Abstract
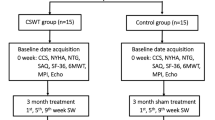
Our aim was to evaluate the safety and effectiveness of extracorporeal cardiac shock wave therapy (CSWT) for the patients with coronary heart disease (CHD) using a randomized, double-blind, controlled clinical trial design. Twenty-five patients with CHD were enrolled in this study. Fourteen of the patients were randomized into the CSWT group and 11 into the control group. We applied the CSWT procedure to each patient by using nine shock treatments during 3 months, but the shock wave (SW) energy was only applied to the patients in the CSWT group and not to the patients in the control group. Technetium-99m sestamibi myocardial perfusion, fluorine-18 fluorodeoxyglucose myocardial metabolism single-photon emission computed tomography (SPECT), and two-dimensional echocardiography were performed to identify segments of myocardial ischemia, myocardial viability, and ejection fraction before and after CSWT. We also followed the patients to evaluate adverse effects. After CSWT, the New York Heart Association class, the Canadian Cardiovascular Society angina scale, nitroglycerin dosage, myocardial perfusion and myocardial metabolic imaging scores of dual-isotope SPECT in the CSWT group were reduced significantly (P = 0.019, 0.027, 0.039, 0.000, 0.001, respectively), and the Seattle Angina Questionnaire scale, 6-min walking test, and left ventricular ejection fraction were increased significantly (P = 0.021, 0.024, 0.016, respectively) compared with those before the SW treatment. All of the parameters in the control group did not change significantly after the treatment (all P > 0.05). No serious adverse effects of CSWT were observed. Cardiac shock wave therapy is a safe and effective treatment for CHD patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary heart disease (CHD) is the leading cause of death in the world [1, 2]. Besides medication, percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) have been the major current therapeutic options for CHD. These therapies have some limitations; moreover, PCI and CABG cannot be performed in many patients with severe CHD for technical and economic reasons, especially in developing countries. The prognosis for these patients is very poor. The newly developed technology of cardiac shock wave therapy (CSWT) brings forth a new option for severe CHD, and has been termed the third “sword” of CHD treatment. In recent years, a series of in vitro, animal, and clinical studies showed that low-energy pulse waves produced by CSWT could induce a “cavitation effect” (micrometer-sized violent collapse of bubbles within and outside cells), which could exert a mechanical shear force on the myocardial tissue and vascular endothelial cell membranes [3–11]. The CSWT was able to promote angiogenesis in ischemic myocardium, improve myocardial perfusion, and increase capillary density (about 10 % of energy density that used for urolithiasis) by upregulating vascular endothelial growth factor (VEGF) and its receptor fms-like tyrosine 1 [5, 6]. This increases expression of endothelial nitric oxide synthase (NOS), stromal-derived factor 1 (SDF-1), insulin-like growth factor (IGF), and interleukin-8 (IL-8) [12–14], resulting in an increase of left ventricular ejection fraction (LVEF) and improvement of left ventricular remodeling [15]. Angina can thus be reduced [7, 10, 16].
To investigate the feasibility, safety, and efficacy of CSWT. We designed and carried out a randomized and double-blind controlled study of CSWT. In this study 25 patients with severe CHD were selected who were randomly divided into the CSWT group of 14 patients receiving CSWT, and the control group of 11 patients who did not receive the treatment. Myocardial perfusion, myocardial metabolism, symptoms of angina, and cardiac function between the two groups were investigated.
Patients and methods
Patients
This study was approved by and performed in accordance with the rules of the ethics committee of our hospital. Informed written consent was obtained from each patient prior to enrollment. All 25 patients had suffered prior myocardial infarction (MI). There were 18 men and 7 women, aged from 47 to 79 years (64.92 ± 8.50 years). All of the selected patients had been admitted to the cardiology department of the 1st Affiliated Hospital of Kunming Medical College, China, from October 2008 to June 2010. The patients were randomly divided into two groups. Fourteen patients were in the CSWT group, 10 male and 4 female, aged from 47 to 78 years (63.71 ± 8.60 years) and 11 patients were in the control group, 8 male and 3 female, aged from 50 to 79 years (66.45 ± 8.51 years). All of the patients selected in this study had been diagnosed definitely as having suffered at least one acute myocardial infarction (AMI) and had not been treated with coronary revascularization (thrombolysis, PCI, or CABG) because of lack of indication (n = 19), poor economic conditions (n = 4), technical limitations (n = 1) and religion that does not accept invasive or surgical procedure (n = 1). Although all of the patients had received standard medical treatment, they all still suffered from angina and poor exercise tolerance, and had been hospitalized more than two times due to myocardial ischemia within 1 year. The basic characteristics of the patients are shown in Table 1. The exclusion criteria of this study included a myocardial infarction within the past 3 months, cardiac thrombus, chronic obstructive pulmonary disease (COPD), pulmonary embolism, New York Heart Association (NYHA) heart function IV, and malignancy.
Localization of myocardial ischemia and viability
The dual-isotope single-photon emission computed tomography (SPECT) of technetium-99m sestamibi (99mTc-MIBI) myocardial perfusion and fluorine-18-fluorodeoxyglucose (18F-FDG) myocardial metabolism were performed in all of the selected patients (Discovery VH Millennium; General Electric, Fairfield, CT, USA) to identify areas of myocardial ischemia and viability. According to the standard recommended by the American Heart Association (AHA), the left ventricle was divided into 17 segments to analyze the myocardial perfusion and metabolism [17], and then to evaluate the myocardial viability. The images were read blindly by two doctors in the Nuclear Medicine Department. Isotope uptake of myocardial perfusion and metabolism were evaluated by semiquantitative score index [18]: 1, normal; 2, sparse; 3, seriously sparse; 4, defect. Myocardial viability was evaluated by SPECT. The myocardium would be identified as viable with the criteria: for 99mTc-MIBI and 18F-FDG uptake score ≤2, or 99mTc-MIBI uptake score increase ≥1 compared with 18F-FDG (myocardial perfusion seriously sparse or defect, but myocardial metabolism well, which means the perfusion and metabolism are mismatched). All radioactive scores of perfusion and metabolism imaging of 17 myocardial segments were added to obtain the total scores of perfusion and metabolic imaging of each patient, which reflected the level of myocardial perfusion and metabolism.
Cardiac shock wave therapy procedure
The CSWT was performed for all patients with a CSWT device (Modulith SLC; Storz Medical, Taegerwilen, Switzerland), which was installed with a real-time ultrasound probe (Fig. 1). In the CSWT procedure, the patients were resting quietly in the supine position. Electrocardiographic data, blood pressure, respiration, and blood oxygen saturation were monitored continuously. The target myocardial regions (ischemic area with some viable segments identified by SPECT) were located by the ultrasound probe. The shock wave (SW) was applied in an R-wave-triggered manner to avoid inducing ventricular arrhythmias. The SW energy was applied and gradually increased in the patients of the CSWT group. The maximum SW energy was 0.09 mJ/mm2. Patients in the control group were also placed in the supine position but no SW energy was applied. Each ischemic target region was treated at nine points, 200 shocks/spot, three times a week, during the first week of each month on the first, third, and fifth day serially. In the course of 3 months, nine CSWT procedures were performed in all of the patients [6, 7, 17]. The patients in the CSWT group were treated with SW energy, but the patients in the control group were treated without SW energy. During the treatment, the patients were closely monitored for adverse effects.
Echocardiography evaluation
The echocardiographic tests were performed on all of the patients before and 1 month after CSWT treatment using a ViViD7 (General Electric) with 2.5-MHz probe frequency. The modified biplane Simpson method was used to measure the LVEF, using the two-dimensional long-axis view of the left ventricle.
Clinical assessment parameters
The effect of CSWT was assessed by the NYHA class, Canadian Cardiovascular Society (CCS) angina scale, Seattle Angina Questionnaire (SAQ) scale, 6-min walking test (6MWT), nitroglycerin dosage, rehospitalization rate, and mortality.
Analysis of cardiac enzymes
The serum concentrations of creatine kinase (CK), MB isoenzyme of creatine kinase (CK-MB), and cardiac troponin I (CTNI) were measured by the chemiluminescence immunoassay (Advia Centaur CP; Siemens, Munich, Germany) before and the day after CSWT.
Clinical follow-up
All of the patients were followed for 6 months after the last CSWT treatment by outpatient review, hospitalization review, and phone tracking. During the follow-up, if the condition of the patients was confirmed not to have improved or to have deteriorated, standard therapy was applied.
Statistical analysis
Continuous variables are expressed as mean ± SD and categorical variables are expressed as percentages. Nonparametric variables are expressed as the median (interquartile range). The comparison between groups was done by t and χ 2 tests. The pretreatment and post-treatment values were compared by paired t test or Wilcoxon signed-rank test. Statistical analyses were performed with SPSS 15.0 (SPSS, Chicago, IL, USA), All statistical tests were two sided, and a P value of less than 0.05 was considered to be statistically significant.
Results
Comparison of characteristics of the two groups
The mean age, gender, time since last MI, body mass index (BMI), history of smoking, hypertension, diabetes, hypercholesterolemia, and medication use for CHD in the two groups were not significantly different (Table 1). All of the patients had completed the nine treatments of CSWT and were followed successfully. Prior to the treatment, one patient in the CSWT group had sinus bradycardia (average heart rate = 42 beats/min and with sinus arrest for the longest P–P interval of 3.2 s). After six treatments of CSWT the sinus arrest disappeared and sinus bradycardia improved (mean heart rate 57 beats/min). No sinus arrest was observed during follow-up. Occasional premature ventricular contractions were observed in one patient in the CSWT group when the CSWT treatment started. As the CSWT treatment progressed, the premature contractions gradually disappeared. Mild chest pain appeared in two patients when the SW energy was increased during CSWT, and the chest pain was relieved when the SW energy was decreased. There was no increase in angina during the treatment or follow-up. No heart failure, hemorrhage, embolism, malignant arrhythmia (ventricular tachycardia/fibrillation), skin ulceration, or other complications were observed. The monitoring showed that the CSWT had no significant effect on blood pressure, heart rate, and arterial blood oxygen saturation.
Comparison of mortality and rehospitalization rate
During the follow-up (average = 8.40 ± 1.84 months), no patient died in the control group, and one patient in the CSWT group died secondary to ventricular fibrillation and hypokalemia. This patient had acute severe diarrhea prior to death. Seven patients were hospitalized for frequent angina: five in the control group and two in the CSWT group. The mortality and rehospitalization rates of the two groups were not different significantly (P = 0.177, 1.000, respectively).
Comparison of clinical parameters
Prior to the SW treatment, there were no significant group differences in any of the clinical variables (NYHA class, CCS angina, SAQ scale, 6MWT, nitroglycerine dosage, all P > 0.05, Table 2). In the first month after nine treatments with the CSWT, NYHA class, CCS angina scale, and nitroglycerin dosage in the CSWT group were decreased significantly (P = 0.019, 0.027, 0.039, respectively), and the SAQ scale and 6MWT were increased significantly (P = 0.021, 0.024, respectively) compared with pre-CSWT treatment. There was no significant change in any of these parameters in the control group (all P > 0.05). Compared with the control group, all the clinical parameters in the CSWT group improved significantly following the SW treatment (all P < 0.05, Table 2).
Comparison of cardiac enzymes
Serum CK (IU/l), CK-MB (IU/l), and CTNI (ng/ml) were not significantly different before and after treatment in the CSWT group (75.93 ± 17.85 vs 74.43 ± 16.39, P = 0.819; 8.36 ± 3.48 vs 8.51 ± 3.24, P = 0.906; 0.06 ± 0.03 vs 0.07 ± 0.02, P = 0.440) or in the control group (80.81 ± 14.21 vs 78.53 ± 13.03, P = 0.699; 8.67 ± 2.74 vs 8.83 ± 3.17, P = 0.904; 0.05 ± 0.03 vs 0.06 ± 0.03, P = 0.413).
Comparison of echocardiography
Prior to the SW treatment, there were no significant differences in left ventricular end-diastolic dimension (LVEDD) (mm) and LVEF (%) between the CSWT group and control group (both P > 0.05). Both LVEDD and LVEF in the CSWT group were improved significantly after the SW treatment compared with the control group (both P < 0.05). After treatment, there was a nonsignificant decrease in LVEDD (P = 0.399) and a significant increase in LVEF (P = 0.016) in the CSWT group compared with pretreatment. In the control group there was no significant change for LVEDD and LVEF before and after the SW treatment (both P > 0.05, Table 3).
Comparison of dual-isotope SPECT test results of the two groups
Dual-isotope myocardial SPECT tests were performed in all 25 patients before and in the first month after the SW treatment. The tests showed that before the SW treatment, 14 patients in the CSWT group had 73 of 238 segments with metabolic disorders (30.7 %) and 95 with ischemia (40.0 %). Sixty-four of the 95 ischemic segments had viable myocardium (67.4 %). Eleven patients in the control group had 64 of 187 myocardial segments with metabolic disorders (34.2 %) and 79 with ischemia (42.2 %). Fifty-five of 79 ischemic segments had viable myocardium (69.6 %). One month after treatment, there were 47 metabolic disorder segments (19.7 %) and 66 ischemic segments (27.7 %) in the CSWT group. Fifty-six of the 66 ischemic segments had viable myocardium (84.8 %) (Fig. 2). In the control group, there were 69 metabolic disorders segments (36.9 %) and 85 ischemic segments (45.5 %). Fifty-five of the 85 ischemic segments had viable myocardium (64.7 %). Before treatment, there was no significant difference for the myocardial perfusion and metabolic imaging scores between the CSWT group and the control group (both P > 0.05). Both radioactive scores in the CSWT group were reduced significantly after the SW treatment compared with the control group (both P < 0.05, Table 4). Compared with scores prior to treatment, the post-treatment myocardial perfusion and metabolic imaging scores of the patients in the CSWT group were decreased significantly (P = 0.000, 0.001, respectively). These scores were not changed significantly after treatment in the control group (both P > 0.05, Table 4).
Images of the dual-isotope SPECT of 99mTc-MIBI myocardial perfusion and 18F-FDG myocardial metabolism. Before CSWT (a), the image shows a matched abnormal myocardial perfusion and myocardial metabolism in the left apex, inferior wall, and posterior wall (both myocardial perfusion and myocardial metabolism scores are 4), suggesting there is no myocardial cell survival. In the lateral wall, the myocardial perfusion and metabolism are mismatched (myocardial perfusion score is 3 but myocardial metabolism score is 2), meaning that in the area with myocardial necrosis there is still some viable myocardium. The myocardial perfusion in the anterior wall and septum is normal. After CSWT (b), the image shows that the uptake of 99mTc-MIBI and 18F-FDG in left apex and posterior-lateral wall, which indicates both of the myocardial perfusion and metabolism in that location, have been improved by the SW treatment. There is an obvious uptake of 99mTc-MIBI in the inferior wall compared with the last test, but the 18F-FDG uptake is not present. This is favorable in that the myocardial perfusion is improved, so that the myocardial cell could use fat mainly in the metabolism but not FDG, therefore both myocardial perfusion and metabolism may be improved by CSWT
Discussion
Our research started tests on the CSWT device in 2008. We have since evaluated this method in vitro, in animal experiments, and in initial clinical studies. All of this research has supported the effectiveness of CSWT [10, 19–21]. Cai et al. confirmed that CSWT could be helpful to the mobilization of endothelial progenitor cells and increase the expression of VEGF and its receptors [20]; Tao et al. [21] found that in porcine AMI, the SW treatment could promote angiogenesis and benefit ventricular remodeling. Wang and other experts did research on CHD patients, which showed CSWT could relieve angina, improve heart function, and increase exercise tolerance [10, 19]. On the basis of the preliminary studies, we attempted this prospective, double-blind controlled clinical experiment to investigate the effectiveness and safety of CWST in CHD patients having suffered a prior MI. To obtain objective data, we used echocardiography and dual-isotope myocardial SPECT before and after treatment in an CSWT and a control group. The treatment of SW was simple and noninvasive, without surgery, anesthesia, or even catheter intervention. During and after the SW treatment, the cardiac enzyme was not changed significantly and no procedural complications or adverse effects were observed in the CSWT group. This suggests that the SW treatment cannot cause any myocardial injury, and that it is safe and can be used repeatedly in CHD management.
A number of studies have confirmed that it is highly specific and sensitive to detect the viable myocardium for the patients with MI using 99mTc-MIBI and 18F-FDG myocardial SPECT imaging [22, 23]. 99mTc-MIBI and 18F-FDG myocardial SPECT reflects myocardial perfusion and metabolism, respectively. When 99mTc-MIBI imaging shows reduction in perfused segments of blood flow, while the 18F-FDG imaging shows the corresponding segments have normal or relatively increased FDG uptake (perfusion and metabolism are mismatched), this indicates that the myocardium is ischemic but viable. On the contrary, in the segments with irreversible injury, both the blood flow perfusion and myocardial glucose utilization (FDG uptake reduced) are reduced simultaneously (perfusion and metabolism are matched). This indicates that there is no survival of myocardial cells, but myocardial scarring and necrosis. In this study, the semiquantitative evaluation of myocardial perfusion and metabolism based on 99mTc-MIBI and 18F-FDG dual-isotope SPECT imaging was used in all of the patients. We used the ischemic myocardial segments with some viability as the target area for the SW treatment in order to obtain the maximal efficacy of CSWT. Comparing the total score of myocardial perfusion and metabolism imaging of the patients before and after the SW treatment, we were able to assess the effect of CSWT objectively. The results of our study showed that both the myocardial perfusion and myocardial metabolism could be improved significantly by CSWT.
During the 8-month follow-up period, mortality and rehospitalization rates of the two groups were not different. This may have been due to the small sample size and the relatively short period of follow-up. The results of our study showed that after the SW treatment, angina symptoms of the patients who had been treated with the SW were alleviated compared with the patients in the control group, who had not been treated with the SW. Moreover, both cardiac function and exercise tolerance of the patients treated by the real SW were improved significantly. These results are consistent with those of the double-blind study of CSWT reported by Japanese experts [16]. During follow-up, no significant change of the LVEDD was observed after the SW treatment in the CSWT group. The lack of significant reduction in LVEDD may also be related to the small sample size and short duration of follow-up, or to the long history of OMI (averaged duration of MI for 5.0 years), so that the ventricular remodeling might have been irreversible. The LVEF of the patients was improved significantly after the SW treatment but was not changed significantly in the control patients, which suggests that the SW treatment improves perfusion and metabolism of ischemic myocardium, so that myocardial contractive function can also be improved significantly.
Conclusion
This double-blind controlled clinical trial shows that CSWT is a noninvasive, safe, and effective treatment for CHD patients. After SW treatment, the clinical condition, perfusion, and metabolism of the ischemic myocardium and myocardial contractive function of the CHD patients were improved significantly and no complications from the CSWT procedure were observed. Although there are some limitations in this study, such as a small sample size and a relatively short follow-up period, the results are encouraging and suggestive that longer and larger studies are needed.
References
Iwasaki K, Matsumoto T, Aono H, Furukawa H, Nagamachi K, Samukawa M (2010) Distribution of coronary atherosclerosis in patients with coronary artery disease. Heart Vessels 25:14–18
Kayrak M, Bacaksiz A, Ulgen MS, Vatankulu MA, Zengin K, Ayhan SS, Basaral MK, Büyükbas S, Kiyici A (2011) Plasma concentrations of soluble CD40 ligand in smokers with acute myocardial infarction: a pilot study. Heart Vessels 26:131–137
Ichioka S, Shibata M, Kosaki K, Sato Y, Harii K, Kamiya A (1997) Effects of shear stress on wound healing angiogenesis in the rabbit ear chamber. J Surg Res 72:29–35
Fisher AB, Chien S, Barakat AI, Nerem RM (2001) Endothelial cellular response to altered shear stress. Am J Physiol Lung Cell Mol Physiol 281:L529–L533
Nishida T, Shimokawa H, Oi K, Tatewaki H, Uwatoku T, Abe K, Matsumoto Y, Kajihara N, Eto M, Matsuda T, Yasui H, Takeshita A, Sunaqawa K (2004) Extracorporeal cardiac shock wave therapy markedly ameliorates ischemia induced myocardial dysfunction in pigs in vivo. Circulation 110:3055–3061
Gutersohn A, Gaspari G (2000) Shock waves upregulate vascular endothelial growth factor m-RNA in human umbilical vascular endothelial cells. Circulation 102(suppl):1–18
Fukumoto Y, Ito A, Uwatoku T, Matoba T, Kishi T, Tanaka H, Takeshita A, Sunaqawa K, Shimokawa H (2006) Extracorporeal cardiac shock wave therapy ameliorates myocardial ischemia in patients with severe coronary artery disease. Coron Artery Dis 17:63–70
Khattab AA, Brodersen B, Schuermann-Kuchenbrandt D, Beurich H, Tölg R, Geist V, Schäfer T, Richardt G (2007) Extracorporeal cardiac shock wave therapy: first experience in the everyday practice for treatment of chronic refractory angina pectoris. Int J Cardiol 121:84–85
Ito K, Fukumoto Y, Shimokawa H (2009) Extracorporeal shock wave therapy as a new and non-invasive angiogenic therapy. Tohoku J Exp Med 219:1–9
Wang Y, Guo T, Cai HY, Ma TK, Tao SM, Sun S, Chen MQ, Gu Y, Pang JH, Xiao JM, Yang XY, Yang C (2010) Cardiac shock wave therapy reduces angina and improves myocardial function in patients with refractory coronary artery disease. Clin Cardiol 33:693–699
Vasyuk YA, Hadzegova AB, Shkolnik EL, Kopeleva MV, Krikunova OV, Iouchtchouk EN, Aronova EM, Ivanova SV (2010) Initial clinical experience with extracorporeal shock wave therapy in treatment of ischemic heart failure. Congest Heart Fail 16:226–230
Mariotto S, Cavalieri E, Amelio E, Ciampa AR, de Prati AC, Marlinghaus E, Russo S, Suzuki H (2005) Extracorporeal shock waves: from lithotripsy to anti-inflammatory action by NO production. Nitric Oxide 12:89–96
Ciampa AR, de Prati AC, Amelio E, Cavalieri E, Persichini T, Colasanti M, Musci G, Marlinghaus E, Suzuki S, Mariotto S (2005) Nitric oxide mediates anti-inflammatory action of extracorporeal shock waves. FEBS Lett 579:6839–6845
Oi K, Fukumoto Y, Ito K, Uwatoku T, Abe K, Hizume T, Shimokawa H (2008) Extracorporeal shock wave therapy ameliorates hindlimb ischemia in rabbits. Tohoku J Exp Med 214:151–158
Uwatoku T, Ito K, Abe K, Oi K, Hizume T, Sunagawa K, Shimokawa H (2007) Extracorporeal cardiac shock wave therapy proves left ventricular remodeling after acute myocardial infarction in pigs. Coron Artery Dis 18:397–404
Kikuchi Y, Ito K, Ito Y, Shiroto T, Tsuburaya R, Aizawa K, Hao K, Fukumoto Y, Takahashi J, Takeda M, Nakayama M, Yasuda S, Kuriyama S, Tsuji I, Shimokawa H (2010) Double-blind and placebo-controlled study of the effectiveness and safety of extracorporeal cardiac shock wave therapy for severe angina pectoris. Circ J 74:589–591
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS (2002) American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the cardiac imaging committee of the Council on Clinical Cardiology of the American Heart Association. J Nucl Cardiol 9:240–245
Fang LG, Li J, Chen LB, Li F, Chen W, Fang Q (2009) Comparison of low-dose adenosine echocardiography and dual-isotope emission simultaneous acquisition for assessment of myocardial viability in early acute myocardial infarction. J Clin Cardiol (China) 25:623–626
Wang Y, Guo T, Cai HY, Ma TK, Tao SM, Chen MQ, Gu Y, Pan JH, Xiao JM, Zhao L, Yang XY, Yang C (2010) Extracorporeal cardiac shock wave therapy for treatment of coronary artery disease. Chin J Cardiol 38:711–715
Cai HY, Wang Y, Li L, Zhao L, Xiao JM, Cao JM, Yang XY, Yang C, Guo T (2010) Changes in the number of endothelial progenitor cells from peripheral blood in patients with coronary atherosclerotic heart disease before and after extracorporeal cardiac shock wave therapy. J Clin Rehabil Tissue Eng Res (China) 14:9249–9252
Tao SM, Gao T, Wang Y, Cai HY, Yang C (2011) Extracorporeal cardiac shock wave therapy improved myocardial micro-vascular circulation after acute myocardial infarction at early stage in pigs. J Sichuan Univ (Med Sci Edi) 42:222–226
Matsunari I, Kanayama S, Yoneyama T, Matsudaira M, Nakajima K, Taki J, Nekolla SG, Tonami N, Hisada K (2005) Electrocardiographic gated dual isotope simultaneous acquisition SPECT using 18F-FDG and 99mTc-sestamibi to assess myocardial viability and function in a single study. Eur J Nucl Med Mol Imaging 32:195–202
Slart RH, Bax JJ, de Boer J, Willemsen AT, Mook PH, Oudkerk M, Van der wall EE, Van Veld Huison DJ, Jaqer PL (2005) Comparison of 99mTc-sestamibi/18FDG DISA SPECT with PET for the detection of viability in patients with coronary artery disease and left ventricular dysfunction. Eur J Nucl Med Mol Imaging 32:972–979
Acknowledgments
We thank Dr Ernest H. Marlingghaus, Storze Medical AG, Switzerland and Kenta Ito, Department of Cardiovascular Medicine, Tohoku University Graduate School of Medicine, Japan, for their valuable help and comments to our study. This study was supported by the 1st Affiliated Hospital of Kunming Medical College, Kunming, Yunnan, China.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, P., Guo, T., Wang, W. et al. Randomized and double-blind controlled clinical trial of extracorporeal cardiac shock wave therapy for coronary heart disease. Heart Vessels 28, 284–291 (2013). https://doi.org/10.1007/s00380-012-0244-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-012-0244-7