Abstract
Purpose
To describe trends in the pharmacological treatment of BPH in the United Kingdom (UK) from 1998 to 2016.
Methods
We created a cohort of men with a diagnosis of BPH between 1998 and 2016 using the Clinical Practice Research Datalink. Using Poisson regression, we estimated annual prescription rates of 5αRIs, α-blockers, and combination therapy (5αRIs + α-blockers). Adherence was defined by a proportion of days covered > 80%.
Results
Our cohort included 192,640 men with BPH who generated 1,176,264 person-years (PYs) of follow-up. The mean age was 68.0 (standard deviation: 10.7) years. The prescription rate of all BPH medications during the study period was 347.6 per 100 PYs (95% CI 347.2–347.9). α-Blockers had the highest prescription rate (222.9 per 100 PYs, 95% CI 222.7–223.2); prescription rates of 5αRIs and combination therapy were 69.1 per 100 PYs (95% CI 69.0–69.3) and 55.5 per 100 PYs (95% CI 55.4–55.7), respectively. The prescription rate for combination therapy was 19 times greater in 2013–2016 than in 1998–2000 (rate ratio: 19.2, 95% CI 18.6–19.7), while the prescription rates for 5αRIs and α-blockers each doubled during this period (rate ratio: 1.86, 95% CI 1.84–1.88 and rate ratio: 2.02, 95% CI 2.01–2.04, respectively). The proportion of patients who were adherent at 1 year to 5αRIs (32.3%), α-blockers (44.0%), and combination therapy (45.6%) was low.
Conclusion
The prescription rate of BPH medications increased substantially between 1998 and 2016 in the UK, with the greatest relative increase observed with combination therapy. Adherence to BPH medications was low in this population-based study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Benign prostatic hyperplasia (BPH), also known as benign prostatic hypertrophy, is a condition affecting middle-aged and older men and is characterized by an enlarged prostate that restricts the normal flow of urine through the urethra [1]. It affects an estimated 15 million American men aged 30–79 years [2]. More than 50% of men aged 60–69 years have symptoms of BPH, with the prevalence increasing up to 90% in older age groups [1]. The prostate volume may increase over time in men with BPH with a subsequent worsening of lower urinary tract symptoms (LUTS), increased degree of bother, and acute urinary retention [3].
In the past 20 years, multiple treatment modalities for BPH have arisen, including watchful waiting, lifestyle changes, drug therapy, and surgical intervention [4]. Initial treatment typically consists of a strategy of watchful waiting and lifestyle modification [5]. For patients with symptomatic bother, BPH treatment progresses to medical therapy, including five-alpha reductase inhibitors (5αRIs) and α-adrenergic antagonists (commonly referred to as ‘α-blockers’), and/or surgery [6]. α-Blockers relax the smooth muscle tone of the prostate and bladder neck, increasing urinary flow [7]. By reducing the prostate size by 20–30% within 3–6 months of use, [8] 5αRIs have been associated with a 50% reduction in total serum prostate-specific antigen level, [9] a 57% relative risk reduction for acute urinary retention, and a 48% relative risk reduction for surgery compared with placebo [10]. They have also been shown to improve quality of life [11].
With an aging population, an increasing prevalence of BPH, and the emergence of new pharmacological treatments for BPH (including combination therapy), there is a need to better understand the population-based treatment patterns for BPH. While a small number of previous studies had examined the patterns of BPH drugs, [12, 13] these studies did not provide a thorough assessment of the trends of the pharmacological treatment of BPH, describing the use of α-blockers only [13] or examining use over a short duration of follow-up only [12]. The objective of this study was therefore to describe the trends in the pharmacological treatment of BPH between 1998 and 2016 in the United Kingdom (UK).
Methods
Data source
We conducted a retrospective cohort study using data from the UK’s Clinical Practice Research Datalink (CPRD). CPRD data are documented by the trained general practitioners and contain the complete primary care medical records of more than 11 million patients from more than 700 general practices across the UK [14]. The CPRD includes over 40 years of longitudinal data and covers approximately 11% of the UK population, of which it is broadly considered to be representative with respect to age, sex, and ethnicity [14]. Participating practices record lifestyle information (BMI and smoking) and each episode of clinical events (symptoms, diagnoses), preventive care, tests, immunizations, specialist referrals, hospital admissions and their major outcomes, and details related to death [14]. Clinical diagnoses are recorded using Read codes, a hierarchical clinical classification system containing over 96,000 codes [14]. The system also captures all prescriptions generated by the general practitioner using a drug product name and British National Formulary code, alongside the details regarding dosage and quantity [14]. Several validation studies have assessed the accuracy, completeness, and consistency of CPRD data and determined that these data are of high quality [14, 15].
This study underwent scientific and ethical review by the Independent Scientific Advisory Committee (ISAC) of the Medicines and Healthcare products Regulatory Agency (ISAC number 16_265A2, the protocol for which was made available to journal reviewers) and ethical review by the research ethics board of the Jewish General Hospital in Montreal, Canada.
Study population
We identified all patients with a Read code indicating the presence of BPH in the CPRD (Supplementary Table 1). This cohort consisted of all patients with BPH, and we refer to this cohort as the ‘prevalent’ cohort. This cohort served as the study population for our primary analysis. The date of cohort entry for this cohort was defined by the latest of: the date of BPH diagnosis, the date on which the patient turned 40 years of age, the date by which the patient had 1 year of observation time in the CPRD, or January 1, 1998 (the beginning of our study period). We also created a secondary cohort restricted to patients newly diagnosed with BPH during the study period. In this cohort, we excluded patients whose first BPH diagnosis occurred before January 1, 1998 or with less than 1 year of CPRD observation time. We refer to this cohort as the ‘incident’ cohort. The date of this first BPH diagnosis defined cohort entry in the incident cohort. From this cohort, we further excluded patients who received a prescription for a BPH drug in the year before this first diagnosis, those with a missing date for their first recorded BPH diagnosis, and men with a history of prostatism. From both cohorts, we excluded patients with a diagnosis of prostate cancer prior to cohort entry as 5αRIs and α-blockers can be used off-label for the treatment of prostate cancer or relieve symptoms associated with cancer treatment. In all analyses, patients were followed from cohort entry until a diagnosis of prostate cancer, departure from the CPRD, the end of the study period (March 31, 2016), or death, whichever occurred first.
BPH medications
The vast majority of medications used to manage the symptoms of BPH are α-blockers and 5αRIs [16]. α-Blockers monotherapy are often considered the first-line pharmacotherapy for BPH [16]. The European Medical Agency (EMA) and the US Food and Drug Administration (FDA) have approved both selective (alfuzosin, silodosin, and tamsulosin) and non-selective (doxazosin, prazosin, and terazosin) α-blockers for the treatment of BPH. Non-selective α-blockers also inhibit α-adrenergic receptors found in the vascular smooth muscle and are also indicated for hypertension [5, 6, 17]. The two main 5αRIs inhibitors approved in the UK for BPH treatment are dutasteride and finasteride [16]. Combination drugs are also available that include combinations of finasteride (5αRI) and terazosin (α-blocker) or dutasteride (5αRI) and tamsulosin (α-blocker). We defined combination therapy based on 1) the prescription of the two classes of drugs in a combined formulation as a single pill; or 2) the prescription of each class of treatment (5αRIs and α-blocker) on the same date.
Statistical analyses
We first described patients’ demographic and clinical characteristics at the time of cohort entry. These baseline characteristics included age in years, frequency of general practitioner visits in the prior year, prostate-specific antigen (PSA) level, lifestyle characteristics (body mass index [BMI], smoking), and Charlson Comorbidity Index (CCI). The rate of prescription was defined by the number of a prescription issued per 100 person-years of follow-up. Using Poisson regression, we estimated prescription rates and corresponding 95% confidence intervals (CIs) for 5αRIs, α-blockers, and combination therapies between January 1, 1998 and March 31, 2016, overall and by time period. We estimated crude and age-adjusted rate ratios (RRs) and 95% CIs comparing each subsequent period to 1998–2000, with age modeled non-linearly using a restricted cubic spline with five knots. We performed all statistical analyses using SAS version 9.4 (SAS Institute Inc., Cary. NC, USA).
We conducted four secondary analyses. First, we stratified our analyses by age. Second, we sub-classified prescriptions of 5αRIs and α-blockers by molecule. Third, we repeated our analyses among patients with incident BPH. Finally, we estimated adherence to BPH therapies (5αRIs, α-blockers, and combination therapy) at 1 and 2 years, with adherence defined by a proportion of days covered (PDC) of at least 80%. We assumed that prescriptions were for 30 days, and we included a 30-day grace period in our main adherence analysis. The PDC formula is described in detail in the Supplementary Methods. In addition, we assessed the association between adherence and baseline patients’ characteristics using multivariable logistic regression.
We conducted four sensitivity analyses to assess the robustness of our results. First, we assumed that prescriptions for a new class of drugs represented add-on therapy rather than a treatment switch. Second, we changed the reference category for our estimated RRs to the preceding period rather than using the 1998–2000 period. Third, we also estimated the rates and rate ratios for combination therapy sub-classified as either combination pills or two separate prescriptions issued on the same day. Finally, we repeated our adherence analyses without the inclusion of a grace period.
Results
Study population and patient characteristics
Among 231,174 patients with a diagnosis of BPH initially identified in CPRD, 192,640 patients met our inclusion criteria and were included in our primary cohort (Fig. 1). Table 1 presents the baseline characteristics of our BPH cohort. Overall, the mean age of BPH patients in the cohort was 68.0 ± 10.7 years. Patients prescribed 5αRIs (72.8 ± 10.0 years) and combination therapy (72.1 ± 9.7 years) were older than patients with no prescription for BPH medication (67.2 ± 10.8 years) and those prescribed α-blockers (68.6 ± 10.2 years). Approximately, half of the patients had a BMI < 30 kg/m2 (52.3%), and slightly less than half were recorded as ever smokers (48.4%). Patients with no BPH medication prescription and those prescribed α-blockers had fewer general practitioner visits and lower CCI scores than those prescribed 5αRIs or combination therapy.
Trends of BPH medications’ prescriptions
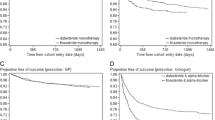
Table 2 presents prescription rates and rate ratios for 5αRIs, α-blockers, and combination therapy overall and by calendar time. The median duration of follow-up was 1850 days (interquartile range 760–3422 days). Less than a third of patients (27.3%) remained in the cohort until the end of the study period, while 21.8% of patients died during follow-up. The overall prescription rate of BPH medications over the study period was 347.6 per 100 PYs (95% CI 347.2–347.9). α-Blockers had the highest prescription rate (222.9 per 100 PYs, 95% CI 222.7–223.2), whereas 5αRIs and combination therapy had relatively lower prescription rates (69.1 per 100 PYs, 95% CI: 69.0–69.3 and 55.5 per 100 PYs, 95% CI: 55.4–55.7, respectively). The prescription of 5αRIs, α-blockers, and combination therapy steadily increased from 1998 to 2016 (Fig. 2, Table 2). The greatest relative increase occurred with combination therapy, with a prescription rate that was 19 times greater in 2013–2016 than in 1998–2000 (age-adjusted RR: 19.2, 95% CI 18.6–19.7). In contrast, the prescription rates for 5αRIs and α-blockers each doubled during this period (age-adjusted RR: 1.86, 95% CI 1.84–1.88 and 2.02, 95% CI 2.01–2.04, respectively). Similar estimates were obtained when modeling age as a continuous variable, as a categorical variable, and non-linearly using a restricted cubic spline (Supplementary Table 2).
Secondary analyses
The rate of prescriptions not only increased over time, but also with age (Fig. 3). In particular, 5αRIs and combination therapy were prescribed 11 (RR: 11.4, 95% CI 11.2–11.6) and 9 (RR: 8.8, 95% CI 8.7–9.0) times more frequently in patients older than 85 years than in patients aged 40–54 years, respectively (Table 3, Supplementary Table 3, and Supplementary Fig. 1). In molecule-specific analyses of 5αRIs drugs, similar trends were observed for both dutasteride and finasteride (Supplementary Table 4). In molecule-specific analyses of α-blockers, tamsulosin was most frequently prescribed and had the largest increase over time (Supplementary Table 5). The proportion of patients who were adherent at 1 year to 5αRIs (32.3%), α-blockers (44.0%), and combination therapy (45.6%) was low (Table 4). Baseline variables associated with adherence to 5αRIs were age, BMI, and CCI score (Supplementary Table 6). Age, calendar year, BMI, smoking status, PSA testing, and CCI were associated with adherence to α-blockers. Age, calendar year, and PSA testing were associated with adherence to combination therapy. Finally, our analyses restricted to patients with incident BPH revealed similar trends as observed in the primary cohort (Supplementary Tables 7, 8 and 9 and Supplementary Figs. 2, 3 , 4 and 5).
Sensitivity analyses
Considering the prescription of a new class of drugs as add-on therapy rather than a treatment switch produced results that were consistent with those of our primary analysis. Changing the reference category to the preceding period attenuated the estimated RRs; all RRs remained greater than one except for the prescription of 5αRIs during the 2013–2016 period, which showed a slight decrease compared to 2010–2012 (Supplementary Table 10). Finally, the sub-classification of combination therapy by formulation revealed that the observed increase in combination therapy occurred in individuals prescribed separate molecules on the same day, as combination pills only entered the market in 2010 and only accounted for a minority of combination therapy prescriptions by the end of the study period (Supplementary Table 11).
Discussion
The prescription rate of BPH medications in the UK considerably increased between 1998 and 2016. This increase was largely driven by the increased prescription of α-blockers, which accounted for 64% of all BPH medication prescriptions during the study period. The overall share of 5αRI prescriptions was less than 20% and steadily increased from 1998 before stabilizing in 2010. Although the absolute rate of prescription was less than that of the monotherapies, the greatest relative increase was observed in the prescription rate combination therapy.
Trends in the prescription of α-blockers showed an increasing pattern largely driven by the prescription of tamsulosin between 1998 and 2016. This trend is consistent with the trends reported by previous studies [12, 13, 18]. After the FDA approval of the α-blocker tamsulosin in 1997, the prescription of α-blockers increased by twofold [19]. Several clinical guidelines such as those issued by the National Institute for Health and Care Excellence, [16] the European Association of Urology, [6] the American Urological Association, [20] and the Canadian Urological Association [21] recommend α-blockers as first-line therapy for men with moderate to severe LUTS and 5αRIs to men with LUTS who have prostates estimated to be larger than 30 g. These recommendations emanate from the high clinical efficacy of α-blockers, their low adverse side effect profile, quick onset of action, and low costs [4].
The prescription rate of 5αRIs also increased, doubling between 1998 and 2016. Despite this observed increase, the prescription rate for this class remains much lower than that of α-blockers. This lower prescription rate is consistent with the recommended use of 5αRIs as second-line therapy [16]. It may also be due to their perceived safety profile; 5αRIs are associated with more serious adverse events than α-blockers, including erectile dysfunction and decreased libido [22]. The FDA has also issued a drug safety warning about increased prostate cancer risk with 5αRIs in 2011, which may have affected physicians’ and patients’ treatment choices [2]. In addition, the uptake of dutasteride was slow in the UK, and general practitioners in the UK did not start prescribing it until 2003 [19].
The prescription rate for combination therapy substantially increased between 1998 and 2016. This trend might be due to the demonstration of the potential complementary mechanisms of these two classes of drugs [23]. In the 1990s, α-blockers were preferred over the combination therapy as a result of the Veterans Affairs Cooperative study [24] and the Prospective European Doxazosin and Combination Therapy Trial study, [25] which reported no difference in short-term effects between α-blocker monotherapy and combination therapy. In contrast, subsequent large randomized studies reported that long-term combination therapy could suppress the progression of BPH and reduce surgical interventions for BPH more effectively than either α-blocker or 5αRIs monotherapies [26]. The rate of combination therapy increased fivefold after the publication of MTOPS study [19].
We found that adherence to BPH medications was low, with only 32.3, 39.2, and 45.6% of patients adherent at 1 year to 5αRIs, α-blockers, and combination therapy, respectively. Adherence among BPH patients has been assessed previously; we reported higher adherence to BPH medication than previous studies [27, 28]. The difference in the study design and our use of PDC to define adherence represent the most likely reasons for this discrepancy. Most of the previous studies in this area defined adherence by discontinuation of therapy [27, 29] or using a medication adherence questionnaire [28]. However, a study by Nichol et.al, which used PDC as a measure of adherence, reported a comparable proportion of adherence (62% in combination therapy and 55% in α-blockers) as that reported here [29]. We also observed higher adherence with combination therapy than monotherapies. Patients with an advanced stage of BPH are more likely to be prescribed combination therapy, and the available literature suggests that patients with more severe disease and worse outcomes are less likely to complain about the side effects [30]. Ultimately, although the low levels of adherence may be attributable to potential side effects in routine clinical setting, [26, 29] future studies are needed to better understand the reasons behind these low levels of adherence.
This study has several strengths. First, the use of CPRD data allowed for a thorough analysis of population-based longitudinal trends of BPH medications prescriptions in the UK. These data are also well validated and have been the sources of over 2000 peer-reviewed publications [14]. Second, the CPRD records prescriptions written by the general practitioner rather than pharmacy dispensing. Consequently, it provides a more valid measurement of treatment intentions. Third, we carried out several sensitivity analyses to assess the robustness of our results and repeated all analyses in the incident cohort.
This study also has potential limitations. First, the CPRD does not record prescriptions written by specialists; therefore, some misclassification is possible. However, BPH is a chronic condition that is typically managed in the primary care setting in the UK, where the general practitioner serves as the gatekeeper to the health-care system. Consequently, while the CPRD may not record some early prescriptions, most prescriptions for BPH medications will be issued by general practitioners and recorded in the CPRD. Second, we assumed that all prescriptions were for 30 days, as the most common prescription duration in the CPRD for medications used to treat chronic conditions is 28–30 days. Third, we defined combination therapy as either a prescription of a combination pill or prescription of both classes of medication on the same day, assuming that those who received prescriptions on different days switched treatments; sensitivity analyses that considered such prescriptions add-on therapy rather than switches produced results that were consistent with those of our primary analysis. Finally, we did not estimate the trends of other class of BPH medications prescriptions such as anti-muscarinic and phosphodiesterase inhibitors, as they were not commonly prescribed during the study period.
Conclusions
The overall rate of prescription of BPH medications substantially increased from 1998 to 2016 in the UK. This increase was largely driven by the increased prescription of α-blockers. The relative use of combination therapy also increased substantially over time, suggesting a trend toward a more aggressive approach to the pharmacological management of BPH. Low rates of adherence were observed for all classes of medication used to treat BPH.
References
Bushman W (2009) Etiology, epidemiology, and natural history of benign prostatic hyperplasia. Urol Clin North Am 36:403–415
FDA Drug Safety Communication: 5-alpha reductase inhibitors (5-ARIs) may increase the risk of a more serious form of prostate cancer. 2011. (Accessed July 13, 2017, at https://www.fda.gov/drugs/drugsafety/ucm258314.htm.)
Santos DJ (2012) Benign prostatic hyperplasia: clinical manifestations and evaluation. TechVascIntervRadiol 15:265–269
Yuan JQ, Mao C, Wong SY et al (2015) Comparative effectiveness and safety of monodrug therapies for lower urinary tract symptoms associated with benign prostatic hyperplasia: a network meta-analysis. Medicine (Baltimore) 94:e974
McVary KT, Roehrborn CG, Avins AL et al (2011) Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol 185:1793–1803
Oelke M, Bachmann A, Descazeaud A et al (2013) EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 64:118–140
Roehrborn CG (2011) Male lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). MedClinNorth Am 95:87–100
McConnell JD, Bruskewitz R, Walsh P et al (1998) The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. N Engl J Med 338:557–563
Roehrborn CG (2011) Male lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). Med Clin N Am 95:87–100
Roehrborn CG, Boyle P, Nickel JC, Hoefner K, Andriole G (2002) Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology 60:434–441
MacDonald D, McNicholas TA (2003) Drug treatments for lower urinary tract symptoms secondary to bladder outflow obstruction. Drugs 63:1947–1962
Hakimi Z, Johnson M, Nazir J, Blak B, Odeyemi IA (2015) Drug treatment patterns for the management of men with lower urinary tract symptoms associated with benign prostatic hyperplasia who have both storage and voiding symptoms: a study using the health improvement network UK primary care data. Curr Med Res Opin 31:43–50
Moon HW, Yang JH, Choi JB et al (2018) Prescription pattern of alpha-blockers for management of lower urinary tract symptoms/benign prostatic hyperplasia. Sci Rep 8:13223
Herrett E, Gallagher AM, Bhaskaran K et al (2015) Data resource profile: clinical practice research datalink (CPRD). Int J Epidemiol 44:827–836
Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ (2010) Validation and validity of diagnoses in the general practice research database: a systematic review. BrJClinPharmacol 69:4–14
National Institute for Health and Care Excellence (2010) Lower urinary tract symptoms in men: assessment and management. Clinical guideline 97. https://www.nice.org.uk/guidance/cg97. Accessed 8 Sept 2020
Gratzke C, Bachmann A, Descazeaud A et al (2015) EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 67:1099–1109
Hutchison A, Farmer R, Verhamme K, Berges R, Navarrete RV (2007) The efficacy of drugs for the treatment of LUTS/BPH, a study in 6 European countries. Eur Urol 51:207–215 (discussion 15-6)
Filson CP, Wei JT, Hollingsworth JM (2013) Trends in medical management of men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Urology 82:1386–1392
Parsons JK, Dahm P, Köhler TS, Lerner LB, Wilt TJ Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment 2020. Available online: https://www.auajournals.org/doi/full/10.1097/JU.0000000000001298. Accessed 8 Sept 2020
Nickel JC, Aaron L, Barkin J, Elterman D, Nachabé M, Zorn KC (2018) Canadian Urological Association guideline on male lower urinary tract symptoms/benign prostatic hyperplasia (MLUTS/BPH): 2018 update. Can Urol Assoc J 12:303–312
Hirshburg JM, Kelsey PA, Therrien CA, Gavino AC, Reichenberg JS (2016) Adverse effects and safety of 5-alpha reductase inhibitors (Finasteride, Dutasteride): a systematic review. J Clin Aesthet Dermatol 9:56–62
Fullhase C, Chapple C, Cornu JN et al (2013) Systematic review of combination drug therapy for non-neurogenic male lower urinary tract symptoms. Eur Urol 64:228–243
Lepor H, Williford WO, Barry MJ et al (1996) The efficacy of terazosin, finasteride, or both in benign prostatic hyperplasia Veterans Affairs Cooperative Studies Benign Prostatic Hyperplasia Study Group. N Engl J Med 335:533–539
Kirby RS, Roehrborn C, Boyle P et al (2003) Efficacy and tolerability of doxazosin and finasteride, alone or in combination, in treatment of symptomatic benign prostatic hyperplasia: the Prospective European Doxazosin and Combination Therapy (PREDICT) trial. Urology 61:119–126
McConnell JD, Roehrborn CG, Bautista OM et al (2003) The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med 349:2387–2398
Lukacs B, Cornu JN, Aout M et al (2013) Management of lower urinary tract symptoms related to benign prostatic hyperplasia in real-life practice in france: a comprehensive population study. Eur Urol 64:493–501
Zabkowski T, Saracyn M (2018) Drug adherence and drug-related problems in pharmacotherapy for lower urinary tract symptoms related to benign prostatic hyperplasia. J Physiol Pharmacol. https://doi.org/10.26402/jpp.2018.4.14
Nichol MB, Knight TK, Wu J, Barron R, Penson DF (2009) Evaluating use patterns of and adherence to medications for benign prostatic hyperplasia. J Urol 181:2214–2221 (discussion 21-2)
DeCastro J, Stone B (2008) Improving therapeutic outcomes in BPH through diagnosis, treatment and patient compliance. Am J Med 121:S27–33
Acknowledgements
This study was funded by a CIHR operating grant (MOP-136946). Dr. Ayele is supported by a postdoctoral award from the Fonds de recherche du Québec–anté (FRQS). Drs. Azoulay and Filion are supported by salary support awards from the FRQS and William Dawson Scholar awards from McGill University. Dr. Platt is a member of the Research Institute of the McGill University Health Center, which receives financial support from the FRQS, and holds the Albert Boehringer I endowed chair in Pharmacoepidemiology at McGill University. The sponsors had no role in designing, data analysis, manuscript preparation, and dissemination or publication of the study.
Funding
This study was funded by a CIHR operating grant (MOP-136946). Dr. Ayele is supported by a postdoctoral award from the Fonds de recherche du Québec–Santé (FRQS). Drs. Azoulay and Filion are supported by salary support awards from the FRQS and William Dawson Scholar awards from McGill University. Dr. Platt is a member of the Research Institute of the McGill University Health Center, which receives financial support from the FRQS, and holds the Albert Boehringer I endowed chair in Pharmacoepidemiology at McGill University. The sponsors had no role in designing, data analysis, manuscript preparation, and dissemination or publication of the study.
Author information
Authors and Affiliations
Contributions
HTA: contributed to the study design, defined the study variables’ code, interpreted the results and drafted the manuscript. PR: conducted the data management and analyses and critically reviewed the manuscript for important intellectual content. LA: critically reviewed the manuscript for important intellectual content. RWP: critically reviewed the manuscript for important intellectual content. JC: conducted the data management and analyses and critically reviewed the manuscript for important intellectual content. SB: critically reviewed the BPH codes definition and the manuscript for important intellectual content. KBF: developed the protocol, supervised the project, contributed to the interpretation of results, and critically reviewed the study variables’ code and the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest. The authors have nothing to disclose in particular relation to this study.
Research involving human participants and/or animals
This study included men over the age of 40 years with the incident diagnosis of BPH. However, informed consent was not required (see below).
Informed consent
Studies using the CPRD are not required to obtain informed consent from the individual study participants as data are anonymized. CPRD operates an opt-in model whereby a GP practice must provide consent for CPRD to collect de-identified primary care data from their practice. Patients at participating practices have the right to opt out of sharing and use of their data for research at any time and CPRD respects and abides by this choice.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ayele, H.T., Reynier, P., Azoulay, L. et al. Trends in the pharmacological treatment of benign prostatic hyperplasia in the UK from 1998 to 2016: a population-based cohort study. World J Urol 39, 2019–2028 (2021). https://doi.org/10.1007/s00345-020-03429-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03429-z