Abstract
Methods
Simultaneous shunt placement and neural tube repair are described and compared with a concomitant series of patients with delayed shunting. Twenty-eight patients with a myelomeningocele underwent closure of neural tube defects at our Institution from 1998 to 2001. Eleven patients (Group 1) had concomitant surgery performed after birth. Group 2 (7 out of 28) included patients without hydrocephalus at birth, in Group 3 (4 out of 28) the children did not develop hydrocephalus, and Group 4 (6 out of 28) patients were born outside our hospital and referred for surgical care after birth.
Discussion
Simultaneous insertion of shunt and correction of a myelomeningocele do not pose an additional risk to the child and do have some advantages, facilitating healing of the back without CSF leakage and protecting the brain from the effects of progressive ventricular dilatation. Patients with a myelomeningocele born outside the hospital are prone to infectious complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelomeningocele is the most complex congenital abnormality compatible with long-term survival. This congenital malformation has been aggressively treated [13] and at least 75% of children born with open spina bifida can be expected to reach their early adult years [2]. The majority of children (80–95%) affected by a myelomeningocele will sooner or later need surgical treatment for associated hydrocephalus.
Many authors have addressed concerns about simultaneous repair of a myelomeningocele and shunt insertion, most of which are related to fears of an increased rate of infection after manipulation of the dorsal sac [4, 6]. Various risk factors for cerebrospinal fluid (CSF) shunt infection have been indicated in the literature, including the etiology of the hydrocephalus, the age of the patient, the surgical procedure, and postoperative CFS leakage [9].
It has been reported that age at shunt insertion may influence the shunt infection rate [11], and it has been argued that because ventricular shunt insertion reverses CSF flow it allows fluid from the lumbar region to travel to the ventricles. Thus, shunt insertion performed within a week of closure of the spinal lesion could increase the risk of shunt infection. On the other hand, other authors did not observe differences between patients with a shunt placed in the 1st month of life, in the first 6 months or after 6 months [3, 17].
However, in hydrocephalic children with a myelomeningocele, insertion of the shunt will provide good healing of the back, will avoid a second operation and will protect the brain from additional lesions that could otherwise result from progressive ventricular dilatation and delayed shunt.
Since our policy is to perform simultaneous shunt placement and myelomeningocele repair and the literature is contradictory, we reviewed our experience concerning this subject.
Patients and methods
We analyzed all patients who underwent myelomeningocele repair at our institution during the period from January 1998 to March 2001.
We detected 28 cases that were subsequently divided into four groups (Table 1). Group 1 consisted of 11 patients who were born with a myelomeningocele and hydrocephalus at our center and who underwent combined correction on the 1st (4 out of 28), 2nd (2 out of 28), 3rd (3 out of 28) or 4th (2 out of 28) day of life. All were then followed up for more than 6 months, and 7 were followed up for more than 1 year. Group 2 consisted of 7 patients born at our center without hydrocephalus at birth, who had their shunts inserted at various times after the initial correction of their myelomeningocele (ranging from 12 days to 6 months). Group 3 consisted of 4 patients born at our center who did not develop hydrocephalus.
The 6 patients in Group 4 who were born outside our hospital underwent surgery between 9 and 40 days after birth. Four patients were already infected on arrival: they required antibiotics, correction of the back lesion, and placement of an EVD. The remaining 2 required no intervention.
After birth, all children were thoroughly examined for clinical status. Hydrocephalus was evaluated by head ultrasound and considered hypertensive when, besides the presence of an enlarged head circumference, the ventricles were dilated and resistive indices measured in the anterior cerebral artery were above 0.8, with a pathologic response to fontanel compression.
Whenever possible, surgery was performed as soon as the child was born. When indicated, a ventriculoperitoneal (V-P) shunt was inserted first. The child was placed in the supine position with the dorsal dressing in place and well padded. The dressing over the abdomen was removed or displaced laterally if in continuity with the dorsum. The surgical field was then prepped and draped as usual for V-P shunt surgery. Next, the incisions were protected and the child was turned to the prone position. All surgical drapes were replaced and again the dorsal region prepped and draped as usual for this type of surgery. Correction of the myelomeningocele was then performed and at the end of surgery the child was placed in a lateral or prone position for the subsequent days. All sutures were absorbable and dressings were usually changed daily.
Observations and results
In Group 1 there was 1 case of infection (shunt inserted on day 4) and 1 case of delayed wound healing; 5 shunt revisions were performed in 3 patients (without infection). In Group 2 there were no cases of infection, and only 1 of delayed wound healing. One of the patients in Group 3 died of clinical complications, and the other 3 had no infection. Of the patients in Group 4 who were already infected (4 cases) upon arrival, 1 subsequently died and the remaining 3 had late shunt insertion; 2 children were not operated on.
Discussion and conclusions
When is the best time for shunt insertion after myelomeningocele repair? This is an intriguing question involving several concerns. Some factors are very important, such as infection, intellectual development, and shunt malfunction [10].
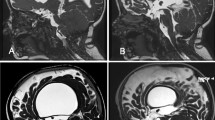
The optimal management of patients with a myelomeningocele and hydrocephalus is facilitated by a constant review of the patients with the aid of the sonogram and CT scan [12].
The timing for cerebrospinal fluid shunt insertion in these neonates with hydrocephalus in association with a myelomeningocele remains controversial. Shunt insertion depends on the severity and rate of progression of hydrocephalus; nevertheless, 25% of infants with a myelomeningocele show hydrocephalus at birth, and some authors advocate that a shunt be placed in these children at the time of back closure [5].
Pang has raised several theoretical concerns about the risk inherent in shunting and closing the back simultaneously [15]. The main factor is the general susceptibility to infection because of the compromised immune function of these newborns.
It has been reported that the age at shunt insertion may influence the shunt infection rate [3, 11], and it has been argued that shunt insertion reverses cerebrospinal fluid flow and allows fluid from the lumbar region to travel to the ventricles facilitating infection. Some authors believe that shunt insertion performed within a week of repair of the myelomeningocele could increase the risk of shunt infection. In 1996, Caldarelli et al. did not find any difference between patient age at the time of myelomeningocele repair or the order in which the spinal surgery and the initial shunting procedure were carried out in terms of the influence on the rate of shunt function [3].
In other studies [4], neonates who underwent simultaneous shunt placement and myelomeningocele repair were compared with neonates treated with conventional sequential myelomeningocele repairs requiring a second separate procedure for shunt placement. Infants operated upon simultaneously experienced no increase in morbidity or mortality and appeared to benefit substantially [6].
Some authors [8, 14] have suggested that simultaneous myelomeningocele repair and V-P shunt insertion reduce hospital stay and back wound morbidity in those patients with evidence of hydrocephalus at birth, without an inordinate increase in shunt-related complications.
Advocates of this approach stress the merits of administering only one anesthetic: reduced incidence of cerebrospinal fluid leaks from the operated site and a shorter hospital stay with the resulting cost-effectiveness. Alternatively, serial ventricular taps or an external ventricular drain may be used initially and shunting may be delayed for several days [15].
Parent and McMillan assessed the complication rate for shunts inserted at the time of myelomeningocele repair and those inserted at a later date in a separate procedure. They reported that delayed insertion of a V-P shunt, or that contemporaneous with the repair of a myelomeningocele, did not increase significantly the risks of shunt infection or shunt malfunction within the 1st year of life [16].
In our study, the rate of infection was low in the group born at our institution who underwent simultaneous shunt placement and myelomeningocele repair. Only one patient showed ventriculitis after shunt insertion and this patient was operated on 4 days after birth.
Children with a myelomeningocele born at other institutions underwent correction of their myelomeningocele and EVD installation when infection was detected. Only when the CSF infection was cleared was shunt surgery indicated.
Our policy is shunting and closing the back simultaneously. The first step is to protect the lesion after birth with local dressings and prophylactic antibiotics. After pediatric clinical evaluation and brain sonography with color-Doppler (unpublished data), the child undergoes concomitant surgery. First of all we insert the shunt and then turn the child and close the myelomeningocele.
The requirements are that the child be born at the same hospital and the lesion adequately dressed. Indication for a shunt is based on brain sonography after the fontanel compression test [19, 20].
Brain sonography can be used to monitor ventricular dilatation in hydrocephalic children and functional tests can be helpful to evaluate the cerebral autoregulation dynamics in infants with hydrocephalus and intracranial hypertension [1, 7, 18, 20].
In conclusion, simultaneous shunt insertion and correction of a myelomeningocele does not carry any additional risk for the child and does have some advantages, providing healing of the back without CSF leakage and protection of the brain from the effects of progressive ventricular dilatation. However, the back lesion must be carefully protected between birth and the time of surgery. Children with a myelomeningocele who are born outside the hospital and referred for treatment elsewhere are prone to major complications since they have not received adequate care for the exposed dorsal lesion since birth.
References
Aaslid R, Markwalder T, Nornes H (1982) Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg 57:769–774
Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA (2001) Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg 34:114–120
Caldarelli M, Di Rocco C, La Marca F (1996) Shunt complications in the first postoperative year in children with meningomyelocele. Childs Nerv Syst 12:748–754
Chadduck WM, Reding DL (1988) Experience with simultaneous ventriculo-peritoneal shunt placement and myelomeningocele repair. J Pediatr Surg 23:913–916
Dias M (2000) Myelomeningocele. In: Choux M, Di Rocco C, Hockley A, Walker M (eds) Pediatric neurosurgery. Churchill Livingstone, London, pp 34–59
Epstein N, Rosenthal E, Zito AD, Osipoff MJ (1985) Shunt placement and myelomeningocele repair: simultaneous vs sequential shunting. Review of 12 cases. Childs Nerv Syst 1:145–147
Hill A, Volpe JJ (1982) Decrease in pulsatile flow in the anterior cerebral arteries in infantile hydrocephalus. Pediatrics 69:4–7
Hubballah MY, Hoffman HJ (1987) Early repair of myelomeningocele and simultaneous insertion of ventriculoperitoneal shunt: technique and results. Neurosurgery 20:21–23
Kulkarni AV, Drake JM, Lamberti-Pasculli M (2001) Cerebrospinal fluid shunt infection: a prospective study of risk factors. J Neurosurg 94:195–201
Liptak GS, McDonald JV (1986) Ventriculoperitoneal shunts in children: factors affecting shunt survival. Pediatr Neurosci 12:289–293
Liptak GS, Masiulis BS, McDonald JV (1985) Ventricular shunt survival in children with neural tube defects. Acta Neurochir (Wien) 74:113–117
Liptak GS, Bolander HM, Langworthy K (2001) Screening for ventricular shunt function in children with hydrocephalus secondary to meningomyelocele. Pediatr Neurosurg 34:281–285
McLone DG (1998) Care of the neonate with a myelomeningocele. Neurosurg Clin North Am 9:111–120
Miller PD, Pollack IF, Pang D, Albright AL (1996) Comparison of simultaneous versus delayed ventriculoperitoneal shunt insertion in children undergoing myelomeningocele repair. J Child Neurol 11:370–372
Pang D (1995) Surgical complications of open spinal dysraphism. Neurosurg Clin North Am 6:243–257
Parent AD, McMillan T (1995) Contemporaneous shunting with repair of myelomeningocele. Pediatr Neurosurg 22:132–135
Piatt JH, Carlson CV (1993) A search for determinants of cerebrospinal fluid shunt survival: retrospective analysis of a 14-year institutional experience. Pediatr Neurosurg 19:233–242
Seibert JJ, McCowan TC, Chadduck WM, Adametz JR, Glasier CM, Wiliamson SL, Taylor BJ, Leithiser Jr RE, McConnell JR, Stansell CA, Rodgers AB, Corbit SL (1989) Duplex pulsed Doppler ultrasound versus intracranial pressure in the neonate: clinical and experimental studies. Radiology 171:155–159
Taylor GA (1992) Effect of scanning pressure on intracranial hemodynamics during transfontanellar duplex Doppler examinations. Radiology 185:763–766
Taylor GA, Madsen JR (1996) Neonatal hydrocephalus: hemodynamic response to fontanelle compression—correlation with intracranial pressure and need for shunt placement. Radiology 201:685–689
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Machado, H.R., Santos de Oliveira, R. Simultaneous repair of myelomeningocele and shunt insertion. Childs Nerv Syst 20, 107–109 (2004). https://doi.org/10.1007/s00381-003-0853-7
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-003-0853-7