical tumour resection should be made with consideration of the patient’s general status.
Conclusion
Endoscopic intervention for cystic intracranial lesions enables the resection of the cyst wall and optimal tissue examination. Via the same approach, the obstructed CSF pathways may be restored and, consequently, diminish the increased intracranial pressure. With the aid of stereotactic guidance or a neuronavigation system, access to the lesion can be gained rapidly and with high accuracy.
A definite therapy is the aim of endoscopic interventions for benign intracerebral cystic lesions (colloid cysts, pineal cysts and arachnoid cysts). It is our policy to treat cystic craniopharyngiomas using endoscopic surgery in combination with microsurgery or radiation therapy if the patient has poor performance status. Particularly in emergency cases such as optic nerve compression or deteriorated consciousness due to compression caused by a cystic craniopharyngioma, emergency endoscopic intervention may play an important role. Endoscopic interventions for intracranial cystic neoplasms are palliative and are performed less invasively to diminish the increased intracranial pressure and to establish histopathological diagnosis. Combined treatments, i.e. chemotherapy, irradiation and placement of an Ommaya reservoir, are alternative treatments for this group of patients. The main goal of the treatment for cystic neoplasms is to maintain patient’s quality of life.
References
Abdou MS, Cohen AR (1998) Endoscopic treatment of colloid cysts of the third ventricle: technical note and review of the literature. J Neurosurg 89:1062–1068
Abdullah J, Caemaert J (1995) Endoscopic management of craniopharyngiomas: a review of 3 cases. Minim Invasive Neurosurg 38:79–84
Alberti O, Riegel T, Hellwig D, Bertalanffy H (2001) Frameless navigation and endoscopy. J Neurosurg 2001:541–543
Antunes JL, Louis KM, Ganti SR (1980) Colloid cysts of the third ventricle. Neurosurgery 7:450–455
Apuzzo MLJ, Chikovani OK, Gott PS, Teng EL, Zee CS, Giannotta SL, Weiss MH (1982) Transcallosal, interfornicial approaches for lesions affecting the third ventricle: surgical considerations and consequences. Neurosurgery 10:547–554
Auer LM, Holzer P, Ascher PW, Heppner F (1988) Endoscopic neurosurgery. Acta Neurochir (Wien) 90:1–14
Barajas MA, Ramirez-Guzman G, Rodriguez-Vazquez C, Toledo-Buenrostro V, Velasquez-Santana H, del Robles RV, Cuevas-Solorzano A, Rodriguez-Hernandez G (2002) Multimodal management of craniopharyngiomas: neuroendoscopy, microsurgery, and radiosurgery. J Neurosurg 97 [Suppl 5]:607–609
Bayoumi ML (1948) Rathke’s cleft and its cysts. Edinb Med J 55:745–749
Bosch DA, Rähn T, Backlund EO (1978) Treatment of colloid cysts of the third ventricle by stereotactic aspiration. Surg Neurol 9:15–18
Bruce JN, Stein BM (1995) Surgical management of pineal region tumors. Acta Neurochir (Wien) 134:130–135
Caemaert J, Abdullah J, Calliauw L, Carton D, Dhooge C, van Coster R (1992) Endoscopic treatment of suprasellar arachnoid cysts. Acta Neurochir 119:68–73
Caemaert J, Abdullah J, Calliauw L (1994) Endoscopic diagnosis and treatment of para- and intra-ventricular cystic lesions. Acta Neurochir Suppl (Wien) 61:69–75
Camacho A, Abernathey CD, Kelly PJ, Laws ER Jr (1989) Colloid cysts: experience with the management of 84 cases since the introduction of computed tomography. Neurosurgery 24:693–700
Chen TC, Krieger M, Hinton DR, Zee CS, Apuzzo LJ (1997) The colloid cyst. In: Apuzzo MLJ (ed) Surgery of the third ventricle, 2nd edn. Lippincott Williams & Wilkins, Philadelphia, pp 1071–1131
Chiechi MV, Smirniotopoulos JG, Mena H (1995) Pineal parenchymal tumors: CT and MR features. J Comput Assist Tomogr 19:509–517
Chiou SM, Lunsford LD, Niranjan A, Kondziolka D, Flickinger JC (2001) Stereotactic radiosurgery of residual or recurrent craniopharyngioma, after surgery, with or without radiation therapy. Neurooncology 3:159–166
Cho BK, Wang KC, Nam DH, Kim DG, Jung HW, Kim HJ, Han DH, Choi KS (1998) Pineal tumors: experience with 48 cases over 10 years. Childs Nerv Syst 14:53–58
Ciricillo SF, Cogen PH, Harsh GR, Edwards MS (1991) Intracranial arachnoid cysts in children: a comparison of the effects of fenestration and shunting. J Neurosurg 74:230–235
Cohen AR (1993) Endoscopic ventricular surgery. Pediatr Neurosurg 19:127–134
Cohen AR (1994) Ventriculoscopic surgery. Clin Neurosurg 41:546–562
Decq P, Le Guerinel C, Brugieres P, Djindjian M, Silva D, Keravel Y, Melon E, Nguyen JP (1998) Endoscopic management of colloid cysts. Neurosurgery 42:1288–1296
Deinsberger W, Böker DK, Bothe HW, Samii M (1994) Stereotactic endoscopic treatment of colloid cysts of the third ventricle. Acta Neurochir (Wien) 131:260–264
Deinsberger W, Böker DK, Samii M (1994) Flexible endoscopes in treatment of colloid cysts of the third ventricle. Minim Invasive Neurosurg 37:12–16
Di Chirico A, Di Rocco F, Velardi F (2001) Spontaneous regression of a symptomatic pineal cyst after endoscopic third-ventriculostomy. Childs Nerv Syst 17:42–46
El Mahdy WE, Powell M (1998) Transsphenoidal management of 28 symptomatic Rathke’s cleft cysts, with special reference to visual and hormonal recovery. Neurosurgery 42:7–16
Engel U, Gottschalk S, Niehaus L, Lehmann R, May C, Vogel S, Janisch W (2000) Cystic lesions of the pineal region—MRI and pathology. Neuroradiology 42:399–402
Fain JS, Tomlinson FH, Scheithauer BW, Parisi JE, Fletcher GP, Kelly PJ, Miller GM (1994) Symptomatic glial cysts of the pineal gland. J Neurosurg 80:454–460
Gaab MR, Schroeder HWS (1998) Arachnoid cysts. In: King W, Frazee J, DeSalles A (eds) Endoscopy of the central and peripheral nervous system. Thieme, New York, pp 136–147
Gaab MR, Schroeder HWS (1998) Neuroendoscopic approach to intraventricular lesions. J Neurosurg 88:496–505
Gillman T (1940) The incidence of ciliated epithelium and mucous cells in the normal Bantu pituitary. S Afr Med Sci 5:30–40
Go KG (1995) The diagnosis and treatment of intracranial arachnoid cysts. Neurosurg Q 5:187–204
Go KG, Houthoff HJ, Hartsuiker J, Blaauw EH, Havinga P (1986) Fluid secretion in arachnoid cysts as clue to cerebrospinal fluid absorption at the arachnoid granulation. J Neurosurg 65:642–648
Gökalp HZ, Yüceer N, Arasil E, Erdogan A, Dincer C, Baskaya M (1996) Colloid cyst of the third ventricle: evaluation of 28 cases of colloid cyst of the third ventricle operated on by transcortical/transventricular (25 cases) and transcallosal/transventricular (3 cases) approaches. Acta Neurochir (Wien) 138:45–49
Golzarian J, Balériaux D, Bank WO, Matos C, Flament-Durand J (1993) Pineal cyst: normal or pathological? Neuroradiology 35:251–253
Guiot G, Rougerie J, Fourestier M (1963) Intracranial endoscopic exploration [in French]. Presse Med 71:1225–1228
Gutierrez-Lara F, Patino R, Hakim S (1975) Treatment of tumors of the third ventricle: a new and simple technique. Surg Neurol 3:323–325
Gutin PH, Klemme WM, Lagger RL, MacRay AR, Pitts LH, Hosobuchi Y (1980) Management of unresectable cystic craniopharyngioma by aspiration through an Ommaya reservoir drainage system. J Neurosurg 52:36–40
Hellwig D, Bauer BL, Hellwig EL (1995) Stereotactic endoscopic interventions in cystic brain lesions. Acta Neurochir (Suppl) 64:59–63
Hellwig D, Haag R, Bartel V, Riegel T, Eggers F, Becker R, Bertalanffy H (1999) Application of new electro-surgical devices and probes in endoscopic neurosurgery. Neurosurg Res 21:67–72
Hellwig D, Bauer BL, Riegel T, Schmideck HH, Sweet WH (2000) Surgical management of intracranial arachnoid, suprasellar, and Rathke’s cleft cysts. In: Schmidek HH, Sweet WH (eds) Operative neurosurgical techniques: indications, methods, and results, vol 1, 4th edn. Saunders, Philadelphia, pp 513–532
Hellwig D, Bauer BL, Schulte M, Gatscher S, Riegel T, Bertalanffy H (2003) Neuroendoscopic treatment for colloid cysts of the third ventricle: the experience of a decade. Neurosurgery 52:525–533
Hernesniemi J, Levio S (1996) Management outcome in third ventricular colloid cysts in a defined population: a series of 40 patients treated mainly by transcallosal microsurgery. Surg Neurol 45:2–14
Herrmann HD, Winkler D, Westphal M (1992) Treatment of tumors of the pineal region and posterior part of the 3rd ventricle. Acta Neurochir (Wien) 116:137–146
Hirano A, Ghatak NR, Wisoff HS, Zimmerman HM (1971) An epithelial cyst of the spinal cord: an electron microscopic study. Acta Neuropathol 18:214–223
Hopf NJ, Perneczky A (1998) Endoscopic neurosurgery and endoscope-assisted microneurosurgery for the treatment of intracranial cysts. Neurosurgery 43:1330–1336
Hopf NJ, Resch KDM, Ringel K, Perneczky A (1998) Endoscopic management of intracranial arachnoid cysts. In: Hellwig D, Bauer BL (eds) Minimally invasive techniques for neurosurgery. Springer, Berlin Heidelberg New York, pp 111–119
Hornig GW, Zervas NT (1992) Slit defect of the diaphragma sellae with valve effect: observation of a “slit valve”. Neurosurgery 30:265–267
Jones RFC, Warnock TH, Nayanar V, Gupta JM (1989) Suprasellar arachnoid cysts: management by cyst wall resection. Neurosurgery 25:554–561
Kasperbauer JL, Orvidas LJ, Atkinson JL, Abboud CF (2002) Rathke cleft cyst: diagnostic and therapeutic considerations. Laryngoscope 112:1836–1839
King WA, Ullman JS, Frazee JF, Post KD, Bergsneider M (1999) Endoscopic resection of colloid cysts: surgical considerations using the rigid endoscope. Neurosurgery 44:1103–1111
Kleinschmidt-Demasters BK, Lilllehei KO, Stears JC (1995) The pathologic, surgical, and MR spectrum of Rathke cleft cysts. Surg Neurol 44:19–26
Kondzioka D, Lunsford LD (1991) Stereotactic management of colloid cysts: factors predicting success. J Neurosurg 75:45–51
Kondzioka D, Lunsford LD (1994) Stereotactic techniques for colloid cysts: role of aspiration, endoscopy, and microsurgery. Acta Neurochir Suppl 61:76–78
Korinth MC, Weinzierl MR, Krings T, Gilbach JM (2001) Occurrence and therapy of space-occupying cystic lesions after brain tumor surgery. Zentralbl Neurochir 62:87–92
Krawchenko J, Collins GH (1979) Pathology of an arachnoid cyst: case report. J Neurosurg 50:224–228
Kreth FW, Schatz CR, Pagenstecher A, Faist M, Volk B, Ostertag CB (1996) Stereotactic management of lesions of the pineal region. Neurosurgery 39:280–289
Lange M, Oeckler R, Beck OJ (1990) Surgical treatment of patients with midline arachnoid cysts. Neurosurg Rev 3:35–39
Lewis AI, Crone KR, Taha J, van Loveren HR, Yeh HS, Tew JM Jr (1994) Surgical resection of third ventricle colloid cysts. Preliminary results comparing transcallosal microsurgery with endoscopy. J Neurosurg 81:174–178
Mamourian AC, Towfighi J (1986) Pineal cysts: MR imaging. Am J Neuroradiol 7:1081–1086
Mathiesen T, Grane P, Lindquist C, von Holst H (1993) High recurrence rate following aspiration of colloid cysts in the third ventricle. J Neurosurg 78:748–752
Mathiesen T, Grane P, Lindgren L, Lindquist C (1997) Third ventricle colloid cyst: a consecutive 12-year series. J Neurosurg 86:5–12
McGrath P (1971) Cysts of sella and pharyngeal hypophyses. Pathology 3:123–131
Michelsen G, Benoit Y, Baert E, Meire F, Caemaert J (2002) Symptomatic pineal cysts: clinical manifestation and management. Acta Neurochir (Wien) 144:233–242
Miyatake S, Kikuchi H, Yamasaki T, Terashima T, Asahi M, Asato R, Higuchi K, Nakashima Y (1992) Glial cyst of the pineal gland with characteristic computed tomography, magnetic resonance imaging, and pathological findings: report of two cases. Surg Neurol 37:293–299
Morita A, Kelly PJ (1993) Resection of intraventricular tumors via a computer-assisted volumetric stereotactic approach. Neurosurgery 32:920–927
Musolino A, Cambria S, Rizzo G, Cambria M (1993) Symptomatic cysts of the pineal gland: stereotactic diagnosis and treatment of two cases and review of the literature. Neurosurgery 32:315–320
Nakamura M, Saeki N, Iwadate Y, Sunami K, Osato K, Yamaura A (2000) Neuroradiological characteristics of pineocytoma and pineoblastoma. Neuroradiology 42:509–514
Oeckler R, Feiden W (1991) Benign symptomatic lesions of the pineal gland. Report of seven cases treated surgically. Acta Neurochir (Wien) 108:40–44
Paladino J, Rotim K, Heinrich Z (1998) Neuroendoscopic fenestration of arachnoid cysts. Minim Invasive Neurosurg 41:137–140
Pierre-Kahn A, Capelle L, Brauner R, Sainte-Rose C, Reiner D, Rappaport R, Hirsch JF (1990) Presentation and management of suprasellar arachnoid cysts. J Neurosurg 73:355–359
Pollock BE, Huston J III (1999) Natural history of asymptomatic colloid cysts of the third ventricle. J Neurosurg 91:364–369
Powell MP, Torrens MJ, Thomson JL, Hogan JG (1983) Isodense colloid cysts of the third ventricle: a diagnostic and therapeutic problem resolved by ventriculoscopy. Neurosurgery 13:234–237
Rappaport ZH (1993) Suprasellar arachnoid cysts: options in operative management. Acta Neurochir (Wien) 122:71–75
Rasmussen AT (1929) Ciliated epithelium and mucous-secreting cells in the human hypophysis. Anat Rec 41:273–283
Regis J, Bouillot P, Rouby-Volot F, Figarella-Branger D, Dufour H, Peragut JC (1996) Les biopsies stéréotactiques des tumeurs de la région pinéale. Réflexions sur leur risque et leur rendement ȧ propos de 370 cas. Neurochirurgie 39:907–912
Riegel T, Freudenstein D, Alberti O, Duffner F, Hellwig D, Bartel V, Bertalanffy H (2002) Novel multipurpose bipolar instruments for endoscopic neurosurgery. Neurosurgery 51:270–274
Russell DS, Rubinstein LJ (1971) Pathology of tumors of the nervous system, 3rd edn. Williams & Wilkins, Baltimore
Schroeder HW, Gaab MR (1997) Endoscopic observation of a slit-valve mechanism in a suprasellar prepontine arachnoid cyst: case report. Neurosurgery 40:198–200
Schroeder HW, Gaab MR, Niendorf WR (1996) Neuroendoscopic approach to arachnoid cysts. J Neurosurg 85:293–298
Shanklin WM (1951) The incidence and distribution of cilia in the human pituitary with a description of microfollicular cysts derived from Rathke’s cleft. Acta Anat (Basel) 11:361–382
Shuangshoti S, Netsky MG, Nashold BS (1970) Epithelial cysts related to sella turcica: proposed origin from neuroepithelium. Arch Pathol 90:444–450
Stern JD, Ross DA (1993) Stereotactic management of benign pineal cysts: report of two cases. Neurosurgery 32:310–314
Sugiyama K, Arita K, Okamura T, Yamasaki F, Kajiwara Y, Ueda H, Kurisu K (2002) Detection of a pineoblastoma with large central cyst in a young child. Childs Nerv Syst 18:157–160
Sweet WH (1980) Recurrent craniopharyngiomas: therapeutic alternatives. Clin Neurosurg 27:206–229
Tirakotai W, Riegel T, Sure U, Bozinov O, Hellwig D, Bertalanffy H (2004) Clinical application of neuro-navigation in a series of burr-hole procedures. Zentralbl Neurochir 65:57–64
Turtz AR, Hughes WB, Goldman HW (1995) Endoscopic treatment of a symptomatic pineal cyst: technical case report. Neurosurgery 37:1013–1014
Weber R, Voit T, Lumenta C, Lenard HG (1991) Spontaneous regression of a temporal arachnoid cyst. Childs Nerv Syst 7:414–415
Welton PL, Reicher MA, Kellerhouse LE, Ott KH (1988) MR of benign pineal cyst. Am J Neuroradiol 9:612
Wisoff JH, Epstein F (1992) Surgical management of symptomatic pineal cysts. J Neurosurg 77:896–900
Yasargil MG, Curcid M, Kis M, Siegenthaler G, Teddy PJ, Roth P (1990) Total removal of craniopharyngioma. Approaches and long-term results in 144 patients. J Neurosurg 73:3–11
Yu X, Liu Z, Li S (2000) Combined treatment with stereotactic intracavitary irradiation and gamma knife surgery for craniopharyngioma. Stereotact Funct Neurosurg 75:117–122
Zamorano L, Chavantes C, Dujovny M, Malik G, Ausman J (1992) Stereotactic endoscopic interventions in cystic and intraventricular brain lesions. Acta Neurochir Suppl 54:69–76
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tirakotai, W., Schulte, D.M., Bauer, B.L. et al. Neuroendoscopic surgery of intracranial cysts in adults. Childs Nerv Syst 20, 842–851 (2004). https://doi.org/10.1007/s00381-004-0941-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-004-0941-3