Abstract
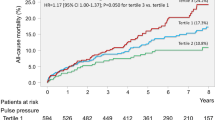
Data regarding relationship between pulse pressure (PP) at admission and in-hospital outcome in patients with acute myocardial infarction (AMI) undergoing primary percutaneous coronary intervention (PCI) are still lacking. A total of 1413 primary PCI-treated AMI patients were classified into quintiles based on admission PP (<40, n = 280; 40–48, n = 276; 49–57, n = 288; 58–70, n = 288; and ≥71 mmHg, n = 281). The patients with PP < 40 mmHg tended to have higher prevalence of male, smoking, and Killip class ≥3 at admission; right coronary artery, left main trunk (LMT), or multivessels as culprit lesions; larger number of diseased vessels; lower Thrombolysis in Myocardial Infarction (TIMI) grade in the infarct-related artery before/after primary PCI; and higher value of peak creatine phosphokinase concentration. Patients with PP < 40 mmHg had highest mortality, while patients with PP 49–57 mmHg had the lowest: 11.8 % (<40), 7.2 % (40–48), 2.8 % (49–57), 5.9 % (58–70), and 6.0 % (≥71 mmHg). On multivariate analysis, Killip class ≥3 at admission, LMT or multivessels as culprit lesions, chronic kidney disease, and age were the independent positive predictors of the in-hospital mortality, whereas admission PP 49–57 mmHg, hypercholesterolemia, and TIMI 3 flow before/after PCI were the negative ones, but admission PP < 40 mmHg was not. These results suggest that admission PP 49–57 mmHg might be correlated with better in-hospital prognosis in Japanese AMI patients undergoing primary PCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Accumulating evidence have indicated that high pulse pressure (PP), which depends on ventricular stroke volume, large arterial stiffness, and timing of wave reflections, is an independent predictor for mortality and cardiovascular events in a variety of populations, such as hypertensive patients [1–3], patients undergoing percutaneous/surgical revascularization [4], patients with left ventricular systolic dysfunction after myocardial infarction [5], and the general population [6, 7]. By contrast, several reports have shown that low PP is associated with increased mortality in patients with advanced or decompensated heart failure [8–10] and in patients with heart failure after myocardial infarction [11]. In addition, a recent report has indicated a relationship between low PP at peak exercise and cardiac mortality in patients with systolic heart failure [12]. However, the relationship between admission PP, clinical manifestations, and in-hospital outcome in acute myocardial infarction (AMI) patients undergoing primary percutaneous coronary intervention (PCI) remains uncertain. The AMI-Kyoto Multi-Center Risk Study, a large multicenter observational study in which collaborating hospitals in Kyoto Prefecture have collected demographic, procedural, and outcome data on AMI patients, was established in 2000 in order to analyze these data and establish an emergency-hospital network for heart diseases in Kyoto [13]. The purpose of the present study was therefore to examine the prognostic impact of admission PP on in-hospital outcome in Japanese AMI patients undergoing primary PCI, using data from the AMI-Kyoto Multi-Center Risk Study.
Patients and methods
Patient population
From July 2006 to December 2010, 1636 consecutive patients with a diagnosis of AMI, who were admitted to AMI-Kyoto Multi-Center Risk Study Group Hospitals within 24 h after the onset of AMI, were enrolled in the present study. Of these, excluding cases with cardiopulmonary arrest on arrival, 1443 patients underwent primary PCI, of whom data on clinical background and PP at admission were available in 1413. The 1413 primary PCI-treated AMI patients were classified into quintiles based on PP at hospital admission (mmHg: <40, n = 280; 40–48, n = 276; 49–57, n = 288; 58–70, n = 288; and ≥71, n = 281). Pulse pressure at admission was calculated as the difference between admission systolic blood pressure (SBP) and admission diastolic blood pressure (DBP). Admission SBP and DBP were defined as SBP and DBP first recorded in supine position or sitting position just after presentation to the emergency room or the outpatient clinic. We retrospectively compared clinical background, coronary risk factors, angiographic findings, acute results of primary PCI, and in-hospital prognosis among the five groups. The diagnosis of AMI required the presence of two of the following three criteria: (1) characteristic clinical history, (2) serial changes on the electrocardiogram suggesting infarction (Q-waves) or injury (ST-segment elevations), and (3) transient increase in cardiac enzymes to more than twofold the normal laboratory value.
Data collection
The patients’ demographic information, cardiovascular history, and risk factors (i.e., smoking, hypercholesterolemia, hypertension, and diabetes mellitus) were recorded. Hypercholesterolemia was defined as total cholesterol ≥220 mg/dl or the use of cholesterol-lowering agents; hypertension was defined as systemic blood pressure ≥140/90 mmHg or the use of antihypertensive treatment; diabetes mellitus was defined as fasting blood sugar ≥126 mg/dl or the use of specific treatment. Chronic kidney disease (CKD) was defined as estimated glomerular filtration rate (eGFR) of smaller than 60 ml/min/1.73 m2, and eGFR was calculated using the Japanese equation: eGFR (ml/min/1.73 m2) = 194 × serum creatinine(−1.094) × age(−0.287) × 0.739 (if female) [14]. All in-hospital data were transmitted to the center located at the Department of Cardiovascular Medicine in Kyoto Prefectural University School of Medicine for analysis. The study protocol was approved by each hospital’s ethics committee.
Emergency coronary angiography and reperfusion therapy
Emergency coronary angiography (CAG) was performed using the standard technique. The coronary flow in the infarct-related artery (IRA) was graded according to the classification used in the Thrombolysis in Myocardial Infarction (TIMI) trial. Significant coronary artery stenosis was defined as at least a 75 % reduction in the internal diameter of the right, left anterior descending, or left circumflex coronary arteries and their major branches, or a 50 % reduction in the internal diameter of the left main trunk (LMT). Nonsignificant stenosis was defined as coronary arterial narrowing less than a significant stenosis. Multivessels as culprit lesions was defined as simultaneous thromboses of multiple coronary arteries in the initial CAG. After the culprit lesions were ascertained by CAG, primary PCI was subsequently performed according to standard techniques, with the final decision about the appropriate strategy in each patient left to the judgment of the physician in charge. Primary PCI was defined as a coronary intervention as the initial mode of revascularization therapy, performed at the time of presentation for ST-elevation myocardial infarction (MI) or non-ST-elevation MI including posterior MI, multivessel MI, and LMT-culprit MI, without prethrombolytic therapy.
End-point measures
In-hospital death was defined as all-cause death during the admission period.
Statistics
Data are expressed as mean ± standard deviation (SD). Five groups were compared using the Chi-square test for discrete variables and the Kruskal–Wallis test or one-way analysis of variance (ANOVA), followed by Scheffe’s test as the post hoc test for continuous variables, as appropriate, according to standard statistical methods. The odds ratio and 95 % confidence intervals assessing the risk of in-hospital death were estimated by univariate and multivariate analyses using a logistic regression model. Potent variables with a P value of less than 0.05 on the univariate analyses were entered into a multivariate analysis. In the logistic regression analysis, TIMI flow grade in the IRA was categorized into two groups: grade 3 and grade ≤2 or unknown, and CKD was categorized into two groups: with CKD and without CKD or without eGFR value. In all analyses, statistically significance was accepted at P < 0.05.
Results
Patient characteristics and risk factors
The clinical characteristics and risk factors among the five groups are summarized in Table 1. Age and gender, and frequency of smoking, hypertension, diabetes mellitus, and Killip class ≥3 at admission were significantly different among the five groups. The patients with PP <40 mmHg tended to be male and have lower SBP, lower DBP, lower heart rate, and larger prevalence of smoking and Killip class ≥3 at admission, while the patients with PP ≥71 mmHg had higher age and higher frequency of female, hypertension, and diabetes mellitus.
Angiographic data
Table 2 shows the emergency CAG data for the five groups. The distribution of culprit coronary artery and the number of diseased vessels were significantly different among the five groups. The patients with PP <40 mmHg were more likely to have right coronary artery (RCA), LMT, or multivessels as culprit lesions as well as larger number of diseased vessels or diseased LMT on initial CAG.
Results of coronary intervention
Table 3 shows the results of primary PCI in the five groups. Data on TIMI grade in the IRA were available in 279 of the 280 patients with PP <40 mmHg, 271 of the 276 patients with PP 40–48 mmHg, 283 of the 288 patients with PP 49–57 mmHg, 285 of the 288 patients with PP 58–70 mmHg, and 279 of the 281 patients with PP ≥71 mmHg. The distributions of TIMI grade in the IRA before/after primary PCI were significantly different among the five groups. The patients with PP <40 mmHg tended to have lower TIMI grade in the IRA before/after primary PCI and higher frequency of intra-aortic balloon pumping, percutaneous cardiopulmonary support, and temporary pacing during procedures and/or the admission period.
In-hospital outcomes
Table 4 shows the in-hospital prognoses in the five groups. The patients with lower admission PP were likely to have a higher value of peak creatine phosphokinase (CK) concentration. Patients with PP <40 mmHg had the highest mortality, while patients with PP 49–57 mmHg had the lowest: 11.8 % (<40 mmHg), 7.2 % (40–48 mmHg), 2.8 % (49–57 mmHg), 5.9 % (58–70 mmHg), and 6.0 % (≥71 mmHg) (P < 0.001). The relationship between PP and cardiac-related death was similar to that between PP and all-cause death. Death ascribed to cardiogenic shock and congestive heart failure were common in the patients with PP <40 mmHg. To assess the contribution of clinical background, risk factors, angiographic findings, results of primary PCI, and PP at admission, univariate and multivariate logistic regression analyses were developed for overall death during hospitalization. Potent variables included age, gender, medical history (previous MI, smoking, hypercholesterolemia, hypertension, diabetes mellitus, and CKD), angiographic findings (multivessels or LMT as culprit lesions, and number of diseased vessels ≥2 or diseased LMT), PCI results (TIMI-3 flow before/immediately after primary PCI, and stent usage), Killip class ≥3 at admission, admission SBP, admission DBP, and PP <40 mmHg, PP 40–48 mmHg, PP 49–57 mmHg, PP 58–70 mmHg, or PP ≥71 mmHg at admission. On univariate testing, except for hypertension (P = 0.6545), PP 40–48 mmHg (P = 0.6990), PP 58–70 mmHg (P = 0.5336), and PP ≥71 mmHg (0.6148), all variables mentioned above were associated with in-hospital death. Excluding hypertension, all the available variables described above and admission PP <40 mmHg or admission PP 49–57 mmHg were therefore entered into multivariate models. On multivariate analysis, Killip class ≥3 at admission, LMT or multivessels as culprit lesions, CKD, and age were the independent positive predictors of the in-hospital mortality, whereas admission PP 49–57 mmHg, hypercholesterolemia, and TIMI-3 flow before/after PCI were the negative ones (Table 5A, B). By contrast, admission PP <40 mmHg was not tightly associated with in-hospital death (Table 5B).
Discussion
The major findings of the present multicenter study are as follows. Among AMI patients undergoing primary PCI, patients with PP <40 mmHg had the highest mortality, while patients with PP 49–57 mmHg had the lowest mortality: 11.8 % (<40 mmHg), 7.2 % (40–48 mmHg), 2.8 % (49–57 mmHg), 5.9 % (58–70 mmHg), and 6.0 % (≥71 mmHg) (P < 0.001). On multivariate analysis, Killip class ≥3 at admission, LMT or multivessels as culprit lesions, CKD, and age were the independent positive predictors of the in-hospital mortality, whereas admission PP 49–57 mmHg, hypercholesterolemia, and TIMI-3 flow before/after PCI were the negative ones, but admission PP <40 mmHg was not.
This study is the first to investigate the prognostic impact of PP at admission on in-hospital prognosis among AMI patients undergoing primary PCI. Pulse pressure reflects left ventricular stroke volume, compliance of the aorta and its major branches, and reflected pressure waves [15]. The wide PP with age in healthy population relates to falls in aortic compliance [16], while malignant cycle among high PP, enhanced aortic stiffness, and progression of atherosclerosis has been proposed [15]. High PP enhances vascular endothelial/structural damage, and results in atherosclerosis progression accompanied by increased aortic stiffness, leading to higher PP. In addition, high PP might worsen myocardial ischemia through increased afterload and reduced coronary perfusion [17]. Indeed, numerous studies from the United States and European investigators have demonstrated that wide PP is a significant risk factor for mortality and cardiovascular events in various populations including patients with coronary artery disease [1–7]. However, the relationship between admission PP and in-hospital prognosis in AMI patients undergoing primary PCI remains to be elucidated. A recent report has indicated that initial low PP was associated with in-hospital mortality in patients with acute coronary syndrome, in which CAG was performed only in approximately 20 % of the study population [18]. In the present report concerning the primary PCI-treated AMI patients, the patients with admission PP <40 mmHg had a significantly higher in-hospital mortality rate than other quintiles; however, admission PP <40 mmHg was not an independent predictor of in-hospital death. Interestingly, the patients with PP 49–57 mmHg had the lowest in-hospital mortality rate, and admission PP 49–57 mmHg was an independent predictor of in-hospital survival.
Lower PP on admission tended to be correlated with worse in-hospital prognosis in the present report. Contrary to the relatively stable/chronic conditions such as hypertension, diabetes, and postmyocardial infarction [1–3, 19–21], in which high PP is related to mortality and morbidity, some recent studies have shown that low PP is associated with increased mortality among patients with advanced or decompensated heart failure [8–10] and among patients with heart failure after AMI [11]. In the acute myocardial disorders such as acute heart failure and AMI, lower PP might reflect reduced stroke volume and circulatory impairment rather than decreased arterial stiffness, and lead to increased mortality. Even in the present report, although data regarding left ventricular function were missing, death due to cardiogenic shock or heart failure mainly contribute to higher in-hospital mortality in those patients with lower PP on admission.
On the other hand, the mechanism by which admission PP 49–57 mmHg was tightly associated with better in-hospital outcome remains unclear. Although based on the peak CK value, the extent of myocardial damage was inversely correlated with admission PP; the patients with admission PP 49–57 mmHg had lesser prevalence of deaths ascribed to heart failure and ventricular rupture, compared with the patients with lower PP or those with higher PP. In the present study population, admission PP was positively correlated with admission SBP. Thus, although data regarding SBP and PP during the admission period were missing, there is a possibility that heart failure due to afterload mismatch might be prone to occur in the patients with admission PP ≥71 mmHg. In addition, not only the patients with lower PP characterized by larger myocardial damage but also the patients with higher PP characterized by higher prevalence of hypertension and female gender might be at high risk of ventricular rupture [22, 23]. Another potential explanation is that relatively lesser frequency of admission CKD might account for lower in-hospital mortality in patients with admission PP 49–57 mmHg, because among AMI patients undergoing PCI admission CKD has been shown to be tightly associated with in-hospital mortality as well as 30-day and 1-year mortality [24, 25], while CKD at the first visit to the outpatient clinic after discharge has also been reported to be relevant to long-term prognosis [26].
Study limitations
First, this is a retrospective observational analysis of a relatively small number of patients. Second, data regarding clinical background and angiographic results of primary PCI were not available for the whole study population. Third, we did not have enough detailed data regarding left ventricular function, elapsed time (the time interval between symptom onset and hospital admission), the time interval between blood pressure measurement and subsequent primary PCI, ischemic time, and in-hospital medical treatment, which might be significant predictors of in-hospital death. In particular, antihypertensive treatments in the preadmission period might significantly affect admission PP. Fourth, “ST-elevation MI” was not distinguished from “non-ST-elevation MI”. Fifth, we did not have enough data regarding nonfatal major adverse cardiovascular events during the admission period. Sixth, data concerning an individual decisive factor of primary PCI for the patients with elapsed time >12 h were lacking. Seventh, we did not have enough data about 30-day mortality as end point in the present study population.
Conclusion
The present study suggests that admission PP 49–57 mmHg might be correlated with better in-hospital prognosis among Japanese AMI patients undergoing primary PCI.
References
Benetos A, Rudnichi A, Safar M, Guize L (1998) Pulse pressure and cardiovascular mortality in normotensive and hypertensive subjects. Hypertension 32:560–564
Millar JA, Lever AF, Burke V (1999) Pulse pressure as a risk factor for cardiovascular events in the MRC Mild Hypertension Trial. J Hypertens 17:1065–1072
Blacher J, Staessen JA, Girerd X, Gasowski J, Thijs L, Liu L, Wang JG, Fagard RH, Safar ME (2000) Pulse pressure not mean pressure determines cardiovascular risk in older hypertensive patients. Arch Intern Med 160:1085–1089
Domanski MJ, Sutton-Tyrrell K, Mitchell GF, Faxon DP, Pitt B, Sopko G; Balloon Angioplasty Revascularization Investigation (BARI) (2001) Determinants and prognostic information provided by pulse pressure in patients with coronary artery disease undergoing revascularization. The Balloon Angioplasty Revascularization Investigation (BARI). Am J Cardiol 87:675–679
Mitchell GF, Moyé LA, Braunwald E, Rouleau JL, Bernstein V, Geltman EM, Flaker GC, Pfeffer MA (1997) Sphygmomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after myocardial infarction in patients with impaired left ventricular function. SAVE investigators. Survival and Ventricular Enlargement. Circulation 96:4254–4260
Benetos A, Safar M, Rudnichi A, Smulyan H, Richard JL, Ducimetieère P, Guize L (1997) Pulse pressure: a predictor of long-term cardiovascular mortality in a French male population. Hypertension 30:1410–1415
Franklin SS, Khan SA, Wong ND, Larson MG, Levy D (1999) Is pulse pressure useful in predicting risk for coronary heart disease? The Framingham Heart Study. Circulation 100:354–360
Aronson D, Burger AJ (2004) Relation between pulse pressure and survival in patients with decompensated heart failure. Am J Cardiol 93:785–788
Voors AA, Petrie CJ, Petrie MC, Charlesworth A, Hillege HL, Zijlstra F, McMurray JJ, van Veldhuisen DJ (2005) Low pulse pressure is independently related to elevated natriuretic peptides and increased mortality in advanced chronic heart failure. Eur Heart J 26:1759–1764
Petrie CJ, Voors AA, van Veldhuisen DJ (2009) Low pulse pressure is an independent predictor of mortality and morbidity in non ischaemic, but not in ischaemic advanced heart failure patients. Int J Cardiol 131:336–344
Petrie CJ, Voors AA, Robertson M, van Veldhuisen DJ, Dargie HJ (2012) A low pulse pressure predicts mortality in subjects with heart failure after an acute myocardial infarction: a post hoc analysis of the CAPRICORN study. Clin Res Cardiol 101:29–35
Kallistratos MS, Poulimenos LE, Pavlidis AN, Dritsas A, Laoutaris ID, Manolis AJ, Cokkinos DV (2012) Prognostic significance of blood pressure response to exercise in patients with systolic heart failure. Heart Vessels 27:46–52
Shiraishi J, Kohno Y, Sawada T, Ito D, Kimura M, Ariyoshi M, Matsui A, Arihara M, Irie H, Hyogo M, Shima T, Nakamura T, Matoba S, Yamada H, Matsumuro A, Shirayama T, Kitamura M, Furukawa K, Matsubara H (2011) Systolic blood pressure at admission, clinical manifestations, and in-hospital outcomes in patients with acute myocardial infarction. J Cardiol 58:54–60
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A; Collaborators developing the Japanese equation for estimated GFR (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992
Dart AM, Kingwell BA (2001) Pulse pressure—a review of mechanisms and clinical relevance. J Am Coll Cardiol 37:975–984
Franklin SS, Gustin W 4th, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D (1997) Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation 96:308–315
Watanabe H, Ohtsuka S, Kakihana M, Sugishita Y (1993) Coronary circulation in dogs with an experimental decrease in aortic compliance. J Am Coll Cardiol 21:1497–1506
El-Menyar A, Zubaid M, Almahmeed W, Alanbaei M, Rashed W, Al Qahtani A, Singh R, Zubair S, Al Suwaidi J (2011) Initial hospital pulse pressure and cardiovascular outcomes in acute coronary syndrome. Arch Cardiovasc Dis 104:435–443
Schram MT, Kostense PJ, Van Dijk RA, Dekker JM, Nijpels G, Bouter LM, Heine RJ, Stehouwer CD (2002) Diabetes, pulse pressure and cardiovascular mortality: the Hoorn Study. J Hypertens 20:1743–1751
Nakano S, Konishi K, Furuya K, Uehara K, Nishizawa M, Nakagawa A, Kigoshi T, Uchida K (2005) A prognostic role of mean 24-h pulse pressure level for cardiovascular events in type 2 diabetic subjects under 60 years of age. Diabetes Care 28:95–100
Avanzini F, Alli C, Boccanelli A, Chieffo C, Franzosi MG, Geraci E, Maggioni AP, Marfisi RM, Nicolosi GL, Schweiger C, Tavazzi L, Tognoni G, Valagussa F, Marchioli R; GISSI-Prevenzione investigators (2006) High pulse pressure and low mean arterial pressure: two predictors of death after a myocardial infarction. J Hypertens 24:2377–2385
Wehrens XH, Doevendans PA (2004) Cardiac rupture complicating myocardial infarction. Int J Cardiol 95:285–292
Yip HK, Wu CJ, Chang HW, Wang CP, Cheng CI, Chua S, Chen MC (2003) Cardiac rupture complicating acute myocardial infarction in the direct percutaneous coronary intervention reperfusion era. Chest 124:565–571
Hanna EB, Chen AY, Roe MT, Wiviott SD, Fox CS, Saucedo JF (2011) Characteristics and in-hospital outcomes of patients with non-ST-segment elevation myocardial infarction and chronic kidney disease undergoing percutaneous coronary intervention. JACC Cardiovasc Interv 4:1002–1008
Mehran R, Nikolsky E, Lansky AJ, Kirtane AJ, Kim YH, Feit F, Manoukian S, Moses JW, Ebrahimi R, Ohman EM, White HD, Pocock SJ, Dangas GD, Stone GW (2009) Impact of chronic kidney disease on early (30-day) and late (1-year) outcomes of patients with acute coronary syndromes treated with alternative antithrombotic treatment strategies: an ACUITY (Acute Catheterization and Urgent Intervention Triage strategY) substudy. JACC Cardiovasc Interv 2:748–757
Matsue Y, Matsumura A, Abe M, Ono M, Seya M, Nakamura T, Iwatsuka R, Mizukami A, Setoguchi M, Nagahori W, Ohno M, Suzuki M, Hashimoto Y (2011) Prognostic implications of chronic kidney disease and anemia after percutaneous coronary intervention in acute myocardial infarction patients. Heart Vessels. doi:10.1007/s00380-011-0209-2
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the AMI-Kyoto Multi-Center Risk Study Group. The institutions and principal investigators of AMI-Kyoto Multi-Center Risk Study Group are listed in the Appendix.
Appendix
Appendix
The following institutions and principal investigators participated in the present study as the AMI-Kyoto Multi-Center Risk Study Group. Kyoto City Hospital: Okada T, Shima M, Takamiya A, Nakajima N, Matsunaga S; Kyoto Kidugawa Hospital: Miyanaga H, Nakagawa T, Matsui H, Kunieda Y; Kyoto Second Red Cross Hospital: Fujita H, Inoue K, Matsuo A, Kimura S, Sakatani T, Isodono K, Tsubakimoto Y; Social Insurance Kyoto Hospital: Yamada C, Tanabe S, Yagi T; Tanabe Central Hospital: Kusuoka S, Takechi N, Nishizawa S; Nantan General Hospital: Tatsumi T, Keira N, Nomura T; Ayabe Municipal Hospital: Shiga K, Kohno Y, Adachi Y; Maizuru Medical Center: Harada Y, Hikosaka T, Nakagami T; Kyoto Saiseikai Hospital: Yamahara Y, Ishibashi K, Takeda M; Gakkentoshi Hospital: Sakai R, Akashi K; Kouseikai Takeda Hospital: Matsumoto K, Kinoshita N, Sawanishi T, Nakamura R; Kameoka Municipal Hospital: Matsuo R; Aiseikai Yamashina Hospital: Yamamoto T; Fukuchiyama Municipal Hospital: Nishio M, Sakamoto T; Saiseikai Shiga Hspital: Nakamura T, Nakahara Y, Kurata H, Hadase M; Omihachiman Community Medical Center: Maki K, Tatsukawa H, Zen K, Kambayashi D; Kyoto Prefectural Yosanoumi Hospital: Honsho S; Kyoto Prefectural University School of Medicine: Shiraishi H, Yamano T.
Rights and permissions
About this article
Cite this article
Shiraishi, J., Kohno, Y., Sawada, T. et al. Prognostic impact of pulse pressure at admission on in-hospital outcome after primary percutaneous coronary intervention for acute myocardial infarction. Heart Vessels 28, 434–441 (2013). https://doi.org/10.1007/s00380-012-0277-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-012-0277-y