Abstract
Case report
A 13-year-old male with an 11-year history of a seizure disorder presented with recent onset raised intracranial pressure symptoms and no obvious phakomatosis. CT revealed a heterogeneous, frontal, intra-axial, densely enhancing, solid lesion with intense perilesional oedema and mass effect. Total microsurgical excision resulted in cure. Histopathological examination showed characteristic Antoni A and B areas and occasional Verocay bodies consistent with the diagnosis of an intraparenchymal schwannoma.
Discussion
The authors present a very rare, entirely solid manifestation of this highly uncommon lesion seen mostly in young adults and children with symptoms suggestive of raised intracranial pressure and associated seizure disorders. The possible developmental origins are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracranial schwannomas in the adult population account for 8% of all primary brain tumours, most of which are acoustic neuromas [15]. By contrast, they account for only 2% of posterior fossa tumours in children [1].
Intraparenchymal schwannomas are exceedingly rare and those within the neuraxis are far more likely to occur in an intraspinal location than in an intracranial one. To the best of our knowledge, only 52 cases have been reported so far in literature [1, 2, 4, 6, 7, 10, 11, 16, 18, 19, 20]. Of these, 8 cases have emanated from our institute [16]. Although typically benign, 4 cases of malignant change have been documented thus far [17].
This report describes a lesion in a boy proven on subsequent biopsy to be a schwannoma.
Case report
A 13-year-old boy was admitted to the All India Institute of Medical Sciences (New Delhi) under the services of the Department of Neurosurgery in April 2001 with complaints of progressively worsening left focal faciobrachial clonic motor seizure activity since the age of 2 years with secondary generalization and postictal ipsilateral hemiparesis, and the absence of any aura, prodrome, interictal headache, vomiting, squint, diplopia, visual deterioration, personality change, worsening scholastic activity, febrile seizures, or birth trauma. The patient had received an empirical 3-month course of anti-tubercular therapy on the basis of CT scan findings at a peripheral centre but instead deteriorated and presented with progressive headache and vomiting for a 15-day period prior to admission. The family history did not indicate epilepsy, neurofibromatosis or a contact with tuberculosis.
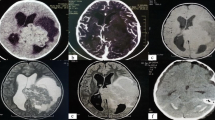
Examination revealed an alert intelligent boy with no neurocutaneous markers, 6/6 visual acuity in both eyes, florid papilloedema, an upper motor neuron type of left facial nerve paresis and minimal weakness of the left upper limb. Tone was increased in all limbs with clonic reflexes but a flexor plantar response bilaterally. Routine haematological and biochemical parameters were within normal limits. The chest skiagram was normal and the contrast enhanced computerized tomogram (CT) described a heterogeneous mass in the right frontal parasagittal parenchyma, which was lobulated and of mixed density, ranging from iso- to hypodense (Fig. 1). Enhancement was irregular but intense in the isodense areas and scanty in the hypodense areas as seen on the non-contrast films. There was extensive perilesional oedema with mass effect and compression of the ipsilateral ventricles.
The patient had two seizures in the preoperative period, which were treated appropriately. The patient underwent a right medial frontal osteoplastic craniotomy and total microsurgical excision of the lesion, which was fleshy, highly vascular, with a well-defined plane of cleavage, gritty in areas, well suckable with no definable dural attachment, located subcortically and separated medially from the falx by a thin rim of cortex.
The postoperative period was uneventful and the patient was afebrile, oriented, ambulant and bereft of fresh deficits at discharge on the fourth postoperative day.
Haematoxylin and eosin staining (Fig. 2) revealed compact fascicles of fusiform cells with elongated nuclei and indistinct cytoplasmic borders arranged in a palisading pattern (Antoni A areas) admixed with haphazardly oriented loosely arranged cells in a myxoid matrix (Antoni B areas). Occasional Verocay bodies were also sighted confirming the diagnosis of a schwannoma. Silver impregnation stains showed a rich pericellular reticulin network in the Antoni A areas.
At the 6-month follow-up, the patient was leading a normal life, was seizure free, and had resumed going to school. A postoperative contrast enhanced CT scan revealed no residual lesion and resolution of the perilesional oedema at 3 months.
Discussion
Intraparenchymal schwannomas are rare tumours but have several characteristic features, which serve to classify them as separate identities as opposed to their far more common vestibular counterparts. The majority occurs in children and young adults with no female predilection. Frim et al., in their review of cases, found that 13 out of 33 cases were in patients less than 15 years old [10]. The most common signs and symptoms include headache, seizures and focal deficits.
Radiologically, peritumoral oedema with or without gliosis in either a superficial or a deep periventricular location is believed to be characteristic, as was manifest in this case report [20]. Although cyst formation and calcification are also believed to be characteristic [20], the lesion did not present with either. The patient in this report had such extensive perilesional oedema that the radiologists offered a differential diagnosis of a meningioma versus a malignant lesion or a tuberculoma. The cause of oedema is uncertain and unlike meningiomas in which vascular endothelial growth factor (VEGF) messenger RNA expression has been documented, the same has not been established in these cases. Chronic oedema may be due to white matter degeneration and gliosis, both of which are frequently associated with this entity [9]. Interestingly, a review of the literature reveals two studies in which cysts were not documented in 16 out of 35 cases by Zagardo et al. [20] and in 45.5% by Tsuiki et al. [18]. Moreover, a frontal lobar location apparently predisposes to this non-cystic presentation as corroborated by reports by Auer et al. [2] and Deogaonkar et al. [6]. However, a report by Tsuiki et al. regarding two frontal lobar intraparenchymal schwannomas included one with a cyst documented both by MRI and intraoperatively [18].
Calcification was also lacking in this lesion on the CT as well as on histopathology. Calcification has only been documented in 6 cases in a recent review [20]. The origin of intracerebral schwannomas has been the source of much controversy. The most popular hypothesis argues that these tumours arise from the proliferation of Schwann cells in the perivascular perineural nerve plexii, which may be either developmental (supported by the early age of presentation) or due to chronic disease [14].
Differentiation from multipotential mesenchymal elements within the CNS is another proposed theory [8].
Russel and Rubenstein, to denote hamartomatous remains of Schwann cells and related reticulin fibres within the neuraxis, which may serve as the precursors for this tumour, have proposed the term schwannosis [15].
Another view, based on the chance findings of DeMyer et al. of aberrant nerve fibres penetrating the medulla oblongata through the long circumferential vessels, holds that these myelinated fibres with their Schwann cells may get incorporated into the substance of the brain as a hamartomatous malformation. These then form the nidus for the growth of an intraparenchymal schwannoma in the posterior fossa [5].
The differential diagnosis of these lesions includes tuberculomas, which are possibly the commonest lesions in this part of South Asia, but those in the supratentorial compartment are often multiple, located at the grey-white junction and hyperdense on the non-contrast CT scan with ring enhancement. They uncommonly calcify and in the non-miliary form rarely generate vasogenic oedema [3]. Meningiomas were also considered in the possible radiological differential but these too are uncommon in this age group, account for only about 2% of all tumours and are strongly associated with neurofibromatosis type 2. These generally have a well-defined dural attachment (with the exception of Sylvian fissure meningiomas), a 50% incidence of calcification and a 12% incidence of cyst formation [3]. Pilocytic astrocytomas are the commonest solid-cystic tumours in the supratentorial compartment but they greatly lack associated perilesional oedema [12]. Pleomorphic xanthoastrocytomas form a similar subgroup of essentially benign supratentorial lesions found again in this very age group, which have similar MRI findings suggesting cyst formation, heterogeneity and associated mild to moderate oedema. Calcification, however, is rarely seen and these lesions are generally located superficially in the cortex with leptomeningeal involvement and a firm dural attachment [13]. Gangliogliomas are also extremely similar in appearance but have a propensity to occur in the temporal lobes.
Conclusion
Intraparenchymal schwannomas offer a rare differential diagnosis of intra-axial, heterogeneous, superficial, cortical or deep periventricular lesions with cyst formation, calcification, and extensive peritumoral oedema or gliosis, in children or young adults, with headache, seizures and/or focal deficits. We have presented in this report a rare manifestation of this lesion with a frontal lobar, solid, heterogeneous, enhancing, intra-axial, solid mass with extensive perilesional oedema lacking calcification or cyst formation. Surgical results after microsurgical excision are favourable in the extreme.
References
Allcutt DA, Hoffman HJ, Isla A et al (1991) Acoustic schwannomas in children. Neurosurgery 29:14–19
Auer R, Budney J, Drake C et al (1982) Frontal lobe perivascular schwannoma. J Neurosurg 56:154–157
Barkovich AJ (2000) Pediatric neuroimaging, 3rd edn. Lippincott Williams and Wilkins, Philadelphia, pp 537–540; 739
Cervoni L, Caruso R, Gagliardi FM (1998) Intracerebral schwannoma. Case report. J Neurosurg Sci 42:57–59
DeMyer W (1965) Aberrant peripheral nerve fibres in the medulla oblongata of man. J Neurol Neurosurg Psychiatry 28:121–123
Deogaonkar M, Goel A, Nagpal RD et al (1994) Intraparenchymal schwannoma of the frontal lobe. J Postgrad Med 40:218–219
Erongun U, Ozkal E, Acar O et al (1996) Intracerebral schwannoma: case report and review. Neurosurg Rev 19:269–274
Feigin I, Ogata J (1971) Schwann cells and peripheral myelin within human central nervous tissues; the mesenchymal character of Schwann cells. J Neuropathol Exp Neurol 30:603–612
Feigen I, Popoff N (1963) Neuropathological changes late in cerebral edema: the relationship to trauma, hypertensive disease and Binswanger’s encephalopathy. J Neuropathol Exp Neurol 22:500–511
Frim DM, Ogilvy CS, Vonsattal JP et al (1992) Is intracerebral schwannoma a developmental tumor of children and young adults? Pediatr Neurosurg 18:190–194
Lee SH, Yoo H, Lee JH et al (1999) Multiple intraparenchymal schwannomas in the cerebellum, brainstem, and cervical spinal cord. Acta Neurochir (Wien) 141:779–780
Lee YY, Van Tassel P, Bruner JM et al (1989) Juvenile pilocytic astrocytomas: CT and MR characteristics. Am J Neuroradiol 10:363–370
Lipper MH, Eberhard DA, Phillips CD et al (1993) Pleomorphic xanthoastrocytoma; a distinctive astroglial tumor: neuroradiologic and pathologic features. Am J Neuroradiol 14:1397–1404
Riggs HE, Clary WU (1957) A case of intramedullary sheath cell tumor of the spinal cord. Consideration of vascular nerves as a source of origin. J Neuropathol Exp Neurol 16:332–336
Russel DS, Rubinstein LJ (1977) Pathology of tumours of the nervous system, 4th edn. Arnold, London, pp 51–52; 372–379
Sharma MC, Karak AK, Gaikwad SB et al (1996) Intracranial intraparenchymal schwannomas: a series of eight cases. J Neurol Neurosurg Psychiatry 60:200–203
Sharma S, Abbott RI, Zagzag D (1998) Malignant intracerebral nerve sheath tumor: a case report and review of the literature. Cancer 82: 545–552
Tsuiki H, Kuratsu J, Ishimaru Y, Nakahara T et al (1997) Intracranial intraparenchymal schwannoma: report of three cases. Acta Neurochir (Wien) 139:756–760
Weiner HL, Zagzag D, Babu R et al (1993) Schwannoma of the fourth ventricle presenting with hemifacial spasm. A report of two cases. J Neurooncol 15:37–43
Zagardo MT, Castellani RJ, Rees JH et al (1998) Radiologic and pathologic findings of intracerebral schwannoma. J Neuroradiol 19:1290–1293
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vaishya, S., Sharma, M.S. Frontal intraparenchymal schwannoma: an unusual presentation. Childs Nerv Syst 20, 247–250 (2004). https://doi.org/10.1007/s00381-003-0852-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-003-0852-8