Abstract
Tolvaptan has been gradually spread to use as a potent diuretic for congestive heart failure in the limited country. However, the response to this aquaretic drug still is unpredictable. A total of 92 patients urgently hospitalized due to congestive heart failure and treated with tolvaptan in addition to standard treatment was retrospectively analyzed. Responder of tolvaptan treatment was defined as a patient with peak negative fluid balance greater than 500 mL/day, and clinical profiles were compared between 76 responders and 16 non-responders. Responders started to increase daily urine volume (UV) from Day 1 through Day 3. In contrast, non-responders showed no significant increase in daily UV from the baseline up to Day 5. Time between admission and tolvaptan administration was shorter in responders, even without statistical significance (3.3 vs. 4.6 days, p = 0.053). Multivariate analysis revealed that blood urea nitrogen (BUN) [cutoff: 34 mg/dL, odds ratio (OR) 9.0, 95% confidence interval (CI) 1.42–57.3, p < 0.01] and plasma renin activity (PRA) (cutoff: 4.7 ng/mL/h, OR 6.1, 95% CI 1.01–36.4, p < 0.01) at baseline were independent predictors for tolvaptan responsiveness. It suggests that renal perfusion may affect tolvaptan-induced UV. Finally, durations of stay in intensive care unit and total hospitalization were significantly shorter in responders (median: 6.0 vs. 13.0 days, p = 0.022; 15.0 vs. 25.0 days, p = 0.016, respectively). Responders of tolvaptan have lower BUN and renin activity at baseline, and shorten hospitalization period.
Trial Registration
The study was registered at University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) with the identifier UMIN000023594. https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000024988
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congestive heart failure (CHF) is a major cause of hospitalization in cardiology units and is often caused by systemic volume overload. Although substantial evidence of medical treatments for CHF has been accumulated, it is not uncommon to encounter patients who are refractory to existing therapies. Thus, diverse approaches are necessary to treat CHF. Loop diuretics are clinically useful to reduce excessive intravascular volume. However, the responses to these classical diuretics are sometimes insufficient in patients with more advanced stages of the disease [1]. Furthermore, the administration of high-dose loop diuretics induces several adverse events, including renal impairment and hyponatremia, through the activation of the renin–angiotensin–aldosterone system (RAAS). These issues ultimately lead to poor long-term survival [2].
Arginine vasopressin (AVP) levels are elevated in CHF patients and may lead to water retention and hyponatremia by activating V2 receptors [3]. Tolvaptan is a selective AVP V2 receptor antagonist that increases the excretion of free water (aquaresis) in CHF patients. In Japan, tolvaptan is covered by health insurance for CHF patients and has gradually become widely used in these patients [4,5,6,7]. Despite this recent usage, the diuretic effect of this aquaretic drug in patients with CHF cannot be accurately predicted. With the above in mind, we aimed to clarify the characteristics of responders to tolvaptan among CHF patients in a real clinical setting.
Methods
Study design
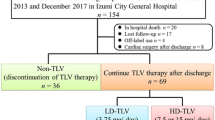
This was a retrospective observational study of patients who were urgently hospitalized due to worsening CHF and were treated with tolvaptan in a single cardiovascular center between June 2011 and March 2014. Patients were diagnosed with CHF by their physicians according to the Framingham heart failure diagnostic criteria. However, patients who were already receiving daily tolvaptan before admission or undergoing maintenance dialysis were excluded. The study protocols conformed to the ethical guidelines of the 1975 Declaration of Helsinki. The ethics committee of our institution approved the study protocol. Written informed consent only for data use from medical records was obtained from all patients before study enrolment. Finally, 92 patients were retrospectively analyzed.
Treatment protocols and definitions
All patients were administered at least one diuretic at the initiation of tolvaptan treatment. Urine volume (UV) and fluid balance (FB) were evaluated before and up to 4 days after the initiation of tolvaptan treatment.
The tolvaptan initial dose was arbitrarily decided by the attending physician and dose was titrated over the following days at the discretion of the attending physician. Once hypernatremia occurred, tolvaptan was discontinued. The final dose of tolvaptan was principally decreased to 3.75 mg after the intensive treatment period. Patients were divided into responders and non-responders depending on their FB. A responder was defined as a patient with a peak value of negative daily FB > 500 mL within the 4 days after the start of tolvaptan treatment. Based on the finding that the median daily FB in all patients peaked at − 558 mL/day on day 2 (Fig. 1), we set a cutoff value of response to tolvaptan at a peak negative FB of approximately > 500 mL/day within 4 days after the initiation of tolvaptan treatment.
Worsening renal function (WRF) was defined as a serum creatinine (Cr) elevation of 0.3 mg/dL above the baseline during the 4 days after the start of tolvaptan treatment. [1,2,3] Hypertension was defined as systolic blood pressure (BP) > 140 mmHg, diastolic BP > 90 mmHg, or ongoing treatment using antihypertensive medicine against previously diagnosed hypertension; diabetes mellitus was defined by a fasting plasma blood glucose level of ≥ 126 mg/dL on two separate occasions or ≥ 200 mg/dL at any time or the use of anti-hyperglycemic agents including insulin. Dyslipidemia was diagnosed according to low-density lipoprotein cholesterol level ≥ 140 mg/dL, high-density lipoprotein cholesterol level < 40 mg/dL, triglyceride level ≥ 150 mg/dL, or the use of anti-lipidemic medicines. Chronic kidney disease was determined based on estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2. Peripheral artery disease (PAD) was determined by an ankle-brachial index ≤ 0.80, angiographically defined peripheral arterial stenosis ≥ 75%, or history of endovascular treatment for ischemic limbs.
Data collection
Baseline patient characteristics, comorbidities, etiology of heart failure, duration from admission to tolvaptan administration, initial doses of tolvaptan and other medications, 4-day total doses of furosemide after the initiation of tolvaptan, and durations of intensive care unit (ICU) and total hospital stays were recorded. All information about past illness was collected from medical records. Vital signs, including physical findings, BP, and UV, and lab data, including Cr and blood urea nitrogen (BUN) for renal function, were evaluated for 5 days after the start of tolvaptan treatment. Plasma renin activity (PRA), plasma aldosterone concentration, brain natriuretic peptide (BNP), and catecholamines (neurohumoral factors) were evaluated for 5 days after the start of tolvaptan treatment. All blood samples for the analysis of baseline parameters were collected immediately before tolvaptan administration or early on the morning of the day of tolvaptan initiation.
Statistical analysis
Values are expressed as means ± SDs and percentiles in tables, means ± SEs in figures, and means alone in the text unless otherwise noted. Data concerning hospital and ICU stays are expressed as medians and interquartile ranges (25–75th percentile). Figures 1 and 4 are presented as boxes and whiskers with maximum and minimum values. The bottom and top of the box are the first and third quartiles, and the band inside the box is the median. The ends of the whiskers represent the minimum and maximums values of all data. The independent Student’s t test or the non-parametric equivalent Mann–Whitney U test was used to compare continuous parameters between responders and non-responders. Fisher’s exact test or the Chi square test was used to evaluate categorical variables. Comparisons among consecutive samples from the two groups were evaluated by multiple t tests using the Holm–Sidak method. The Wilcoxon matched-pairs signed-rank test was used for comparisons of consecutive samples with baseline. Multivariate analysis was performed to evaluate the independent contribution of clinical and physiological variables to tolvaptan response by forward stepwise logistic regression analysis. The variables with statistical significance in the univariate analysis were tested. In multivariate analysis, we adjusted the duration of hospital stay for serum creatinine and sodium concentration at admission. The area under the receiver operating characteristic (ROC) curve (AUC) was plotted to determine cutoff points to convert continuous parameters to categorical variables. A two-sided p value < 0.05 was considered statistically significant.
Results
Baseline clinical backgrounds and medications
Patient characteristics are shown in Table 1. Patients in this study were typically in the late 70 s and half were men. They experienced diverse comorbidities; in particular, chronic kidney disease was highly prevalent in both groups. There was no significant difference in any parameters except those relating to renal function, such as Cr, BUN, and PRA, between the two groups. The etiologies of heart failure are shown in Supplemental Table 1; the prevalence was similar in both groups. Both groups had comparable echocardiographic parameters (Supplemental Table 2). The rate of pre-hospital oral furosemide use was approximately 60% in both groups (responders vs. non-responders 61% vs. 56%, p = 0.75). Angiotensin converting enzyme inhibitors/angiotensin II receptor blockers and beta-blockers were similarly administered between the groups. Other pre-hospital oral medications were also similarly administered and 4-day total doses of furosemide were not significantly different between the groups. However, aldosterone antagonists were significantly more frequently administered in responders (82 vs. 50%, p < 0.01) (Table 2). Compared to the CHF patients enrolled in one of the largest representative observational studies in Japan, these two study populations had comparable etiologies of CHF, renal functions, BNP levels and pre-hospital medications (Supplemental Table 3). In contrast, the major difference between the studies was NYHA classification at the admission. Also, patients in the current study frequently included female patients with older age, lower systolic BP and preserved cardiac function, compared to ATTEND registry.
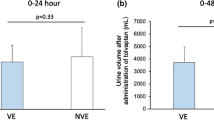
Water excretion
The patients’ UV and FB values are shown in Fig. 2. The UV of responders started to increase from day 1 (1191–1897 mL/day, p < 0.01, Fig. 2a). This increase was greater than 150% of baseline. This significant increase persisted over the 3 days after tolvaptan initiation. Responders achieved negative FB during 4 days after tolvaptan initiation. In contrast, non-responders did not show any significant change in UV from baseline and never achieved negative FB at any time point. UV and FB showed significant differences between the groups (day 3: 1987 vs. 1032 mL/day, p < 0.001; − 684 vs. + 216 mL/day, p < 0.001, respectively, Fig. 2). Cutoff values of UV and FB at day 1 in responders and non-responders were 1080 mL/day and − 208 mL/day, respectively (Supplemental Figure 1). Total 4-day UV and 4-day negative FB were greater in responders (Supplemental Figure 2).
Predictors of response to tolvaptan
Tolvaptan administration
All patients were treated with natriuretics and if the efficacy of these drugs was not enough to restore the patient’s status, we considered tolvaptan. Total administered duration and initial dose of tolvaptan were not statistically different between the groups (5.9 vs. 7.2 days, p = 0.26; 7.8 vs. 7.7 mg, p = 0.75, respectively, Supplemental Figure 3A, B). With regard to the time between the patient’s admission and the initial administration of tolvaptan, there was a tendency for tolvaptan to be administered earlier in responders (3.3 vs. 4.6 days, p = 0.053, Supplemental Figure 3C). Additionally, among the entire study population, an earlier start of tolvaptan was associated with a shorter duration of hospital stay (r = 0.43, p < 0.001, Supplemental Figure 3D).
Renal function
Responders had significantly better baseline renal function (Cr: 1.19 vs. 2.16 mg/dL, p < 0.01; eGFR: 52.9 vs. 34.1 mL/min/1.73 m2, p = 0.012; Cystatin C: 1.60 vs. 2.07 mg/L; BUN: 26.7 vs. 42.0 mg/dL, p < 0.01, Table 1, Fig. 3a, b). In responders, BUN/Cr ratio significantly decreased between day 0 and day 5; however, there was no significant difference between the groups (Fig. 3c). Tolvaptan administration further worsened renal function in non-responders (Cr: 0.6 vs. 23.0%, p < 0.01; BUN: − 3.9 vs. 15.9%, p = 0.045, Fig. 3, Supplemental Figure 4A, B). As a result, the incidence of WRF in responders was significantly lower than that in non-responders (11 vs. 63%, p < 0.01, Supplemental Figure 4C).
Renal function and neurohumoral factors Serum creatinine (a), BUN (b), BUN/creatinine ratio (c), catecholamines [adrenaline (d), noradrenaline (e) and dopamine (f)], BNP (g), plasma aldosterone concentration (h), and plasma renin activity (i) before and 5 days after tolvaptan administration. BNP indicates brain natriuretic peptide; BUN blood urea nitrogen; Cr serum creatinine; Resp. responders. *p < 0.05 compared to non-responders. #p < 0.05 compared to baseline in responders. $p < 0.05 compared to baseline in non-responders
Neurohumoral factors
In terms of neurohumoral factors, both groups had similar baseline values and achieved substantial reductions for all kinds of catecholamines (Table 1, Fig. 3d–f). Furthermore, the kinetics of BNP and aldosterone concentration were similar between the groups (Table 1, Fig. 3g, h). Only responders achieved significant reductions in these parameters. However, PRA at baseline was significantly lower in responders (3.5 vs. 12.3 ng/mL/h, p < 0.01, Table 1, Fig. 3i). Additionally, baseline PRA value was associated with eGFR (r = − 0.35, p = 0.003, Supplemental Figure 5) rather than with BUN or BUN/creatinine ratio (r = 0.19, p = 0.038; r = 0.28, p = 0.020, respectively). PRA level was not significantly different between patients with and without aldosterone antagonist administration at baseline (1.25 [0.63–7.15] vs. 1.20 [0.40–7.70] ng/mL/h, p = 0.76).
Medications
Patients who did not receive pre-treatment with furosemide represented 39 and 44% of responders and non-responders, respectively. Furthermore, total doses of 4-day furosemide were not significantly different between the groups (141 vs. 228 mg, p = 0.93, Table 2). Therefore, treatment with loop diuretics did not seem to significantly affect response to tolvaptan. However, the prevalence of in-hospital use of aldosterone antagonists was significantly higher in responders (82 vs. 50%, p < 0.01, Table 2).
Sodium concentration
Sodium concentration during the 4 days after tolvaptan initiation is shown in Supplemental Figure 6. Responders showed significantly higher baseline, minimum, and maximum sodium concentrations (day 0: 137 vs. 135 mEq/L; minimum: 135 vs. 132 mEq/L, p < 0.01; maximum: 144 vs. 139 mEq/L, p < 0.01). At day 5, the significant difference between the groups disappeared. Hypernatremia, defined as a sodium concentration ≥ 150 mEq/L, occurred in six patients (8%) in responders and none in non-responders. However, these patients did not experience any neurological disorders related to hypernatremia.
Multivariate analysis
A multivariate logistic regression model used while considering other covariates including Cr, BUN, sodium, and PRA at baseline, and in-hospital administration of aldosterone antagonist as significant parameters (determined by univariate analysis) is summarized in Table 3. ROC analysis showed that the cutoff values for these covariates were 0.79, 34.0 mg/dL, 139 mEq/L, and 4.7 ng/ml/h, respectively. The only variables related to tolvaptan responsiveness were BUN and PRA level (odds ratio [OR] 9.01, 95% confidence interval [CI] 1.42–57.3; OR 6.06, 95% CI 1.01–36.4, respectively).
In-hospital prognosis
Responders had significantly shorter stays in the ICU and hospital (6.0 [3.5–7.5] vs. 13.0 [6.0–15.0] days, p = 0.022; 15.0 [11.0–23.0] vs. 25.0 [18.0–41.0] days, p = 0.016, respectively, Fig. 4a, b). There was a significant trend toward shorter duration of hospital stay in responders, even after adjusting for baseline creatinine and sodium concentration (cutoff: 16.0 days, OR 7.15, 95% CI 1.23–41.4). However, the in-hospital mortality rate was not significantly different between the groups (9.2 vs. 6.3%, p = 0.70, Fig. 4c).
Discussion
Summary of the principal findings of the study
First, this study showed that urine response to tolvaptan was associated with hospital stay in patients with CHF. Furthermore, urine response on the first day of tolvaptan administration predicted response. The cutoff values of response in UV and FB at day 1 were 1080 and − 208 mL/day, respectively. Second, multivariate analysis revealed that BUN and PRA at baseline were independent predictors of urine response to tolvaptan. BUN and PRA reflect renal perfusion; therefore, patients with maintained renal perfusion were likely to respond to tolvaptan.
Rationale of response to tolvaptan
There are diverse parameters proposed for determining response to tolvaptan; however, to date, a gold standard has not been determined. Response largely depends on patient age, gender, stage of heart failure, etiologies, and medications. Therefore, it may be hard to fit one criterion for response to other populations. When response to tolvaptan was set as a UV increase > 0 mL/day after tolvaptan use, baseline urine osmolality > 358 mOsm/L predicted response [8]. However, this cutoff level in urine response discriminated only two patients (2%) as non-responders in the population assessed in the present study. Such differences may be largely due to patient selection. Diuretic response also varies among hospitals; the clinical backgrounds of patients are vastly different between university hospitals and community hospitals. However, a large proportion of CHF patients are admitted to community hospitals. Therefore, it is necessary to understand the response to diuretics in the real clinical setting. ATTEND registry that was the largest registry of CHF patients in Japan recruited substantial numbers of university hospitals [9]. Therefore, even it may have represented real world clinical settings, it was not consisted of homogenous population, and still enclosed considerable differences between hospitals in terms of patient backgrounds.
The median value of peak negative FB was 500 mL/day in the entire population; thus, we set this value as a cutoff point between the responder and non-responder groups. This peak appeared at 2 days after tolvaptan initiation. The infusion volume varies among patients; therefore, a cutoff value of peak negative FB may be a reasonable method for determining response.
Predictors of tolvaptan response
Multivariate analysis revealed that PRA and BUN were independent predictors of tolvaptan response. The renal collecting duct, where tolvaptan acts, is the final part of the nephron; therefore, substantial primitive urine should be delivered down to the collecting duct for sufficient tolvaptan response. All parameters with statistical significance according to univariate analysis, including Cr, BUN, sodium concentration, and PRA, reflect renal function. However, multivariate analysis excluded Cr and sodium as predictors of tolvaptan response. This suggests that renal hypoperfusion affects tolvaptan response, rather than renal parenchymal damage.
Non-responders received higher doses of furosemide during 4 days after the initiation of tolvaptan, but this difference was not statistically significant. A different diuretic response was already observed between the groups on the first day of tolvaptan administration. Poor response to tolvaptan resulted in a higher total dose of furosemide for 4 days and may lead to further worsening of renal function in non-responders. High-dose loop diuretics activate neurohumoral factors, including the sympathetic nerve system (SNS), RAAS, and vasopressin. High PRA level may represent renal hypoperfusion profiles and relate to high BUN concentration [10]. Furthermore, renal hypoperfusion can decrease reactivity to diuretics, and poorer diuretic response is associated with worse long-term clinical prognoses in CHF patients [11, 12]. In this study, baseline PRA was significantly associated with not only BUN or BUN/creatinine ratio but also eGFR, suggesting that response to tolvaptan depends on renal blood perfusion in addition to renal parenchymal status.
The present study showed that the degree of water excretion in patients with acute CHF who were treated with tolvaptan did not affect in-hospital prognosis. Therefore, further investigations involving longer observation periods are warranted to determine the relationship between response to tolvaptan and long-term clinical outcomes. In contrast, good response to tolvaptan could shorten hospital stays. The median length of hospital stay in tolvaptan responders was 15 days in this study, 6 days shorter than the median duration in large Japanese heart failure registries [9, 13]. Baseline profiles were comparable between responders and non-responders except for parameters representative of renal function. There was a difference in renal blood perfusion in particular. In this study, there were no significant correlations between renal function and other profiles that may affect renal blood flow such as age, left ventricular systolic function, and systemic blood pressure. Diverse factors can lead to the deterioration of renal function; however, renal hypoperfusion is the most typical phenotype of non-responders to tolvaptan. This is a possible reason why renal function was the only predictor of response to tolvaptan in this study. Consistent with our results, previous reports described that worse renal function was a significant predictor of poor response to tolvaptan [14].
Response was reflected by UV and FB on the day of tolvaptan initiation. This quick prediction is clinically important. In Japan, in particular, it has been hard for clinical interventions to make a significant impact during the hospitalization period because insufficient back-up facilities are available for the care of CHF patients after hospital discharge. Therefore, when patients are categorized as poor responders to tolvaptan, intensive and multidisciplinary treatment should be considered. A recently published report suggested that tolvaptan use at an early stage of acute CHF is associated with shorter hospital stays [15]. In the present study, the early initiation of tolvaptan therapy was associated with shorter hospitalization duration. The time between admission and tolvaptan administration might be related to lower doses of furosemide, resulting in maintained renal perfusion via the avoidance of arterial underfilling. Additionally, responders received beta-blockers or aldosterone antagonists more frequently than non-responders, without statistical significance. These drugs may exert favorable effects on diuretic response to tolvaptan by suppressing SNS and RAAS activation in CHF patients [16].
Sodium kinetics
Hyponatremia is a furosemide-resistant factor. In this condition, residual free water in the interstitial space is prevented from being freely drawn back into circulation because blood osmolality is kept low by natriuretics. Therefore, the furosemide dose tends to be increased in such patients, resulting in renal hypoperfusion through arterial underfilling. Additionally, the response to loop diuretics depends on the time course and the amount of drug reaching the urine and the pharmacodynamics of response in the ascending limb of loop of Henle. Renal blood flow in CHF patients with hyponatremia is often reduced and the response to diuretic is progressively attenuated [17].
Patients with hyponatremia are generally thought to be good candidates for tolvaptan. Tolvaptan preserves or increases serum sodium concentration by sodium channel-independent diuresis through the vasopressin V2 receptor. However, in this study, responders had higher serum sodium concentration at baseline. In other words, low sodium concentration at baseline was not a predictor of better outcomes in terms of UV. One of the possible reasons for this is that hyponatremia represents impaired renal function that is predominantly found in non-responders. Convoluted tubule damage due to chronic kidney disease decreases sodium reuptake.
Conversely, we experienced six patients with hypernatremia, defined as a sodium concentration of ≥ 150 mEq/L (only in responders). This figure represented 6.5% of the entire population. Prior reports have demonstrated that hypernatremia occurs in 0–19% of cases. [18,19,20] Tolvaptan was discontinued in patients who developed hypernatremia; however, we have never experienced a patient with neurological deficit related to hypernatremia, and all such patients were discharged with comparable durations of hospital stay.
Study limitations
First, this was a retrospective study in a single center and included a limited number of patients. Second, we regarded peak values of negative daily FB > 500 mL after the start of tolvaptan as a marker of tolvaptan response. This cutoff value was determined based on the findings in this specific study population and may not be applicable to the global CHF population. Third, in this study, patient-selection bias exists for tolvaptan use; well-treated CHF patients with furosemide alone could not be administered tolvaptan. It may have affected the results in this study. Fourth, the initial dose of tolvaptan was arbitrarily decided by the attending physician. Thus, 12% of patients were started at 3.75 or 15 mg/day of tolvaptan. Additionally, one patient who initially received 15 mg/day was followed up with an increased dose of up to 30 mg/day of tolvaptan. The analysis was, therefore, prone to titration bias. Fifth, 40% of the study population did not receive loop diuretics before hospitalization, suggesting that they were ‘de novo’ CHF patients. This heterogeneity may affect the response to tolvaptan observed in this study. Sixth, the frequent use of carperitide as a vasodilator may also affect the response to tolvaptan. Seventh, all laboratory data, including neurohumoral factors, were obtained on the day of tolvaptan initiation; therefore, differences in admission time may have affected the results. Finally, urine osmolality was not tested and may have differed between responders and non-responders.
Conclusions
Responders to tolvaptan had better renal function and lower renin activity at baseline and achieved shorter hospitalization periods. Rapid urine response may be a predictor of response to tolvaptan.
Change history
12 December 2017
In the original publication of the article, the values of blood urea nitrogen (BUN) and plasma renin activity (PRA) have been published incorrectly and the corrected values are as follows.
References
Peacock WF, Costanzo MR, De Marco T, Lopatin M, Wynne J, Mills RM, Emerman CL (2009) Impact of intravenous loop diuretics on outcomes of patients hospitalized with acute decompensated heart failure: insights from the ADHERE registry. Cardiology 113:12–19
Hasselblad V, Gattis Stough W, Shah MR, Lokhnygina Y, O’Connor CM, Califf RM, Adams KF Jr (2007) Relation between dose of loop diuretics and outcomes in a heart failure population: results of the ESCAPE trial. Eur J Heart Fail 9:1064–1069
Lee CR, Watkins ML, Patterson JH, Gattis W, O’Connor CM, Gheorghiade M, Adams KF Jr (2003) Vasopressin: a new target for the treatment of heart failure. Am Heart J 146:9–18
Gheorghiade M, Konstam MA, Burnett JC Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C (2007) Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST Clinical Status Trials. JAMA 297:1332–1343
Costello-Boerrigter LC, Smith WB, Boerrigter G, Ouyang J, Zimmer CA, Orlandi C, Burnett JC Jr (2006) Vasopressin-2-receptor antagonism augments water excretion without changes in renal hemodynamics or sodium and potassium excretion in human heart failure. Am J Physiol Renal Physiol 290:F273–F278
Uemura Y, Shibata R, Takemoto K, Uchikawa T, Koyasu M, Ishikawa S, Mitsuda T, Miura A, Imai R, Iwamiya S, Ozaki Y, Kato T, Miura T, Watarai M, Murohara T (2016) Clinical benefit of tolvaptan in patients with acute decompensated heart failure and chronic kidney disease. Heart Vessels 31:1643–1649
Hanatani A, Shibata A, Kitada R, Iwata S, Matsumura Y, Doi A, Sugioka K, Takagi M, Yoshiyama M (2017) Administration of tolvaptan with reduction of loop diuretics ameliorates congestion with improving renal dysfunction. Heart Vessels 32:287–294
Imamura T, Kinugawa K, Shiga T, Kato N, Muraoka H, Minatsuki S, Inaba T, Maki H, Hatano M, Yao A, Kyo S, Nagai R (2013) Novel criteria of urine osmolality effectively predict response to tolvaptan in decompensated heart failure patients–association between non-responders and chronic kidney disease. Circ J 77:397–404
Sato N, Kajimoto K, Keida T, Mizuno M, Minami Y, Yumino D, Asai K, Murai K, Muanakata R, Aokage T, Sakata Y, Mizuno K, Takano T (2013) Clinical features and outcome in hospitalized heart failure in Japan (from the ATTEND Registry). Circ J 77:944–951
Mentz RJ, Stevens SR, DeVore AD, Lala A, Vader JM, AbouEzzeddine OF, Khazanie P, Redfield MM, Stevenson LW, O’Connor CM, Goldsmith SR, Bart BA, Anstrom KJ, Hernandez AF, Braunwald E, Felker GM (2015) Decongestion strategies and renin-angiotensin-aldosterone system activation in acute heart failure. JACC Heart Fail 3:97–107
Valente MA, Voors AA, Damman K, Van Veldhuisen DJ, Massie BM, O’Connor CM, Metra M, Ponikowski P, Teerlink JR, Cotter G, Davison B, Cleland JG, Givertz MM, Bloomfield DM, Fiuzat M, Dittrich HC, Hillege HL (2014) Diuretic response in acute heart failure: clinical characteristics and prognostic significance. Eur Heart J 35:1284–1293
Ter Maaten JM, Dunning AM, Valente MA, Damman K, Ezekowitz JA, Califf RM, Starling RC, van der Meer P, O’Connor CM, Schulte PJ, Testani JM, Hernandez AF, Tang WH, Voors AA (2015) Diuretic response in acute heart failure-an analysis from ASCEND-HF. Am Heart J 170:313–321
Tsuchihashi-Makaya M, Hamaguchi S, Kinugawa S, Yokota T, Goto D, Yokoshiki H, Kato N, Takeshita A, Tsutsui H (2009) Characteristics and outcomes of hospitalized patients with heart failure and reduced vs preserved ejection fraction. Report from the Japanese cardiac registry of heart failure in cardiology (JCARE-CARD). Circ J 73:1893–1900
Imamura T, Kinugawa K, Fujino T, Inaba T, Maki H, Hatano M, Yao A, Komuro I (2014) Increased urine aquaporin-2 relative to plasma arginine vasopressin is a novel marker of response to tolvaptan in patients with decompensated heart failure. Circ J 78:2240–2249
Matsukawa R, Kubota T, Okabe M, Yamamoto Y (2015) Early use of V2 receptor antagonists is associated with a shorter hospital stay and reduction in in-hospital death in patients with decompensated heart failure. Heart Vessels 31:1650–1658
Felker GM, Mentz RJ (2012) Diuretics and ultrafiltration in acute decompensated heart failure. J Am Coll Cardiol 59:2145–2153
Paterna S, Di Pasquale P, Parrinello G, Amato P, Cardinale A, Follone G, Giubilato A, Licata G (2000) Effects of high-dose furosemide and small-volume hypertonic saline solution infusion in comparison with a high dose of furosemide as a bolus, in refractory congestive heart failure. Eur J Heart Fail 2:305–313
Watanabe K, Dohi K, Sugimoto T, Yamada T, Sato Y, Ichikawa K, Sugiura E, Kumagai N, Nakamori S, Nakajima H, Hoshino K, Machida H, Okamoto S, Onishi K, Nakamura M, Nobori T, Ito M (2012) Short-term effects of low-dose tolvaptan on hemodynamic parameters in patients with chronic heart failure. J Cardiol 60:462–469
Kinugawa K, Sato N, Inomata T, Shimakawa T, Iwatake N, Mizuguchi K (2014) Efcacy and safety of tolvaptan in heart failure patients with volume overload—an interim result of post-marketing surveillance in Japan. Circ J 78:844–852
Hirai K, Shimomura T, Moriwaki H, Ishii H, Shimoshikiryo T, Tsuji D, Inoue K, Kadoiri T, Itoh K (2016) Risk factors for hypernatremia in patients with short- and long-term tolvaptan treatment. Eur J Clin Pharmacol 72:1177–1183
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was not financially supported from any company, grant or fund, and all authors have no conflict of interest.
Additional information
The original version of this article was revised: The values of blood urea nitrogen (BUN) and plasma renin activity (PRA) have been corrected in this article.
A correction to this article is available online at https://doi.org/10.1007/s00380-017-1102-4.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kogure, T., Jujo, K., Hamada, K. et al. Good response to tolvaptan shortens hospitalization in patients with congestive heart failure. Heart Vessels 33, 374–383 (2018). https://doi.org/10.1007/s00380-017-1072-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-1072-6