Abstract
The purpose of this study is to access the outcomes of aortic bypass graft placement in children. This is a retrospective review of all children having aortic bypass graft placement for aortic arch obstruction for the first time between 1982 and 2013 at a single institution. The actuarial survival and the freedom from aortic arch reoperation were calculated and compared between the groups. Seventy consecutive children underwent aortic bypass graft placements. The median age and body weight at the operation were 14 days and 3.6 kg. There were 7 early deaths, 6 late deaths, and 7 heart transplants during the median follow-up of 10.8 years (0.0–31.5 years). The actuarial transplant free survival was 64.7 % at 20 years and the freedom from aortic arch reoperation was 50.5 % at 10 years. Between the children younger than 1 year old and older than 1 year old, there were significant differences in actuarial transplant free survival (56.4 vs. 100 % at 15 years, p = 0.0042) and in the freedom from aortic arch reoperation (18.7 vs. 100 % at 10 years, p < 0.001). The children who received aortic bypass graft larger than 16 mm in size had no aortic arch reoperation at 15 years. The aortic bypass graft placement for aortic arch obstruction can be done with low mortality and morbidity for children who can receive bypass graft larger than 16 mm in size. However, it should be avoided for the neonates and infants except selected situations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Complex aortic arch obstruction including interrupted aortic arch, hypoplastic aortic arch with coarctation of the aorta, and recurrent coarctation of the aorta still remains challenging for surgical repair and the necessity of reoperation for recurrent aortic arch obstruction is not completely avoidable [1, 2].
Historically, the surgical technique for the aortic arch obstruction with intracardiac anomaly at our institution was the aortic bypass graft placement from the ascending (or transverse arch) to descending aorta [3, 4]. The aortic bypass graft placement could effectively avoid the use of cardiopulmonary bypass and the midline incision in small children, which would facilitate the postoperative recovery and the intracardiac repair at next stage operation. It could also avoid the overwhelming dissection in redo operations, which also would facilitate the postoperative recovery and avoid postoperative complications [5]. The aortic bypass graft placement was switched to the native-to-native aortic tissue anastomosis with patch augmentation under cardiopulmonary bypass for the neonates and early infants at our institution as the outcomes for cardiopulmonary bypass surgery in early infancy had significantly improved in 1990s [6]. However, the aortic bypass graft placement remains as an important surgical option for the grown-up patients who have multiple surgical histories [7, 8]. The infants who are not good candidate for cardiopulmonary bypass due to complicated medical situations or complex anatomy [9] might have benefit from this surgical approach.
The purpose of this study is to review our experience of aortic bypass graft placement for aortic arch obstruction in children and to access its efficacy.
Materials and methods
Study design
Between January 1982 and December 2013, all children (less than 20 years old) who had the first aortic bypass graft placement for aortic arch obstruction were identified using the institutional cardiothoracic surgical database at the Arkansas Children’s Hospital. The patients who had the second or third aortic bypass graft placement were excluded from this study. This study was approved and monitored by the Institutional Review Board at the University of Arkansas for Medical Sciences and the need for patient consent was waived due to its retrospective nature.
The medical records of each subject were reviewed with regards to demographic data, past medical history, primary and secondary diagnosis, intraoperative data with surgical techniques, postoperative outcomes including immediate and late complications and reoperation. Follow-up data were obtained from the last clinic visit.
Statistical analysis
Descriptive statistics were expressed as median (range) for continuous patient characteristics, and frequency (percentage) for categorical patient characteristics. The primary outcomes of the study were time-to-death and time-to-reoperation. The time-to-death was defined as the time from the date of surgery to death (event) or heart transplant (event) or last follow-up date (censored). The time-to-reoperation was defined as the time from the date of surgery to the date of aortic arch reoperation (event) or death (censored) or last follow-up date (censored). The Kaplan–Meier estimates of the survival function were computed over the study period for all the patients and subgroups of patients with respect to their ages and graft size. The log-rank tests were carried out to compare the survival distributions among subgroups of patients. A smoothed hazard curve was plotted for the time-to-reoperation to investigate the change in the hazard of aortic arch reoperation over time. A Cox proportional hazards model was fitted for time-to-reoperation as a function of each risk factor to evaluate the univariate association between time-to-reoperation and each risk factor. Risk factors with a univariate p value less than 0.1 were selected for the multivariable Cox proportional hazards model. Redundancy analysis was performed to check the collinearity among the all risk factors to be included in the multivariable model, and none of the variables was found to be redundant. The hazard ratio estimate and its corresponding 95 % confidence interval was computed for each risk factor based on the models.
p values less than 0.05 were considered to indicate statistical significance. All the data were analyzed using statistical software Stata/MP 14 (StataCorp LP, College Station, TX, USA).
Results
Patient characteristics
The study cohort included 70 patients (40 male and 30 female). The age at operation was younger than 1 year old in 44 patients, between 1 and 10 years old in 8 patients, and older than 10 years old in 18 patients. The median age and body weight were 14 days (0.0–19.6 years) and 3.6 kg (1.4–90.4 kg).
The aortic arch morphology included 28 patients (40 %) with interrupted aortic arch, 18 patients (26 %) with hypoplastic arch, 18 patients (26 %) with recurrent coarctation, and 6 patients (9 %) with complex coarctation of the aorta. The intracardiac morphology included 30 patients (43 %) with no major shunt lesion, 21 patients (30 %) with unrepaired ventricular septal defect, 12 patients (17 %) with unrepaired complex intracardiac anomaly, and 7 patients (10 %) with single ventricle physiology. Three patients had DiGeorge syndrome and 2 patients had Trisomy 21.
Operative intervention
The operative approach included 56 left thoracotomy, 7 median sternotomy, 7 median sternotomy and thoracotomy (1 median sternotomy and right thoracotomy for the patients who had right-sided interrupted aortic arch [8]). Thirty-three patients had concomitant procedure including 26 pulmonary artery banding and 7 intracardiac procedures with cardiopulmonary bypass (4 Damus-Kaye-Stansel anastomosis, 2 ventricular septal defect closure, and 1 right ventricle to pulmonary artery conduit replacement). All grafts were expanded polytetrafluoroethylene tubes, and 41 small size grafts (4–8 mm), 5 medium size grafts (10–15 mm), and 24 large size grafts (more than 16 mm) were used.
The patient characteristics and operative intervention were summarized in Table 1.
Operative outcomes
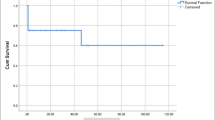
There were 7 early and 6 late deaths with median follow-up of 10.8 years (0.0–31.5 years). All mortalities were cardiac related except one patient with malignant teratoma. Two unilateral diaphragmatic plication due to the phrenic nerve injury were performed for 2 neonates (2.8 %). During the follow-up period, 7 patients (2 patients with single ventricle physiology) received orthotopic heart transplant, of which 2 patients eventually had late mortalities. The operative outcomes were summarized in Table 2. The actuarial transplant free survival was 64.7 % at 20 years (95 % confidence interval 46.5–78.1 %, Fig. 1a). The actuarial transplant free survival was further analyzed by dividing the patients by age (children younger than 1 year old vs. children older than 1 year old), which showed significant difference (56.4 vs. 100 % at 15 years, p = 0.0042).
Among 63 hospital survivors, 26 patients required 32 aortic arch reoperations for recurrent obstruction with median interval of 6.3 years after aortic bypass graft placement. The number of aortic arch reoperations was once in 20 patients and twice in 6 patients. All heart transplant patients had aortic arch reoperation before or at the time of transplant. The details of reoperation were redo aortic bypass graft placement in 28 operations, patch aortoplasty in 2, redo aortic bypass graft and apico-aorta graft placement in 1, and shunt placement between the neck vessels in 1 (Fig. 2). Among 42 long-term survivors with recent clinic visit, all are in good health with New York Heart Association Class I or II. Nineteen patients (45 %) were on anti-hypertensive drugs, and all but one patient has good blood pressure control with systolic blood pressure less than 160 mmHg at latest clinic visit. The freedom from aortic arch reoperation for recurrent obstruction was 50.5 % at 10 years (95 % conficence interval 35.1–64.0 %, Fig. 1b).
The posterior view of three dimensional reconstruction of chest computed tomography for the patient with interrupted aortic arch and ventricular septal defect showing two bypass grafts between the ascending aorta and the descending aorta (white arrows). The patient underwent 1st aortic bypass graft and pulmonary artery banding via left thoracotomy in neonatal period, the intracardiac repair at 6 months old, and 2nd aortic bypass via left thoracotomy at 13 years old
The freedom from aortic arch reoperation was further analyzed by dividing the patients by age (children younger than 1 year old vs. children older than 1 year old) and by conduit size, which showed significant differences by age (18.7 and 100 % for children younger than 1 year old and children older than 1 year old at 10 years, p < 0.001, Fig. 3a) and by conduit size (19.1, 66.7, and 100 % for small, medium, and large graft at 10 years, p < 0.001, Fig. 3b).
Risk analysis
The Cox proportional hazards model to investigate the risk factors for aortic arch reoperation showed that the age, body weight, and aortic arch morphology were significantly associated with aortic arch reoperation in univariate analysis (p = 0.016, 0.018, and 0.001, respectively). However, none of the risk factors was significantly associated with aortic arch reoperation in multivariable analysis (Table 3).
A smoothed hazard curve over time showed that hazard for aortic arch reoperation was increased over time and peaked at 9 years after initial operation (Fig. 4).
Discussion
This review of aortic bypass graft placement at a single institution demonstrated a reasonable long-term survival, considering that the majority of operations were performed in 1980s and 1990s.
The aortic bypass graft placement is an attractive surgical option for the grown-up patient with recurrent aortic arch obstruction to avoid overwhelming dissection and postoperative complications [5, 7, 8]. The aortic bypass graft placement can be done through the median sternotomy or thoracotomy, and in the anatomic fashion or extra-anatomic fashion, based on the patient’s past surgical history and surgeon’s discretion [5, 7, 8, 10]. McKellar and colleagues reported excellent intermediate-term results of extra-anatomic ascending to descending aorta bypass for 50 adult patients with no graft-related reoperation in the mean follow-up of 33 months. The extra-anatomic aortic bypass graft could also effectively relieve the systemic hypertension [10]. However, the long-term outcomes of aortic bypass graft placement for children are still unclear. Moreover, the aortic bypass graft placement could not be a good option due to the concerns for length and size of the graft for the growing children. Kanter and colleagues reported the long-term outcomes of extra-anatomic aortic bypass via sternotomy in 19 children aged 2 months to 18 years (mean 10.7 years) in the mean follow-up of 7.9 years with no hospital or late death. However, they commented that the percutaneous balloon dilatation or traditional surgical techniques were their preferred choice and the extra-anatomic aortic bypass was chosen only for the selected patients [11].
In this current study, the children older than 1 year old had good long-term outcomes of aortic bypass graft placement with low mortality and morbidity. One patient with 14 mm bypass graft required aortic arch reoperation, and the other patient who had single ventricle physiology and 16 mm bypass graft for recurrent coarctation required heart transplantation 25 years after Fontan completion and subsequently died due to fungal infection. The actuarial transplantation free survival and the freedom from aortic arch reoperation for children older than 1 year old were 100 and 91.7 % at 15 years. The majority of these children (92 %) received bypass graft larger than 16 mm in size, which seemed adequate to avoid aortic arch reoperation under the dual aortic pathway situation with narrowed native aortic arch and large bypass graft.
In contrast, the children younger than 1 year old had much worse outcomes. Our preferred strategy for the aortic arch obstruction with intracardiac anomaly in the past, especially for the patients with interrupted aortic arch, was the staged repair with aortic bypass graft placement without cardiopulmonary bypass, due to the high early mortality of the aortic arch repair under cardiopulmonary bypass for neonates and infants. Unexpectedly, the children younger than 1 year old in current study still had relatively high early mortality of 16 % (7/44) even without cardiopulmonary bypass use. The long-term outcomes of aortic bypass graft in these children had 5 late mortalities and 6 heart transplants, which resulted in actuarial transplant free survival of 63.6 % at 15 years. Even this result was comparable with other operative techniques used in 1980s and 1990s [1], the aortic arch reoperation was mandatory in these children. The reasons for late death and severe heart failure necessitating heart transplant were multi-factorial, and it could be attributable to the residual aortic arch obstruction due to the size mismatch of bypass graft to growing patient over time or other residual lesions [12]. Recently, we have selectively employed aortic bypass graft placement for infant with complicated medical and anatomical conditions [9]. The hybrid approach with ductal stent placement and bilateral pulmonary artery banding could be another option as surgical palliation for these patients in current era [13].
Limitations of the present study include its retrospective and non-randomized nature.
In conclusion, the aortic bypass graft placement for aortic arch obstruction can be done with low mortality and morbidity for children who can receive bypass graft larger than 16 mm in size. However, it should be avoided for the neonates and infants except selected situations.
References
McCrindle BW, Tchervenkov CI, Konstantinov IE, Williams WG, Neirotti RA, Jacobs ML, Blackstone EH, Congenital Heart Surgeons Society (2005) Risk factors associated with mortality and interventions in 472 neonates with interrupted aortic arch: a Congenital Heart Surgeons Society study. J Thorac Cardiovasc Surg 129:343–350
Brown JW, Ruzmetov M, Hoyer MH, Rodefeld MD, Turrentine MW (2009) Recurrent coarctation: is surgical repair of recurrent coarctation of the aorta safe and effective? Ann Thorac Surg 88:1923–1930
Sturm JT, vanHeeckeren DW, Borkat G (1981) Surgical treatment of interrupted aortic arch in infancy with expanded polytetrafluoroethylene grafts: 2-year follow-up results. J Thorac Cardiovasc Surg 81:245–249
Shinkawa T, Jaquiss RBD, Imamura M (2012) Single institutional experience of interrupted aortic arch repair over 28 years. Interact CardioVasc Thorac Surg 14:551–555
Edie RN, Janani J, Attai LA, Malm JR, Robinson G (1975) Bypass grafts for recurrent or complex coarctations of the aorta. Ann Thorac Surg 20:558–566
Karl TR, Sano S, Brawn W, Mee RB (1992) Repair of hypoplastic or interrupted aortic arch via sternotomy. J Thorac Cardiovasc Surg 104:688–695
Connolly HM, Schaff HV, Izhar U, Dearani JA, Warnes CA, Orszulak TA (2001) Posterior pericardial ascending-to-descending aortic bypass: an alternative surgical approach for complex coarctation of the aorta. Circulation 104:I133–I137
Izhar U, Schaff HV, Mullany CJ, Daly RC, Orszulak TA (2000) Posterior pericardial approach for ascending aorta-to-descending aorta bypass through a median sternotomy. Ann Thorac Surg 70:31–37
Uppu SC, Shinkawa T, Imamura M (2012) Single institution experience with a right-sided interrupted aortic arch. Interact CardioVasc Thorac Surg 15:802–804
McKellar SH, Schaff HV, Dearani JA, Daly RC, Mullany CJ, Orszulak TA, Sundt TM 3rd, Connolly HM, Warnes CA, Puga FJ (2007) Intermediate-term results of ascending-descending posterior pericardial bypass of complex aortic coarctation. J Thorac Cardiovasc Surg 133:1504–1509
Kanter KR, Erez E, Williams WH, Tam VK (2000) Extra-anatomic aortic bypass via sternotomy for complex aortic arch stenosis in children. J Thorac Cardiovasc Surg 120:885–890
Miyazaki A, Sakaguchi H, Ohuchi H, Yasuda K, Tsujii N, Matsuoka M, Yamamoto T, Yazaki S, Tsuda E, Yamada O (2015) The clinical characteristics of sudden cardiac arrest in asymptomatic patients with congenital heart disease. Heart Vessels 30:70–80
Akintürk H, Michel-Behnke I, Valeske K, Mueller M, Thul J, Bauer J, Hagel KJ, Schranz D (2007) Hybrid transcatheter-surgical palliation: basis for univentricular or biventricular repair: the Giessen experience. Pediatr Cardiol 28:79–87
Acknowledgments
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Shinkawa, T., Chipman, C., Holloway, J. et al. Single center experience of aortic bypass graft for aortic arch obstruction in children. Heart Vessels 32, 76–82 (2017). https://doi.org/10.1007/s00380-016-0842-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0842-x