Abstract
Independent no-reflow predictors should be evaluated in female patients with ST-segment elevation acute myocardial infarction (STEMI) and successfully treated with primary percutaneous coronary intervention (PPCI) in the current interventional equipment and techniques, thus to be constructed a no-reflow predicting model. In this study, 320 female patients with STEMI were successfully treated with PPCI within 12 h after the onset of AMI from 2007 to 2010. All clinical, angiographic, and procedural data were collected. Multiple logistic regression analysis was used to identify independent no-reflow predictors. The no-reflow was found in 81 (25.3%) of 320 female patients. Univariate and multivariate stepwise logistic regression analysis identified that low SBP on admission <100 mmHg (OR 1.991, 95% CI 1.018–3.896; p = 0.004), target lesion length >20 mm (OR 1.948, 95% CI 1.908–1.990; p = 0.016), collateral circulation 0–1 (OR 1.952, 95% CI 1.914–1.992; p = 0.019), pre-PCI thrombus score ≥4 (OR 4.184, 95% CI 1.482–11.813; p = 0.007), and IABP use before PCI (OR 1.949, 95% CI 1.168–3.253; p = 0.011) were independent no-reflow predictors. The no-reflow incidence significantly increased as the numbers of independent predictors increased [0% (0/2), 10.8% (9/84), 14.5% (17/117), 37.7% (29/77), 56.7% (17/30), and 81.8% (9/11) in female patients with 0, 1, 2, 3, 4, and 5 independent predictors, respectively; p < 0.0001]. The five no-reflow predicting variables were admission SBP <100 mmHg, target lesion length >20 mm, collateral circulation 0–1, pre-PCI thrombus score ≥4, and IABP use before PCI in female patients with STEMI treated with PPCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women differ from men with respect to coronary artery disease epidemiology, symptomatology, pathophysiology, and outcome [1]. PPCI is currently the most effective treatment strategy in acute myocardial infarction (AMI) in women as well as in men [2]. Nevertheless, several studies showed that higher frequency of angiographic no-reflow or slow reflow and higher mortality occurred in women than in men [3, 4]. Furthermore, recent studies showed that female sex was an independent predictor of mortality following AMI [5]. With the current practice to increase use of drug-eluting stents and glycoprotein receptor antagonists as well as shorter delay in the timing of coronary intervention, this study was undertaken to identify independent predictors for no-reflow after PPCI in female patients with STEMI in the contemporary clinical practice.
Materials and methods
Patients
This study is a prospective observational study conducted at two medical institutions. Between January 2007 and January 2010, 320 consecutive female patients who were admitted within 12 h after the onset of STEMI were enrolled (1,093 male patients during the same enrollment period). All patients signed the informed consent forms. STEMI was defined as the presence of new ST elevation at the J-point in two contiguous leads with the cut-off points: ≥0.2 mV in men or ≥0.15 mV in women in leads V2–V3 and/or ≥0.1 mV in other leads, or presumed new left bundle-branch block, and creatine kinase-MB (CK-MB) >1 times normal in patients who had prolonged chest pain lasting ≥30 min. Cardiac symptoms lasting >30 min that occurred within 48 h before the onset of infarction were defined as pre-infarction angina.
Maximum creatine kinase-MB were determined from blood samples obtained every 4 h following PPCI. The creatinine clearance (CrCl) was calculated by applying the Cockcroft–Gault formula [6].
Coronary angiography and PPCI
All patients underwent coronary angiography using a common technique. Angiograms were analyzed using a validated quantitative coronary angiographic system (MEDIS, CMS 4.0, Leiden, The Netherlands).
All patients received oral aspirin (300 mg) and clopidogrel (300 mg) immediately after admission and intravenous heparin (5000 U) before PCI. The allocation of coronary angiography and reperfusion therapy was determined by physician’s decision. All patients were successfully implanted drug-eluting stents in the infarct-related artery (IRA) after the coronary angiography. Aspiration thrombectomy was performed by more than two passages across the lesion. IABP was inserted in all patients with cardiogenic shock or some patients with Killip class 3 that needed intra-aortic balloon bump (IABP) support before PCI.
Myocardial blush grade (MBG) immediately after PCI were evaluated by two experienced investigators, who were otherwise blinded to all clinical data. The perfusion status of IRA was assessed in accordance with the myocardial blush grade [7]. Angiographic no-reflow can be defined as a TIMI flow grade <3 or 3 with an MBG 0–1 [8]. Collateral vessels were graded according to the report by Rentrop [9]. Thrombus score was modified from Gibson [10].
Statistics
All metric variables were described as mean ± standard deviation. Statistical analysis was performed with the Chi-square test for categorical variables. Student’s t test and analysis of variance were used for continuous variables. Univariate and multivariate stepwise logistic regression analysis was performed adjusting diabetes mellitus, age, body mass index (BMI), hypertension, smoking, hyperlipidemia, family history of coronary artery disease (CAD), pre-infarction angina, prior MI, prior PCI, prior coronary artery bypass grafting (CABG), time from pain to PPCI, Killip class, use of cardiovascular medication before AMI, and PCI as reperfusion therapy, physical findings, electrocardiographic findings, admission CrCl, CK-MB, IRA, TIMI flow grade, vessel disease, thrombus score, collateral circulation, reference diameter, lesion diameter, percent stenosis before procedural, target lesion length, stenting methods, post-dilation, stents, stent diameter, post-PCI minimal lumen diameter, maximal inflation pressure, thrombolysis before PCI, intra-aortic balloon bump (IABP) use, tirofiban use, and aspiration thrombectomy.
All statistical processes were performed using SPSS-PC 16.0 (SPSS-PC Inc., Chicago, IL, USA). A p value <0.05 was considered significant.
Results
Patient characteristics
Of the 320 patients who underwent PPCI on an IRA, 81 (25.3%) developed no-reflow after PPCI. Compared to the reflow group, the no-reflow group had significantly lower SBP on admission (101.1 ± 26.7 vs. 114.2 ± 24.4 mmHg, respectively), lower admission DBP (66.0 ± 17.4 vs. 71.5 ± 14.1 mmHg), and significantly higher peak CK values (239 ± 205 vs. 160 ± 166 U/l) (p < 0.05 for all). Moreover, the no-reflow group had a significantly larger proportion of Killip classes 2–4 (54.3 vs. 33.1%, respectively) (p < 0.05 for all). There were no significant differences between the no-reflow group and the reflow group with respect to age, BMI, hypertension, diabetes mellitus, current smoking, hyperlipidemia, prior MI, prior PCI, prior CABG, pre-infarction angina, family history of CAD, medication before infarction, time from pain to balloon, heart rates, electrocardiographic findings, admission CrCl, and admission plasma glucose and LDL-cholesterol (p > 0.05 for all) (Table 1).
Angiographic findings and primary PCI procedure
The angiographic data revealed that the no-reflow group had a significantly larger proportion of low (≤1) initial TIMI flow (84.0 vs. 61.0%, for no-reflow and reflow, respectively), 1 vessel disease (24.7 vs. 13.8%, respectively), collateral flow grades (0–1) (95.1 vs. 82.4%, respectively), pre-PCI thrombus score 2–5 (93.8 vs. 72.8%, respectively), significantly longer target lesion (21.61 ± 9.15 vs. 18.00 ± 7.42 mm, respectively), and significantly more severe stenosis before procedure (99.4 ± 2.2% vs. 97.7 ± 4.6%, respectively) (p < 0.05 for all) (Table 2).
Among the procedural features, the no-reflow incidence was significantly higher in patients who had more post-dilation (54.3 vs. 30.9%, for no-reflow and reflow, respectively), ≥2 stents (37.0 vs. 31.0%), and much IABP use before PCI (24.9 vs. 5.8%, respectively) (p ≤ 0.05 for all) (Table 2).
However, IRA, reference diameter, target lesion diameter, stenting methods, stent diameter, post-PCI minimal lumen diameter, maximal inflation pressure, tirofiban use and aspiration thrombectomy showed no difference between the two groups (p > 0.05 for all) (Table 2).
Independent no-reflow predictors
Univariate and multivariate stepwise logistic regression analysis identified that SBP on admission <100 mmHg (OR 1.991, 95% CI 1.018–3.896; p = 0.004), target lesion length >20 mm (OR 1.948, 95% CI 1.908–1.990; p = 0.016), collateral circulation 0–1 (OR 1.952, 95% CI 1.914–1.992; p = 0.019), pre-PCI thrombus score ≥4 (OR 4.184, 95% CI 1.482–11.813; p = 0.007), and IABP use before PCI (OR 1.949, 95% CI 1.168–3.253; p = 0.011) were independent no-reflow predictors (Table 3).
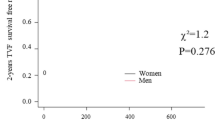
The no-reflow incidence and independent predictors
The no-reflow incidence significantly increased as the numbers of independent predictors increased [0% (0/2), 10.8% (9/84), 14.5% (17/117), 37.7% (29/77), 56.7% (17/30), and 81.8% (9/11) in patients with 0, 1, 2, 3, 4, and 5 independent predictors, respectively; p < 0.0001)] (Fig. 1).
Discussion
Rapid restoration of coronary flow to the jeopardized myocardium has become an essential part of therapy after AMI. Despite an open IRA, breakdown of obstruction to coronary microvasculature can markedly decrease blood flow to the infarct zone. This phenomenon is important because it correlates with infarct size, short- and long-time mortality, and provides useful prognostic information [11].
In the present study, the no-reflow rate after PPCI was 25.3%, which was consistent with previously published no-reflow rates of 5–25% [12]. SBP on admission <100 mmHg, target lesion length >20 mm, collateral circulation 0–1, pre-PCI thrombus score ≥4, and IABP use before PCI were independent no-reflow predictors.
A systolic arterial BP (ABP) <120 mmHg in patients with AMI was associated with a higher mortality than in patients with ABP >120 mmHg [13]. A low SBP (<120 mmHg) decreased coronary blood flow (CBF), collateral blood flow, and increased infarct size [14, 15]. Based on these data, low normal BP is associated with decreased CBF. Furthermore, this decreased CBF accelerates leukocyte accumulation, enhances the trapping of leukocytes in capillaries, and adhesion of leukocytes in venules, and enhances the no-reflow.
Most acute coronary syndromes result from plaque rupture or fissuring with superimposed thrombus formation. Microvascular embolization of plaque material and thrombus content can occur spontaneously or iatrogenically during the PCI procedure [16]. An intravascular ultrasound study showed that high atherothrombotic burden and decreased plaque volume may be risk factors for development of the no-reflow during stent implantation in patients with AMI [17]. Furthermore, a recent study found that fibrofatty volume over the entire lesion length was the only independent factor for no-reflow and slow reflow during PPCI [18]. These studies indicate that not only thrombus burden but also plaque material determines the development of no-reflow. The longer the target lesion, the larger the plaque burden. Our study demonstrates that female patients with a target lesion length >20 mm were about twofold more likely to develop the no-reflow than those with a target lesion length ≤20 mm.
Well-developed collateral circulation theoretically augments microvascular reperfusion by preserving anatomical patency of the vasculature, and enhancing myocardial viability and microvascular integrity within the occluded IRA territory. Collateral flow may prolong the maximal time of coronary occlusion before reperfusion when irreversible transmural myocardial necrosis develops, and reduce infarct size [19]. Well-developed collaterals (≥2) before reperfusion by PCI in patients with STEMI are associated with a protective effect on coronary microcirculation and decreasing no-reflow [20, 21].
Distal embolism of thrombus plays a major role in no-reflow. However, TIMI thrombus grades cannot provide information regarding the no-reflow prediction on subsequent PCI. A previous study showed that specific angiographic morphologic features of high-burden thrombus formation were independent no-reflow predictors in 794 patients with AMI after PPCI [22], but these predictors are very complex to guide subsequent PCI and adjunctive therapies. Our study is in accordance with a previous study [23], showing that pre-PCI thrombus score ≥4 was one of no-reflow predictors.
Our study demonstrates that all patients with cardiogenic shock, and some patients with Killip class 3 on admission that needed IABP support, and not all patients with Killip class 3 on admission, had a higher no-reflow incidence. A linear association between Killip class and postprocedural TIMI 3 flow was also observed in the Shock Trial Registry [24]. Killip class ≥3 at presentation may be a consequence of a larger infarction that may be associated with more severe damage of microvascular bed and decreasing coronary perfusion pressure, thus explain that the patients with IABP use had higher no-reflow incidence in our study. The cardiac cells within the no-reflow area were swollen by microscopic examination. The capillary endothelium was damaged and exhibited areas of regional swelling with large intraluminal protrusions that in some cases appeared to plug the capillary lumen [25]. Cellular edema and cell contracture compressing the capillaries may contribute to the microvascular compression [26]. A higher rate of distal embolization was found in patients with advanced Killip class, which may partially explain the no-reflow observed in these patients [27].
Limitations
The no-reflow prediction model should be confirmed in large-scale prospective studies in the future. The major limitation is the absence of a core-lab, although angiographic data were analyzed with similar criteria. The no-reflow was diagnosed without the assistance of myocardial contrast echocardiography. Hence, the evaluation of coronary microcirculation was insufficient.
Conclusions
The five no-reflow predicting variables were SBP on admission <100 mmHg, target lesion length >20 mm, collateral circulation 0–1, pre-PCI thrombus score ≥4, and IABP use before PCI in patients with STEMI treated with PPCI. Therefore, the prediction model provides a basis for therapeutic decision-making. Because most patients with STEMI have a combination of these factors, combined treatment strategies are preferred to improve patient outcomes, such as aspiration thrombectomy, adenosine, or glycoprotein IIb/IIIa inhibitors [28].
References
Pepine CJ (2004) Ischemic heart disease in women: facts and wishful thinking. J Am Coll Cardiol 43:1727–1730
Lee KH, Jeong MH, Ahn YK, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi D, Cho MC, Kim CJ, Seung KB, Chung WS, Jang YS, Cho JG, Park SJ, Korea Acute Myocardial Infarction Registry (KAMIR) Investigators (2008) Gender differences of success rate of percutaneous coronary intervention and short-term cardiac events in Korea Acute Myocardial Infarction Registry. Int J Cardiol 130:227–234
Vaknin-Assa H, Assali A, Fuchs S, Zafrir N, Kornowski R (2006) Prognostic impact of sex on clinical outcomes following emergent coronary angioplasty in acute myocardial infarction. Coron Artery Dis 17:1–5
De Luca G, Suryapranata H, Dambrink JH, Ottervanger JP, Van’t Hof AW, Zijlstra F, Hoorntje JC, Gosselink AT, de Boer MJ (2004) Sex-related differences in outcome after ST-segment elevation myocardial infarction treated by primary angioplasty: data from the Zwolle Myocardial Infarction study. Am Heart J 148:852–856
Lansky AJ, Pietras C, Costa RA, Tsuchiya Y, Brodie BR, Cox DA, Aymong ED, Stuckey TD, Garcia E, Tcheng JE, Mehran R, Negoita M, Fahy M, Cristea E, Turco M, Leon MB, Grines CL, Stone GW (2005) Gender differences in outcomes after primary angioplasty versus primary stenting with and without abciximab for acute myocardial infarction: results of the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) Trial. Circulation 111:1611–1618
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16:31–41
Van’t Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F (1998) Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Circulation 97:2302–2306
Niccoli G, Burzotta F, Galiuto L, Crea F (2009) Myocardial no-reflow in humans. J Am Coll Cardiol 54:281–292
Rentrop KP, Cohen M, Blanke H, Phillips RA (1985) Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol 5:587–592
Gibson CM, de Lemos JA, Murphy SA, Marble SJ, McCabe CH, Cannon CP, Antman EM, Braunwald E, TIMI Study Group (2001) Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction: a TIMI 14 substudy. Circulation 103:2550–2554
Brosh D, Assali AR, Mager A, Porter A, Hasdai D, Teplitsky I, Rechavia E, Fuchs S, Battler A, Kornowski R (2007) Effect of no-reflow during primary percutaneous coronary intervention for acute myocardial infarction on six-month mortality. Am J Cardiol 99:442–445
Reffelmann T, Kloner RA (2002) The no-reflow phenomenon: basic science and clinical correlates. Heart 87:162–168
Lee KL, Woodlief LH, Topol EJ, Weaver WD, Betriu A, Col J, Simoons M, Aylward P, Van de Werf F, Califf RM, for the GUSTO-I Investigators (1995) Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction: results from an international trial of 41021 patients. Circulation 91:1659–1668
Nanas JN, Tsolakis E, Terrovitis JV, Eleftheriou A, Drakos SG, Dalianis A, Charitos CE (2004) Moderate systemic hypotension during reperfusion reduces the coronary blood flow and increases the size of myocardial infarction in pigs. Chest 125:1492–1499
Ishikura F, Miki A, Iwata A, Toshida T, Shakudo M, Asanuma T, Kitakaze M, Shinozaki Y, Mori H, Beppu S (2008) Effect of systemic blood pressure on microcollateral circulation evaluated by real-time contrast echocardiography. J Am Soc Echocardiogr 21:765–769
Skyschally A, Erbel R, Heusch G (2003) Coronary microembolization. Circ J 67:279–286
Katayama T, Kubo N, Takagi Y, Funayama H, Ikeda N, Ishida T, Hirahara T, Sugawara Y, Yasu T, Kawakami M, Saito M (2006) Relation of atherothrombosis burden and volume detected by intravascular ultrasound to angiographic no-reflow phenomenon during stent implantation in patients with acute myocardial infarction. Am J Cardiol 97:301–304
Bae JH, Kwon TG, Hyun DW, Rihal CS, Lerman A (2008) Predictors of slow flow during primary percutaneous coronary intervention: an intravascular ultrasound virtual histology study. Heart 94:1559–1564
Reimer KA, Jennings RB, Cobb FR, Murdock RH, Greenfield JC Jr, Becker LC, Bulkley BH, Hutchins GM, Schwartz RP Jr, Bailey KR (1985) Animal models for protecting ischemic myocardium: results of the NHLBI Cooperative Study. Comparison of unconscious and conscious dog models. Circ Res 56:651–655
Desch S, Eitel I, Schmitt J, Sareban M, Fuernau G, Schuler G, Thiele H (2009) Effect of coronary collaterals on microvascular obstruction as assessed by magnetic resonance imaging in patients with acute ST-elevation myocardial infarction treated by primary coronary intervention. Am J Cardiol 104:1204–1209
Jorapur V, Steigen TK, Buller CE, Dzavík V, Webb JG, Strauss BH, Yeoh EE, Kurray P, Sokalski L, Machado MC, Kronsberg SS, Lamas GA, Hochman JS, Mancini GB (2008) Distribution and determinants of myocardial perfusion grade following late mechanical recanalization of occluded infarct-related arteries postmyocardial infarction: a report from the Occluded Artery Trial. Catheter Cardiovasc Interv 72:783–793
Yip HK, Chen MC, Chang HW, Hang CL, Hsieh YK, Fang CY, Wu CJ (2002) Angiographic morphologic features of infarct-related arteries and timely reperfusion in acute myocardial infarction. Chest 122:1322–1332
Kirma C, Izgi A, Dundar C, Tanalp AC, Oduncu V, Aung SM, Sonmez K, Mutlu B, Ozdemir N, Erentug V (2008) Clinical and procedural predictors of no-reflow phenomenon after primary percutaneous coronary interventions. Circ J 72:716–721
Hochman JS, Buller CE, Sleeper LA, Boland J, Dzavik V, Sanborn TA, Godfrey E, White HD, Lim J, LeJemtel T (2001) Cardiogenic shock complicating acute myocardial infarction-etiologies, management and outcome: a report from the SHOCK Trial Registry. Should we emergently revascularize occluded coronaries for cardiogenic shock? JAMA 285:190–192
Summers WK, Jamison RL (1971) The no reflow phenomenon in renal ischemia. Lab Invest 25:635–643
Lee BY, Wilson GJ, Domenech RJ, MacGregor DC (1980) Relative roles of edema versus contracture in the myocardial postischemic “no-reflow” phenomenon. J Surg Res 29:50–61
De Luca G, Gibson CM, Huber K, Zeymer U, Dudek D, Cutlip D, Bellandi F, Noc M, Emre A, Zorman S, Gabriel HM, Maioli M, Rakowski T, Gyöngyösi M, Van’t Hof AW; EGYPT Cooperation (2009) Association between advanced Killip class at presentation and impaired myocardial perfusion among patients with ST-segment elevation myocardial infarction treated with primary angioplasty and adjunctive glycoprotein IIb-IIIa inhibitors. Am Heart J 158:416–421
Tarsia G, De Michele M, Polosa D, Biondi-Zoccai G, Costantino F, Del Prete G, Osanna RA, Innelli P, Sisto F, Sheiban I, Lisanti P (2010) Manual versus nonmanual thrombectomy in primary and rescue percutaneous coronary angioplasty. Heart Vessels 25:275–281
Conflict of interest
The authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, Y., Wang, C., Yang, X. et al. Independent no-reflow predictors in female patients with ST-elevation acute myocardial infarction treated with primary percutaneous coronary intervention. Heart Vessels 27, 243–249 (2012). https://doi.org/10.1007/s00380-011-0144-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-011-0144-2