Abstract
The purpose of this study was to evaluate the outcome of nonagenarians after transcatheter aortic valve replacement (TAVR) from the OBSERVANT study and to pool the results of the literature on this topic. Aortic stenosis is the most common acquired valvular heart disease in the Western countries, and its prevalence is linked to the phenomenon of population aging. TAVR can be considered as a wise approach to treat nonagenarians, but data on its safety and effectiveness are scarce. Data on 80 patients aged >90 years who underwent TAVR from OBSERVANT study were analyzed. A systematic review and meta-analysis of published data were performed. Thirty-day mortality in the OBSERVANT series was 6.3 %. None of these patients experienced stroke. Permanent pacemaker implantation was necessary in 20 % of patients. Paravalvular regurgitation was observed in 57.5 %. Survival at 1, 2, and 3 years was 79.6, 71.9, and 61.5 %. Ten series provided data on 1227 nonagenarians who underwent TAVR. Pooled 30-day mortality rate was 7.1 %, stroke 2.8 %, vascular access complication 8.8 %, and permanent pacemaker implantation 10.6 %. Paravalvular regurgitation was observed in 60.1 % of patients. Pooled 1-, 2-, and 3-year survival rates were 79.2, 68.2, and 55.6 %. Transapical TAVR was associated with a significantly higher risk of early mortality compared with transfemoral TAVR. The results of OBSERVANT study and aggregate data meta-analysis suggest that in nonagenarians, TAVR is associated with low postoperative morbidity and excellent intermediate survival. Transapical TAVR in these very elderly is associated with high postoperative mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The projections of European population showed large and sustained increases in life expectancy, the stratum of nonagenarians being the one with the largest increase in proportion [1]. This will cause an increase in the need of treatment of heart valve diseases. Although there is enough evidence on the safety of conventional valve surgery in advanced age [2–4], catheter-based treatments can be considered as wise approaches to treat nonagenarians, but data on the value of these interventions in these fragile patients are scarce. In this study, we sought to assess the early and intermediate outcome of transcatheter aortic valve replacement (TAVR) in a large series of nonagenarians from a multicenter, prospective study. Furthermore, a systematic review and meta-analysis of published data on nonagenarians who underwent TAVR were performed.
Materials and methods
Study design and data collection of the OBSERVANT study
OBSERVANT (observational study of effectiveness of AVR–TAVI procedures for severe aortic stenosis treatment) is a national observational, prospective, multicenter, cohort study that enrolled consecutive patients with severe aortic valve stenosis undergoing TAVR or SAVR at 93 Italian cardiology/cardiac surgery centers between December 2010 and June 2012. Details on the study design, patient eligibility criteria, and data collection modalities have been reported elsewhere [5, 6]. The study protocol has been approved by local ethical committees, and the patients gave an informed and written consent to the scientific treatment of their data in an anonymous form. Data on demographic characteristics, health status prior to intervention, comorbidities, and complete information on the type of intervention were collected into a standardized online datasheet on a password-protected website. An administrative follow-up has been set up for each enrolled patient through a record linkage with the National Hospital Discharged Records database for in-hospital events and with the Tax Registry Information System for information on survival. Collected data were stored and analyzed at the Italian National Institute of Health.
The study population included all consecutive adult patients requiring an aortic valve replacement for severe aortic valve stenosis (defined as an aortic valve area <1 cm2, maximum aortic velocity >4 m/s, or mean pressure gradient >40 mmHg). Patients who underwent isolated TF–TAVR or TA–TAVR were included in this analysis. Patients received Sapien XT or CoreValve bioprostheses.
All-cause mortality within 30 days from intervention and up to 3 years was the primary outcome measures of this study. Secondary outcome end points were in-hospital adverse events, such as stroke, vascular complications, red blood cell transfusion, and acute kidney injury. Stroke was defined as any focal deficit lasting >24 h, or focal deficit lasting <24 h with positive neuroimaging studies. Vascular complications were defined as any access site complication requiring surgical or percutaneous vascular intervention. Acute kidney injury was classified in three stages according to the AKIN definition criteria considering only the peak postoperative serum creatinine level within 48 h from the procedure [7, 8]. Other secondary outcome end points were major adverse cardiac and cerebrovascular events (MACCE) at 3 years. MACCE was defined as the composite end point, including any of these adverse events: death from any cause, stroke, myocardial infarction, percutaneous coronary intervention, and/or coronary surgery.
Meta-analysis
An English language literature review was performed through PubMed, Scopus, Sciencedirect, and Google Scholar on July 2015 for any study evaluating the outcome after TAVR for stenosis of the aortic valve in nonagenarians. The words employed in the search were: “transcatheter,” “TAVI”, “TAVR”, “nonagenarian”, and “90 years”. Reference list of obtained articles was used to broaden the search. We applied the guidelines for preferred reporting items for systematic reviews and meta-analyses (PRISMA) [9]. Two authors (F.B. and M.P.) independently reviewed the abstracts and articles and collected the data from the included studies.
To enter this analysis, studies had to fulfill the following criteria: (1) observational studies providing detailed baseline, operative, and outcome data of patients aged 90 years or more who underwent TAVR; (2) prospective or retrospective observational studies including ≥10 patients; (3) studies published in English language; (4) studies published as a full article; (5) studies reporting on at least 30-day postoperative mortality. Language of the articles was defined as reported in PubMed. We did not include in this study data unpublished or reported only in abstract.
The following criteria were used to exclude studies from this analysis: (1) studies reporting controversial data (data not matching each other with the text and tables); (2) studies without information on baseline characteristics, treatment modality, and data on at least the primary outcome end point of this study; (3) studies with duplicate data.
Data on study size, study design, baseline characteristics, operative data, early adverse events, and late survival were retrieved only from the articles, and no attempt to get specific or missing data from the authors was made. Each study was independently evaluated by M.P and F.B for inclusion or exclusion from this analysis. Baseline and operative data of interest were extracted and reported in a dedicated Excel spreadsheet.
The quality of the included studies was independently assessed by three investigators (F.B., M.P.) using the National Heart, Blood, and Lung Institute (NHBLI) criteria for study quality assessment of case–control series (https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/case–control; accessed on April 22, 2016).
The main outcome measure of this study was any 30-day and late postoperative mortality. Secondary outcome end points of this study were stroke, myocardial infarction, Acute Kidney Injury Network grades 1–3 [7], vascular access complications, major bleeding, permanent pacemaker implantation, paravalvular regurgitation, mean postoperative transvalvular gradient, and length of stay in the intensive care unit.
Statistical analysis
Statistical analyses were performed using the SPSS statistical package, version 22 (IBM Corporation, Armonk, New York, USA). The freely downloadable software Open Meta-analyst (http://www.cebm.brown.edu/open_meta/, accessed on February 29, 2016) was used for meta-analysis of aggregate data. Continuous variables are presented as the mean ± standard deviation and categorical variables as counts and percentages. Operative deaths were included in survival analyses. Time to event was estimated using the Kaplan–Meier’s method. Multivariate analysis was not performed because of the small size of this series. In meta-analysis of aggregate data, proportions were pooled using random effects models to incorporate the anticipated heterogeneity of these small size observational studies. Analysis of time-to-event outcome end points was performed by calculating the proportion of patients alive at each interval after estimating the number of events and the number of patients at risk from available survival curves and tables using a spreadsheet developed by Tierney and collaborators [10]. This enables to estimate the number of patients at risk for those studies not reporting it at each study interval. Once the number of events and the number of patients at risk were estimated, the proportions of patients alive at each interval were calculated and were then pooled by the random-effect method. Heterogeneity across studies was evaluated using the I 2 test. Sensitivity and meta-regression analyses were not performed due to the limited number of available studies. The results are expressed as pooled mean and proportions and mean with 95 % confidence interval (95 % CI). A P < 0.05 was considered statistically significant.
Results
Early and late outcome in the OBSERVANT study
For the purposes of this study, 80 patients fulfilled the inclusion criteria and were the subjects of this analysis. Their baseline characteristics and echocardiographic data are summarized in Tables 1 and 2. Seven patients underwent transapical TAVR (8.8 %). The procedure was performed in 19 patients (23.8 %) in local anesthesia.
Thirty-day mortality in this series was 6.3 %. The observed/expected mortality ratio as estimated by the EuroSCORE II was 0.84. Transfemoral TAVR was associated with a 30-day mortality of 5.5 % and transapical TAVR of 14.3 % (P = 0.36). None of these patients experienced stroke. Permanent pacemaker implantation was necessary in 20 % of patients. No severe paravalvular regurgitation was observed in this series, but mild-to-moderate regurgitation was observed in 57.5 % of patients. Five patients (6.3 %) required dialysis after TAVR. The mean length of stay in the intensive care unit was 2.3 ± 2.9 days. Other early adverse events are summarized in Table 3.
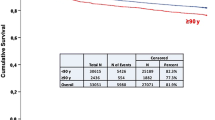
The mean follow-up was 1.95 ± 1.1 years. Survival at 1, 2, and 3 years was 79.6, 71.9, and 61.5 % (Fig. 1). At 3 years, freedom from MACCE was 53.8 %, from stroke was 90.1 %, from myocardial infarction was 91.4 %, and from coronary revascularization was 94.8 %.
Meta-analysis
Literature search yielded 39 articles potentially fulfilling the inclusion criteria of this study (Fig. 2). Two studies [11, 12] were excluded, because the involved centers contributed to a multicenter study [13] with study periods overlapping more than 50 %. Nine articles [13–21] were suitable for this analysis which included also the present data from the OBSERVANT study. In overall, 10 series provided data on 1227 nonagenarians who underwent TAVR. Characteristics of these studies are reported in Table 4. Eight studies reported on at least 1-year survival. The NHLBI quality of four studies was judged to be fair and that of six studies was good. Pooled baseline characteristics of nonagenarians are summarized in Table 5. The high prevalence in these patients of coronary artery disease, stroke, peripheral vascular disease, and pulmonary disease is of clinical relevance. Furthermore, these patients had a high prevalence of atrial fibrillation and prior implanted pacemaker. Specific data on concomitant coronary revascularization were not available from these studies.
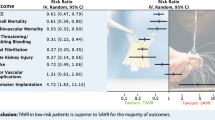
Pooled 30-day mortality rate was 7.1 % (Fig. 3), stroke 2.8 %, vascular access complication 8.8 %, and permanent pacemaker implantation 10.6 %. Mild-to-severe paravalvular regurgitation was observed in 60.1 % of patients (Table 6). Two studies [13, 20] along with the OBSERVANT study provided data on 30-day mortality after transfemoral (686 patients) and transapical TAVR (249 patients). Transapical TAVR was associated with a significantly higher risk of early mortality compared with transfemoral TAVR (pooled proportion: 14.2 versus 6.5 %; HR 2.56, 95 % CI 1.63–4.01, I 2 0 %).
Pooled survival rates at 1-, 2-, and 3-year were 79.2, 68.2, and 55.6 %, respectively. Details on survival proportions, estimated patients at risk, and heterogeneities are summarized in Fig. 4. Supplementary Fig. 1 shows forest plots of pooled survival at these study intervals.
Discussion
The results of the OBSERVANT study demonstrated that TAVR can be performed in nonagenarians with low risk of early mortality and morbidity. Such excellent results were obtained despite a high prevalence of significant comorbidities, such as decreased renal function, peripheral arteriopathy, pulmonary disease, and coronary artery disease (Table 1). It is also worth noting that about 20 % of these patients had a prior pacemaker implanted. In this study, the observed/expected mortality ratio as estimated by the EuroSCORE II was 0.84, which suggests that this risk score may provide a reliable estimate of the operative risk in these very elderly. We may expect that a policy of strict preoperative selection was adopted in all these patients, but still TAVR was not associated with an increased risk of adverse events. In the OBSERVANT series, no patient experienced postoperative stroke, the rate of severe acute kidney injury was about 6 %, and the mean length of stay in the intensive care unit was 2.3 days. However, almost 60 % of patients had a mild-to-moderate paravalvular regurgitation.
Pooled analysis of data from the OBSERVANT study and other nine series confirmed the high prevalence of comorbidities in nonagenarians (Table 5), and that TAVR was generally associated with a favorable early outcome (Table 6). In overall, the risk of end-organ and access complications can be considered comparable with that of current series, including mostly younger patients. Pooled analysis confirmed the rather high rate of mild-to-severe paravalvular regurgitation, but only 10 % being moderate to severe.
Data from the OBSERVANT study as well as those from pooled analysis showed that 3-year survival in nonagenarians is about 55 %, which is excellent in patients whose life expectancy is rather short. Indeed, there is evidence that such results are similar to age and gender matched general population [11, 13]. The improved functional health status and quality of life at mid-term after TAVR as demonstrated in recent series [13] further confirm the validity of this treatment method in nonagenarians.
It is worth noting that the rate of paravalvular regurgitation observed in the OBSERVANT series as well as in the pooled analysis was about 60 % and that about 10 % of patients had a moderate-to-severe regurgitation. This finding may to some extent be attributed to the type of valve prostheses used during the study period. However, we may speculate that such a high rate of paravalvular regurgitation may most likely be related to the severity of calcification of the aortic valve in these nonagenarians.
Two previous studies [17, 19] reported on postoperative rate of pacemaker implantation >20 %. In the present series, the rate of pacemaker implantation was rather high (20 %) as well, but this may be due to the relatively small sample size that may affect the estimation of the rate of this adverse event. The type of prosthesis might have had an impact on this outcome end point. However, we do not have sufficient data to perform a sub-analysis on this issue.
The relatively large and increasing number of nonagenarians who were included in the published studies suggests that there is an increasing need of invasive treatment of cardiovascular diseases in these patients. Remains the question whether this less invasive treatment strategy is cost-effective in nonagenarians. TAVR can be considered a costly alternative to conventional aortic valve replacement in patients without a prohibitive operative risk, but there is a burden of evidence on its cost-effectiveness in inoperable patients [22, 23]. Since, at this stage, a few would argue that the conventional aortic valve replacement is a valid option in nonagenarians [24], we may conclude that TAVR is highly justified in selected nonagenarians in view of its potential to increase their quality of life and provide a survival similar to age- and gender-matched general population.
A few studies reported on the outcome according to access route. The present pooled analysis indicates that transapical TAVR is associated with excessive early mortality compared with transfemoral TAVR [25]. We do not have data to assess any potential difference in the baseline risk factors of these study groups. However, we may assume that a mini-thoracotomy and the related need of general anesthesia are too risky in such a fragile patient’s population as demonstrated also in younger patients [26].
Study limitations
A number of limitations may affect the validity of the present findings. First, the decision to treat nonagenarians was most certainly based on a careful preoperative selection taking into consideration patients’ comorbidities and frailty status. Therefore, a significant selection bias can be expected, and these results cannot be generalized. Similarly, pooled analysis included data from institutional series with large volume and specific experience in TAVR. Therefore, these results may not be reproducible in all centers. Second, this study did not provide a comparative data with younger patients. We do believe that comparing the results of TAVR in nonagenarians versus younger patients may introduce a significant bias as nonagenarians were likely selected according to more stringent criteria than younger patients. Despite the limitations of strict selection criteria, a study by Yamamoto et al. [21] showed that adjusted mortality of nonagenarians after TAVR is not worse than younger patients. These results were confirmed by a recent study by Abramowitz et al. [18]. Finally, despite a few series reported fairly good results with SAVR in nonagenarians [11, 15], the frailty of these patients and their short life expectancy are reasonable arguments against conventional surgery in nonagenarians. Because of these reasons, we did not plan any comparative analysis of TAVR versus SAVR in this subset of patients.
Conclusions
In conclusion, the results of the OBSERVANT study and meta-analysis of published data suggest that in selected nonagenarians, TAVR is associated with low postoperative morbidity and excellent early and intermediate survival. Preliminary data indicate that transapical TAVR is associated with excessive early mortality in nonagenarians.
References
European Commission (2014) The 2015 ageing report: underlying assumptions and projection methodologies. 8:1–413. http://ec.europa.eu/economy_finance/publications/european_economy/2014/pdf/ee8_en.pdf. Accessed 29 Feb 2016
Aoyagi S, Fukunaga S, Arinaga K, Tomoeda H, Akasu K, Ueda T (2010) Heart valve surgery in octogenarians: operative and long-term results. Heart Vessels 25:522–528
Cappabianca G, Ferrarese S, Musazzi A, Terrieri F, Corazzari C, Matteucci M, Beghi C (2016) Predictive factors of long-term survival in the octogenarian undergoing surgical aortic valve replacement: 12-year single-centre follow-up. Heart Vessels. doi:10.1007/s00380-016-0804-3
Biancari F, Barbanti M, Santarpino G, Deste W, Tamburino C, Gulino S, Immè S, Di Simone E, Todaro D, Pollari F, Fischlein T, Kasama K, Meuris B, Dalén M, Sartipy U, Svenarud P, Lahtinen J, Heikkinen J, Juvonen T, Gatti G, Pappalardo A, Mignosa C, Rubino AS (2016) Immediate outcome after sutureless versus transcatheter aortic valve replacement. Heart Vessels 31:427–433
Gruppo di Lavoro tecnico dello studio OBSERVANT, D’Errigo P, Fusco D, Grossi C, Ramondo AB, Ranucci M, Santini F, Santoro G, Seccareccia F, Tamburino C (2010) OBSERVANT: observational study of appropriateness, efficacy and effectiveness of AVR-TAVI procedures for the treatment of severe symptomatic aortic stenosis. Study protocol. G Ital Cardiol (Rome) 11:897–909
Tamburino C, Barbanti M, D’Errigo P, Ranucci M, Onorati F, Covello RD, Santini F, Rosato S, Santoro G, Fusco D, Grossi C, Seccareccia F, OBSERVANT Research Group (2015) 1-year outcomes after transfemoral transcatheter or surgical aortic valve replacement: results from the Italian OBSERVANT study. J Am Coll Cardiol 66:804–812
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A (2007) Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11:R31
D’Errigo P, Moretti C, D’Ascenzo F, Rosato S, Biancari F, Barbanti M, Santini F, Ranucci M, Miceli A, Tamburino C, Onorati F, Santoro G, Grossi C, Fusco D, Seccareccia F, on behalf of the OBSERVANT Research Group (2016) Transcatheter aortic valve implantation versus surgical aortic valve replacement for severe aortic stenosis in patients with chronic kidney disease stages 3b-5. Ann Thorac Surg. doi:10.1016/j.athoracsur.2016.01.109
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Tierney JF, Stewart LA, Ghersi D, Burdett Sarah, Sydes MR (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8:16
Mack MC, Szerlip M, Herbert MA, Akram S, Worley C, Kim RJ, Prince BA, Harrington KB, Mack MJ, Holper EM (2015) Outcomes of treatment of nonagenarians with severe aortic stenosis. Ann Thorac Surg 100:74–80
Kayatta MO, Thourani VH, Jensen HA, Condado JC, Sarin EL, Kilgo PD, Devireddy CM, Leshnower BG, Mavromatis K, Li C, Guyton RA, Stewart JP, Simone A, Keegan P, Block P, Lerakis S, Babaliaros VC (2015) Outcomes for transcatheter aortic valve replacement in nonagenarians. Ann Thorac Surg 100:1261–1267
Thourani VH, Jensen HA, Babaliaros V, Kodali SK, Rajeswaran J, Ehrlinger J, Blackstone EH, Suri RM, Don CW, Aldea G, Williams MR, Makkar R, Svensson LG, McCabe JM, Dean LS, Kapadia S, Cohen DJ, Pichard AD, Szeto WY, Herrmann HC, Devireddy C, Leshnower BG, Ailawadi G, Maniar HS, Hahn RT, Leon MB, Mack M (2015) Outcomes in nonagenarians undergoing transcatheter aortic valve replacement in the PARTNER-I Trial. Ann Thorac Surg 100:785–793
Noble S, Frangos E, Samaras N, Ellenberger C, Frangos C, Cikirikcioglu M, Bendjelid K, Frei A, Myers P, Licker M, Roffi M (2013) Transcatheter aortic valve implantation in nonagenarians: effective and safe. Eur J Intern Med 24:750–755
Murashita T, Greason KL, Suri RM, Nkomo VT, Holmes DR, Rihal CS, Mathew V (2014) Aortic valve replacement for severe aortic valve stenosis in the nonagenarian patient. Ann Thorac Surg 98:1593–1597
Pascual I, López-Otero D, Muñoz-García AJ, Alonso-Briales JH, Avanzas P, Morís C (2014) Safety and efficacy of transcatheter aortic valve implantation in nonagenarian patients. Rev Esp Cardiol 67:583–584
Akin I, Kische S, Paranskaya L, Schneider H, Rehders TC, Turan GR, Divchev D, Kundt G, Bozdag-Turan I, Ortak J, Birkemeyer R, Nienaber CA, Ince H (2012) Morbidity and mortality of nonagenarians undergoing CoreValve implantation. BMC Cardiovasc Disord 12:80
Abramowitz Y, Chakravarty T, Jilaihawi H, Kashif M, Zadikany R, Lee C, Matar G, Cheng W, Makkar RR (2015) Comparison of outcomes of transcatheter aortic valve implantation in patients ≥90 versus <90 years. Am J Cardiol 116:1110–1115
Verouhis D, Yamasaki K, Ivert T, Rück A, Settergren M (2014) Transcatheter aortic valve implantation is feasible and safe in nonagenarians. J Am Geriatr Soc 62:189–190
Yamamoto M, Mouillet G, Meguro K, Gilard M, Laskar M, Eltchaninoff H, Fajadet J, Iung B, Donzeau-Gouge P, Leprince P, Leuguerrier A, Prat A, Lievre M, Chevreul K, Dubois-Rande JL, Teiger E, FRANCE-2 Registry Investigators (2014) Clinical results of transcatheter aortic valve implantation in octogenarians and nonagenarians: insights from the FRANCE-2 registry. Ann Thorac Surg 97:29–36
Yamamoto M, Meguro K, Mouillet G, Bergoend E, Monin JL, Lim P, Dubois-Rande JL, Teiger E (2012) Comparison of effectiveness and safety of transcatheter aortic valve implantation in patients aged ≥90 versus <90 years. Am J Cardiol 110:1156–1163
Indraratna P, Ang SC, Gada H, Yan TD, Manganas C, Bannon P, Cao C (2014) Systematic review of the cost-effectiveness of transcatheter aortic valve implantation. J Thorac Cardiovasc Surg 148:509–514
Eaton J, Mealing S, Thompson J, Moat N, Kappetein P, Piazza N, Busca R, Osnabrugge R (2014) Is transcatheter aortic valve implantation (TAVI) a cost-effective treatment in patients who are ineligible for surgical aortic valve replacement? A systematic review of economic evaluations. J Med Econ 17:365–375
Davis JP, LaPar DJ, Crosby IK, Kern JA, Lau CL, Kron IL, Ailawadi G (2014) Nonagenarians undergoing cardiac surgery. J Card Surg 29:600–604
Biancari F, Rosato S, D’Errigo P, Ranucci M, Onorati F, Barbanti M, Santini F, Tamburino C, Santoro G, Grossi C, Covello RD, Ventura M, Fusco D, Seccareccia F, on behalf of the OBSERVANT Research Group (2016) Immediate and intermediate outcome after transapical versus transfemoral transcatheter aortic valve replacement. Am J Cardiol 117:245–251
Takagi H, Umemoto T, ALICE (All-Literature Investigation of Cardiovascular Evidence) Group (2014) A meta-analysis of adjusted observational studies for mortality in transapical versus transfemoral aortic valve implantation. Int J Cardiol 174:165–170
Acknowledgements
The OBSERVANT Study was supported by a Grant (Fasc. 1M30) from Italian Ministry of Health and Istituto Superiore di Sanità. The authors thank Gabriella Badoni for her technical support in the organizational phases of the study. Fulvia Seccareccia, Paola D’Errigo, Stefano Rosato, Alice Maraschini, Gabriella Badoni, National Center for Epidemiology, Surveillance and Health Promotion-ISS; Corrado Tamburino, Marco Barbanti, SICI-GISE, Gennaro Santoro, FIC, ANMCO; Francesco Santini, Francesco Onorati, Claudio Grossi, SICCH; Marco Ranucci, Remo Daniel Covello, ITACTA; Danilo Fusco, Epidemiology Department Lazio Region; Rossana De Palma, Emilia Romagna Region; Salvatore Scondotto, Sicilia Region.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof. Tamburino receives honorary fees from Medtronic and Abbott; there is no potential conflict of interest related to the matter of the article for any other author.
Additional information
On behalf of the OBSERVANT Research Group.
Members of OBSERVANT Research Group are listed in Acknowledgements.
Rights and permissions
About this article
Cite this article
Biancari, F., D’Errigo, P., Rosato, S. et al. Transcatheter aortic valve replacement in nonagenarians: early and intermediate outcome from the OBSERVANT study and meta-analysis of the literature. Heart Vessels 32, 157–165 (2017). https://doi.org/10.1007/s00380-016-0857-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0857-3