Abstract
Introduction
The BPH surgical armamentarium is composed of a rapidly expanding number of technologies and techniques. These include greenlight photovaporization of the prostate (PVP), greenlight enucleation of the prostate (GreenLEP), holmium laser enucleation of the prostate (HoLEP), thulium laser enucleation of the prostate (ThuLEP) and, more recently, the aquablation procedure. To the best of our knowledge, no direct comparison in operative time has been performed.
Methods
Data for this study were pooled from five sources. For aquablation, patient-level data from four studies of the aquablation procedure were provided by the device manufacturer as well as from a high-volume commercial user. PVP, GreenLEP, HoLEP, and ThuLEP were performed by high-volume, experienced experts. Endpoints included total operative time, resection time, and proportion of total operative time for resection. General linear models were used to evaluate the relationship between prostate volume (or other continuous predictors) and procedure time.
Results
Total procedure time was related to prostate size. Except for the small prostate size range (size < 40 cc), at any given prostate volume, procedure time was highest for PVP, intermediate for LEPs, and lowest for Aquablation. The relationship between procedure time and prostate size (i.e., slope of the fitted lines) was 0.16 min/g for aquablation, 0.32 min/g, 0.28 min/g and 0.32 min/g for GreenLEP, HoLEP and ThuLEP, respectively, and 0.63 min/g for PVP.
Conclusion
In our analysis of pooled data of multi-surgical techniques and technologies, aquablation provided the lowest operative time across all prostate volumes. PVP had the longest procedure time for prostates > 40 cc.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Benign prostatic hyperplasia (BPH) is a histologic diagnosis of smooth muscle and epithelial cell proliferation within the prostatic transition zone [1]. It is the most common benign urologic disease in men. Its incidence is age-related—as the population ages, its prevalence will continue to increase, particularly increasing in incidence after age 50 [2].
Surgery is indicated for lower urinary tract symptoms (LUTS) attributed to BPH and unresponsive to conservative (primarily medication) treatment, provided the patient’s comorbidities do not preclude this approach [3]. In accordance with current national guidelines, the BPH surgical ablative armamentarium is composed of a number of technologies and techniques [3,4,5] However, only a few can be considered for treating small to very large prostates with TURP-like efficacy. These include greenlight photovaporization of the prostate (PVP), greenlight enucleation of the prostate (GreenLEP), holmium laser enucleation of the prostate (HoLEP), thulium laser enucleation of the prostate (ThuLEP) and, more recently, aquablation.
HoLEP harnesses the well-established, globally available 2140 nm pulsed holmium:yttrium–aluminum–garnet (Ho:YAG) laser to assist with mechanical enucleation of the prostate. This wavelength is strongly absorbed by water (and water-rich tissues) with good hemostasis [6]. Enucleation, having been well established and studied since initially described by Gilling et al. [7] allows the surgeon to follow anatomic planes to separate entire lobes of the prostate, mimicking the action of the index finger in open simple prostatectomy. In general, these lobes are then liberated into the bladder with subsequent morcellation. HoLEP has been well demonstrated to be safe, effective and durable in all prostate volumes [8,9,10].
Similar to HoLEP, ThuLEP combines the blunt mechanical enucleation of tissue with a different wavelength to remove the prostatic adenoma. Thulium laser works at a wavelength of 2010 nm in continuous wave mode [11]. ThuLEP has been shown to have similar outcomes to HoLEP with the exception of hemostatsis [12].
Moreover, greenlight XPS uses a unique 532 nm KTP-LBO (potassium–titanyl–phosphate–lithium triborate) length laser. This wavelength freely travels through water (therefore, a non-contact procedure) and is selectively absorbed by hemoglobin which acts as an intravascular target for the light energy which greatly improves hemostasis [13]. Studies have demonstrated that greenlight PVP is safe and effective with significantly shorter catheterization and hospitalization times than TURP [14,15,16]. Greenlight can also be used for enucleation [17]. GreenLEP has been shown to be safe with similar effectiveness in the treatment of BPH when compared to HoLEP [18].
Aquablation (AQUABEAM System, PROCEPT BioRobotics, Inc., USA) is a robotically executed, surgeon-guided, high-velocity waterjet technology integrating real-time ultrasonography. Studies have shown the non-inferior symptom relief benefit of aquablation as compared to TURP, but with considerably lower resection times and low risks of sexual side effects, specifically ejaculatory function [19]. Aquablation’s effectiveness has also been shown in large prostates with analyses of trial data showing that the benefits observed in smaller prostates transfer to larger ones.
In this study, given the paucity of comparative performance between technologies, we sought to compare the procedural outcomes of high-volume, expert surgeons of each technique and mid-term improvement in international prostate symptom scores (IPSS) of aquablation, greenlight PVP, GreenLEP, HoLEP, and ThuLEP.
Methods
Data sources
Data for this study were pooled from five sources (further details below). All men had comparable diagnostic work-up for BPH according to EAU/AUA guidelines with preoperative assessment of symptom scores (IPSS), uroflow measures, post-void residual (PVR), cystoscopy and transrectal ultrasound (TRUS) for prostate volume assessment. Long-term outcomes were not included due to lack of consistent data collection.
Aquablation Individual patient-level data from the following four studies of the aquablation procedure were provided by the device manufacturer/study sponsor: (1) WATER (NCT02505919) [20], a double-blinded prospective international multicenter clinical trial of the aquablation procedure vs. standard transurethral resection of the prostate (TURP) in prostates measuring between 30 and 80 cc, (2) WATER II (NCT03123250) [21], a prospective international single-arm clinical study of the aquablation procedure in men with larger (80–150 cc) prostates, (3) WATER FRANCAIS (NCT03191734) [22], a prospective 3-center single-arm clinical trial conducted in France, and (4) Open WATER (NCT02974751), a prospective registry of outcomes of Aquablation in the commercial setting, conducted at five centers in the UK, Germany, Australia, New Zealand and Lebanon (enrollment complete and follow-up ongoing, unpublished). Additionally, data from the commercial experience of one high-volume user (TB) were added (unpublished full data set, but partial data set published on first 118 patients [23]).
Photo-vaporization of the prostate Patients undergoing standardized anatomic PVP with greenlight XPS at the University of Montreal Hospital Center between February 2011 and March 2019 were included. All procedures were performed by a single surgeon (KCZ) with greenlight laser experience since 2005. All greenlight XPS cases were conducted as previously described as outpatient, same-day surgery [24].
Greenlight laser enucleation of the prostate Patients underwent GreenLEP at Clinique Pasteur (Toulouse, France) between June 2013 and March 2019. The procedure, executed as described by Gomez-Sancha et al. [25], was performed by a single surgeon (VM) who has had laser experience since 2011.
Holmium laser enucleation of the prostate Patients underwent HoLEP at Indiana University Health Methodist Hospital (Indianapolis, USA) between April 2016 and April 2018. All procedures were performed by a single surgeon (JEL) who performed the first holmium enucleation prostatectomy in the United States in 1998 and completed > 2000 HOLEPs.
Thulium laser enucleation of the prostate Patients underwent ThuLEP at Asklepios Hospital Harburg (Hamburg, Germany) between January 2017 and March 2019 as described initially by Bach et al. in 2009 [12]. All procedures were performed by a single surgeon (TB), with enucleation experience since 2007.
Men with prostate volumes < 30 cc (5% for Aquablation, 2.7% for PVP, 0.5% for GreenLEP, 1% for HoLEP and 11.4% for thulium) were excluded from the analysis.
Procedural outcomes
The procedural rate (operative minutes per cc TRUS prostate volume) was calculated as operative time divided by measured TRUS baseline prostate volume. For aquablation, the total operative time was defined as the number of minutes from either the insertion of the TRUS probe or insertion of the aquablation handpiece (using the earlier of the two) to the catheter placement or removal of the TRUS probe (using the later of the two). This calculation was available in WATER, WATER II, and WATER FRANÇAIS studies as well as in commercial procedures. For Open WATER, total procedure time was estimated as minutes from handpiece in to catheter in. For PVP, total procedure time was calculated from camera entry to Foley placement. For the enucleation procedures (HoLEP, ThuLEP, and GreenLEP), total procedure time was calculated from the insertion of the scope to the completion of morcellation.
International prostate symptom score
IPSS were collected at baseline and at all post-operative follow-up visits. Unfortunately, not all centers used the same timepoints for IPSS assessments post-operatively. Given the variation in surgeon follow-ups, analysis of IPSS score changes was performed in patients with both baseline and follow-up scores where the follow-up score used was the latest of post-operative scores collected at least 1 month following surgery but not more than 12 months after surgery. Mean IPSS follow-up time was 8.7 months for aquablation, 2 months for GreenLEP, 8.5 months for HoLEP, 12 months for thulium and 7.6 months for PVP.
Statistical analysis
General linear models were used to evaluate the relationship between prostate volume (or other continuous predictors) and procedure time or other continuous outcome measures. Multivariate models were also used. A p value ≤ 0.05 was considered statistically significant. All statistical analyses were performed using R on the R studio platform.
Results
Compared to aquablation, those undergoing GreenLEP, HoLEP and ThuLEP were slightly older (by 1.2, 2.1, and 3.7 years, respectively). Men undergoing aquablation, PVP, GreenLEP, HoLEP, and ThuLEP had mean prostate volumes of 71.7 cc, 79.6 cc, 97.4 cc, 116.1 cc and 75.7 cc, respectively (Table 1).
Procedural outcomes
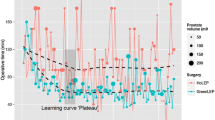
Total procedure time was strongly related to prostate size (p < 0.0001, Fig. 1); except for the small prostate size range (size < 40 cc), at any given prostate volume, procedure time was highest for PVP, intermediate for LEPs, and lowest for aquablation. Procedure time of the approach and prostate size can be found in Table 2. The relationship between procedure time and prostate size (i.e., slope of the fitted lines) was 0.16 min/g for aquablation, 0.32 min/g, 0.28 min/g and 0.32 min/g for GreenLEP, HoLEP and ThuLEP, respectively, and 0.63 min/g for PVP.
After controlling for prostate volume, the addition of baseline PSA, age, and body mass index to statistical models did not further predict procedure time. In stepwise selection models, prostate volume was the strongest predictor of total procedure time for each procedure (p < 0.0001 for all procedures except thulium, where p = 0.0021).
IPSS scores were available at both baseline and follow-up (minimum 1 month, maximum 12 months) in 511/608 (84%) of treated aquablation patients, 490/608 (81%) PVP patients, 125/365 (34%) GreenLEP patients, 85/221 (38%) HoLEP patients and 113/272 (42%) thulium patients. Baseline scores were highest for the PVP group and lowest for the GreenLEP group (Fig. 2); follow-up scores were low in all groups. All change scores were highly statistically significant (< 0.001) (Fig. 3).
Discussion
In this study, we compared procedural parameters and mid-term improvement in IPSS of four commonly performed procedures (Greenlight PVP, GreenLEP, HoLEP, and ThuLEP) and a newer procedure, aquablation. The aquablation procedure had the lowest total procedure time across all prostate sizes and the lowest slope (i.e., increase in procedure time per extra gram of tissue). ThuLEP and Greenlight PVP had the longest procedures for prostate sizes < 40 cc and > 40 cc, respectively.
As expected, prostate volume was the strongest predictor of total procedure time. Greenlight PVP’s operative time was the most affected by an increase in prostate size, as shown by its highest slope value (0.63 min/g by TRUS volume). This can be explained by the greenlight energy being fully transmitted to tissue during vaporization. Aquablation’s operative time was the least affected by an increase in prostate size with a slope value of 0.16 min/g (3.93 times faster than PVP). This can be explained by the fact that the process to prepare to the resect tissue is the same regardless of prostate size. Then the tissue resection is performed robotically that takes approximately 5 minutes regardless of prostate size. This is in line with a previous analysis of aquablation surgical times comparing prostates < 100 cc and > 100 cc. This analysis showed a volume-independent rapid ablation of prostate tissue with a mean resection time, for the smaller and larger prostates, of 6.4 min and 9.1 min, respectively [26]. In aquablation, the duration of resection is dictated by the length of the prostate. The waterjet rotates and transverses at a constant speed regardless of depth.
Across all prostate sizes, aquablation had significantly shorter operative time despite limited previous experience. All 14 WATER sites and 9 out of 16 WATER II sites had never performed an aquablation procedure before enrolling their first patient in these trials. This is in contrast with the other approaches analyzed in this study which were all executed by surgeons with significant expertise in each technique.
Advantages of our study include its large sample size and use of standardized measures (prostate volume as estimated by TRUS, symptom scores measured with IPSS). Disadvantages include its retrospective design. While comparative effectiveness was beyond the scope of this study and the focus of this paper was on short-term and procedural outcomes, additional limitations include the limited follow-up for long-term outcomes and heterogeneous data collection of long-term outcomes. Characterization of the median lobe and anticoagulation varied by data source, making it difficult for any analysis of its potential impact on procedure times and symptom responses. An additional limitation of our study is the different study designs pooled. For example, part of the data pooled for aquablation is from the WATER trials which had high considerations for accuracy than prospectively maintained institutional databases. Unfortunately, data collection methods were also too disparate to estimate the impact of technology choice on adverse event rates as well as consistent post-operative assessments with IPSS. As large tertiary centers were considered for procedural referral, the follow-up timepoints were not consistent at all centers. Additionally, pooling data from several centers in different countries further limits the generalizability of our results. Nevertheless, in expert hands, all technologies/techniques provided comparable significant IPSS improvements compared to baseline. Aquablation data came from > 20 surgeon users whereas PVP, GreenLEP, HoLEP and ThuLEP data were derived from highly experienced individual experts. Procedure times for these latter technologies could be longer for less experienced users. However, in the context of this study, these limitations do not impact the key findings considering that the quickest procedure was still the more recent aquablation.
Conclusions
In our analysis of pooled data of multi-surgical techniques and technologies performed by high-volume experts, Aquablation demonstrated the lowest operative time across all prostate volumes. Such findings are valuable when counseling men and planning anesthesia time for respective BPH procedures; however, they need to be considered along with other factors such as complications and re-intervention rates.
References
Lue TF, McAninch JW (eds) (2013) Smith & Tanagho's general urology. McGraw-Hill Medical
Vuichoud C, Loughlin KR (2015) Benign prostatic hyperplasia: epidemiology, economics and evaluation. Can J Urol 22(Suppl 1):1–6
Foster HE, Barry MJ, Dahm P, Gandhi MC, Kaplan SA, Kohler TS, Lerner LB, Lightner DJ, Parsons JK, Roehrborn CG, Welliver C, Wilt TJ, McVary KT (2018) Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline. J Urol 200(3):612–619
Nickel JC, Aaron L, Barkin J, Elterman D, Nachabé M, Zorn KC (2018) Canadian Urological Association guideline on male lower urinary tract symptoms/benign prostatic hyperplasia (MLUTS/BPH): 2018 update. Can Urol Assoc J 12(10):303–312. https://doi.org/10.5489/cuaj.5616
Gratzke C, Bachmann A, Descazeaud A et al (2015) EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 67(6):1099–1109. https://doi.org/10.1016/j.eururo.2014.12.038
Kuntz RM (2006) Current role of lasers in the treatment of benign prostatic hyperplasia (BPH). Eur Urol 49(6):961–969. https://doi.org/10.1016/J.EURURO.2006.03.028
Le Duc A, Gilling PJ (1999) Holmium laser resection of the prostate. Eur Urol 35(2):155–160. https://doi.org/10.1159/000019836
Wilson LC, Gilling PJ, Williams A et al (2006) A randomised trial comparing holmium laser enucleation versus transurethral resection in the treatment of prostates larger than 40 grams: results at 2 years. Eur Urol 50(3):569–573. https://doi.org/10.1016/J.EURURO.2006.04.002
Krambeck AE, Handa SE, Lingeman JE (2010) Experience with more than 1000 holmium laser prostate enucleations for benign prostatic hyperplasia. J Urol 183(3):1105–1109. https://doi.org/10.1016/j.juro.2009.11.034
Ahyai SA, Gilling P, Kaplan SA et al (2010) Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol 58(3):384–397. https://doi.org/10.1016/J.EURURO.2010.06.005
Herrmann TRW, Bach T, Imkamp F et al (2010) Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. Introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol. 28(1):45–51. https://doi.org/10.1007/s00345-009-0503-0
Bach T, Netsch C, Haecker A, Michel M-S, Herrmann TRW, Gross AJ (2010) Thulium:YAG laser enucleation (VapoEnucleation) of the prostate: safety and durability during intermediate-term follow-up. World J Urol 28(1):39–43. https://doi.org/10.1007/s00345-009-0461-6
Sachs B, Misrai V, Tabatabaei S, Woo HH (2019) Multicenter experience with photoselective vaporization of the prostate on men taking novel oral anticoagulants. Asian J Urol. https://doi.org/10.1016/J.AJUR.2019.07.005
Hueber PA, Liberman D, Ben-Zvi T, Woo H, Hai MA, Te AE, Chughtai B, Lee R, Rutman M, Gonzalez RR, Barber N, Al-Hathal N, Al-Qaoud T, Trinh QD, Zorn KC (2013) 180 W vs 120 W lithium triborate photoselective vaporization of the prostate for benign prostatic hyperplasia: a global, multicenter comparative analysis of perioperative treatment parameters. Urology 82(5):1108–1113
Thomas JA, Tubaro A, Barber N et al (2016) A multicenter randomized noninferiority trial comparing greenlight-XPS laser vaporization of the prostate and transurethral resection of the prostate for the treatment of benign prostatic obstruction: two-yr outcomes of the GOLIATH study. Eur Urol 69(1):94–102
Ajib K, Mansour M, Zanaty M et al (2018) Photoselective vaporization of the prostate with the 180-W XPS-Greenlight laser: five-year experience of safety, efficiency, and functional outcomes. Can Urol Assoc J 12(7):E318–E324. https://doi.org/10.5489/cuaj.4895
Huet R, Mathieu R, Verhoest G, Bensalah K, Vincendeau S (2015) Énucléation prostatique au laser Greenlight (GreenLEP) versus Photovaporisation prostatique (PVP) GreenlightXPS 180 W pour les volumes de %3e 80 mL : étude monocentrique comparative et prospective des résultats péri-opératoires et fonctionnels à moyen terme. Progrès en Urol 25(13):732. https://doi.org/10.1016/J.PUROL.2015.08.034
Elshal AM, Elkoushy MA, El-Nahas AR et al (2015) GreenLightTM Laser (XPS) photoselective vapo-enucleation versus holmium laser enucleation of the prostate for the treatment of symptomatic benign prostatic hyperplasia: a randomized controlled study. J Urol 193(3):927–934. https://doi.org/10.1016/J.JURO.2014.09.097
Gilling PJ, Barber N, Bidair M et al (2019) Randomized controlled trial of aquablation versus transurethral resection of the prostate in benign prostatic hyperplasia: one-year outcomes. Urology 125:169–173. https://doi.org/10.1016/J.UROLOGY.2018.12.002
Gilling P, Barber N, Bidair M et al (2018) WATER: a double-blind, randomized, controlled trial of aquablation vs transurethral resection of the prostate in benign prostatic hyperplasia. J Urol 199(5):1252–1261. https://doi.org/10.1016/j.juro.2017.12.065
Desai M, Bidair M, Bhojani N et al (2018) WATER II (80–150 mL) procedural outcomes. BJU Int. https://doi.org/10.1111/bju.14360
Misrai V, Rijo E, Zorn KC, Barry-Delongchamps N, Descazeaud A (2019) Waterjet ablation therapy for treating benign prostatic obstruction in patients with small- to medium-size glands: 12-month results of the first french aquablation clinical registry. Eur Urol. https://doi.org/10.1016/J.EURURO.2019.06.024
Bach T, Giannakis I, Bachmann A et al (2018) Aquablation of the prostate: single-center results of a non-selected, consecutive patient cohort. World J Urol. https://doi.org/10.1007/s00345-018-2509-y
Azizi M, Tholomier C, Meskawi M et al (2017) Safety, perioperative, and early functional outcomes of vapor incision technique using the greenlight XPS 180 W system: direct comparison with photoselective vaporization of the prostate. J Endourol 31(1):43–49. https://doi.org/10.1089/end.2016.0474
Gomez Sancha F, Rivera VC, Georgiev G, Botsevski A, Kotsev J, Herrmann T (2015) Common trend: move to enucleation—is there a case for GreenLight enucleation? Development and description of the technique. World J Urol 33(4):539–547. https://doi.org/10.1007/s00345-014-1339-9
Bhojani N, Nguyen D-DD, Kaufman RP, Elterman D, Zorn KC (2019) Comparison of %3c 100 cc prostates and %3e 100 cc prostates undergoing aquablation for benign prostatic hyperplasia. World J Urol 37(7):1361–1368. https://doi.org/10.1007/s00345-018-2535-9
Funding
WATER, WATER II, OPEN WATER, and FRANCAIS WATER clinical studies were funded by PROCEPT BioRobotics.
Author information
Authors and Affiliations
Contributions
D-DN: protocol/project development, data analysis, manuscript writing. VM: data collection, manuscript editing. TB: data collection, manuscript editing. NB: manuscript editing. JEL: data collection, manuscript editing. DSE: manuscript editing. KCZ: protocol/project development, data collection, data management, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
Consultants and proctors for Boston Scientific for greenlight: KZ, DE, VM. Investigators and consultants for PROCEPT BioRobotics: VM, TB, NB, KZ. DDN were supported by a summer scholarship from the Endourological Society.
Research involving human participants and/or animals
This research involves humans.
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nguyen, DD., Misraï, V., Bach, T. et al. Operative time comparison of aquablation, greenlight PVP, ThuLEP, GreenLEP, and HoLEP. World J Urol 38, 3227–3233 (2020). https://doi.org/10.1007/s00345-020-03137-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03137-8