Abstract
Purpose
To present the author’s experience with detrusorotomy (DM) for refractory detrusor overactivity (RDO) with open and robotic approach.
Methods
Children who underwent DM for RDO in a single surgeon series since 2012 were identified from a prospectively maintained database. Those who completed the defined strict bladder cycling regime postoperatively were included in this report excluding those who failed the bladder cycling regime.
Results
Ten children (M7: F3) were included in this report, six open and four robotic. All procedures were completed with no conversion to open in the robotic group. There were no intra or postoperative complications from the procedures. Duration of procedure was lower in robotic group (125 min) vs the open group at (208 min). Hospital stay was also lower in the robotic group (2.7 days) compared to the open group (5.6 days). All children in open group had concomitant Mitrofanoff channel created for bladder drainage. One child in robotic group had concomitant Mitrofanoff channel during DM. Median follow-up is longer at 54 months (31–82) in open group compared to 14 months (5–21). All children are clinically well with safe upper tracts on US scan in both series. Estimated % change in bladder capacity is similar in both groups at 140 (90–200) and 126 (80–200) for open and robotic groups, respectively.
Conclusions
DM as an extension of medical treatment for RDO can be performed safely and is effective in children. Preliminary experience with robotic approach to DM is promising with reduced duration of procedure and hospital stay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Enterocystoplasty (EC) has transformed the life of many children with end stage bladder disease by incorporating a bowel segment to improve the compliance and capacity of the native bladder [1]. The introduction of bowel into the urinary tract is not without its attendant consequences which are well recognised [2, 3]. Alternatives to EC are those procedures that do not incorporate bowel into the urinary tract and Detrusorotomy (DM) is one such option [4].
DM, also known as auto-augmentation, has been attempted by many authors with varied success [5]; experience reported thus far seems to suggest DM is most effective when the bladder has not deteriorated to the extreme [6]. DM has largely been performed by an open incision with few attempting a minimally invasive approach [7]. This is a report of DM as an option for Refractory Detrusor overactivity (RDO) and the first report of DM by robotic approach as regards technique of DM.
Methods
The database of children who underwent DM were prospectively created since early 2012. All DM procedures were performed by the open approach up until early 2017 (open) and subsequently by the robotic approach (robotic). Indication for DM in all these cases was RDO. RDO is defined as detrusor overactivity not controlled with conservative management including anticholinergics with reduced bladder capacity for age and rising detrusor pressures with potential to affect the upper tracts. Formal invasive urodynamics were only done preoperatively as a routine. Postoperatively, children are followed up closely in the clinic and outcomes were assessed by evaluation of the clinical status, non-invasive bladder and upper urinary tract assessments to assess change in bladder capacity, intraoperative complications and need for conversion to EC.
The open approach was done via a pfannenstiel incision and the robotic approach involved one camera port in the epigastric region and two working ports in the left and Right hypochondrium to facilitate optimum access without being too close to the target organ, the bladder.
The DM was performed in the coronal plane for all the children in the series (Fig. 1) except for one child in the robotic group, where DM was done in the anteroposterior sagittal plane (Fig. 2). This child had a previous Mitrofanoff fashioned along right side of posterior wall. The exposed bladder mucosa in all cases was left covered with peritoneum with no additional supporting layer as demonstrated in the accompanying video (Video 1).
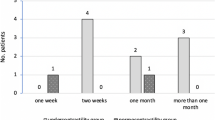
A strict regime of bladder cycling was instituted in the postoperative phase with 15-min clamp and release starting post op day 2. The clamp duration was increased incrementally by 15 min until 1-hour clamp duration followed by 30-min increments with a view to get to 3-hour clamp and 15-min release over a period of 2–3 weeks. This regime was monitored by clinical nurse specialists but carried out by caregivers at home after discharge from hospital.
Results
A total of 12 children were identified from the database, 8 M and 4 F. Two children, one boy and one girl, were excluded as they did not cooperate with bladder cycling regime and thus the outcomes from DM cannot be assessed. Therefore ten children who completed their bladder cycling program postoperatively were included in this study, six open and four robotic. All procedures were completed successfully with no intra or post-operative complications.
Table 1 shows the details of both groups with follow-up outcomes. All children have a safe and stable appearance of the upper tracts on US scan with no new significant hydronephrosis or complete resolution of hydronephrosis compared to preoperative status. Figure 3 shows a bladder outline from a case in the open series and Fig. 4 shows the bladder outline on a case from the robotic series. Follow-up in the open series is longer than the robotic series for obvious reasons. None of the patients in either group needed an EC yet (as of the last follow-up).
Discussion
The inference from this report is DM is effective for RDO whilst demonstrating the feasibility of robotic approach for DM without any increase in morbidity and with reduced hospital stay for the cases in robotic group as compared to the open group. The outcomes of DM are otherwise similar in both groups although the follow-up is shorter in the robotic group.
As regards the procedure of DM itself, it is fair to say the indications for this procedure are not well defined making it difficult to compare different published materials. The main issue revolves around the philosophy of approach and this is outlined by Kumar et al. in their report whereby they describe DM as a bridge between medical and surgical management options for RDO [6].
Over the years since its first description by Cartwright [8], there has been scepticism on the role of and benefit from DM [9, 10], mainly due to lack of clarity on how to define a “bladder that has not deteriorated”. Attempts at DM with a view to enlarge the bladder have not met with success with resultant conversion to EC. However, performing DM early as an extension of medical treatment has allowed the author to realise the true potential as evident in the outcomes presented in Table 1. This is particularly true of the cases in the open group, where the longest follow-up is 82 months with a median of 54 months. None of the patients in this series in either group have needed any additional procedures such as EC to keep the diseased bladder compliant in contrast to some published material [5, 9,10,11].
One important aspect of DM is the issue around keeping the bladder distended to allow it to reconfigure following division of the detrusor muscle in the bladder wall. Some have advocated the use of balloon device to keep the bladder distended in the postoperative phase [12]; however, the author believes in early cycling of the bladder for the procedure of DM to achieve its true potential. This obviates the need for an additional device in the bladder.
The technique of DM demands meticulous dissection of individual detrusor fibres and the robotic approach certainly provides enhanced magnification along with other inherent benefits from this technology to facilitate the procedure. The ability to access structures like the bladder deep within the pelvis is a hallmark of this technology allowing early recovery for the patients by obviating the need for invasive surgical incision on the abdominal wall. Hospital stay in the robotic series is considerably shorter than the open group although statistically not meaningful to compute a p value given small numbers.
There have been no intra or postoperative complications in both groups of this series and that is mainly due to meticulous attention to technique together with attempting DM early before bladder is deteriorated. By not having a perforation of the bladder mucosa intraoperatively, early cycling of the bladder has been achieved in all these cases and that must contribute to the outcomes reported in the author’s experience. However, should a perforation occur, it should be sealed immediately with preferably absorbable monofilament suture. The surgeon has then to decide if DM needs to be done at a different site, but that judgement depends on the expertise of the surgeon concerned. Djordjevic et al. have suggested a rectus muscle backing to provide support to the bulging bladder mucosa [13].
Various options for management of RDO have been described, both medical and surgical. One medical option is intravesical injection of Botox into the detrusor muscle with variable success rates in published literature [14]. However, Botox therapy necessitates repeated injections at regular intervals and there are reports of the lasting duration of its effect decreasing with repeated injections [15].
Medical treatment is appropriately the first line in the management of neurogenic bladder. Verpoorten [16] suggests with early aggressive medical treatment, children with neurogenic bladder should no longer require surgical bladder augmentation to achieve safe urinary continence in adolescence and adulthood. On the other hand, published PHIS (Pharmaceutical health information system, USA) data reveal incidence of EC has not decreased over time [17]. For the vast majority of surgeons, the default position is to perform EC as the preferred surgical procedure for RDO, having stood the test of time with reproducible results for increasing bladder capacity and improving compliance to allow safe storage of urine at low pressure [1].
On balance, early aggressive medical management and surgical treatment by EC are options at the two ends of the timeline depending on success of medical therapy and progression towards end stage bladder disease. Role of DM should not be aimed at replacing EC as an alternative procedure as perceived by many authors [9, 10] but as an option to try and reduce the use of bowel within the lower urinary tract. With that approach, DM is an extension of medical treatment or a bridge between Botox therapy and EC [6].
Those who are sceptical about the role of DM need to reflect on the current situation with EC as the only procedure to manage poorly compliant bladders is an extreme viewpoint and surely even if a handful of patients within that cohort can be managed without EC, that is certainly a game changer to avoid the sequelae of EC in the longer term. To speculate further, even in the longer term if the DM rate is only about 20% as a minimum, it will be considered a success and paradigm shift in management of RDO. However, for this to occur, there needs to be a concerted effort for many more clinicians to try DM as a possible intermediary early option and not as an alternative to EC for end stage bladder disease. There is also a need to define its indications but that will almost certainly happen when DM gets established and accepted widely.
The limitation to this study is certainly due the small cohort of patients in this series and time will only tell whether the outcomes can be reliably produced with a larger cohort. This is particularly true of the robotic approach for DM, where follow-up is shorter than the open series for obvious reasons. The children are closely followed up clinically by the author with routine US scan and non-invasive bladder evaluation and hopefully longer-term data on follow-up will be available in due course.
Conclusion
In conclusion, DM is an effective option to be considered early in the timeline of management of RDO and increased bladder capacity. DM should be considered an extension of medical treatment before bladder deteriorates and not as an alternative to EC. This study also demonstrates that DM can be safely performed in children by the robotic approach without any increase in morbidity but with reduced duration of procedure and shorter hospital stay compared to open approach. This is a small series and larger numbers with longer follow-up will be needed for this mode of treatment to be widely accepted.
References
Biers SM, Venn SN, Greenwell TJ (2012) The past, present and future of augmentation cystoplasty. BJU Int 109:1280–1293. https://doi.org/10.1111/j.1464-410X.2011.10650.x
Mundy AR (1999) Metabolic complications of urinary diversion. Lancet 353:1813–1814
Stein R, Rubenwolf P (2014) Metabolic consequences after urinary diversion. Front Pediatr 2:15. https://doi.org/10.3389/fped.2014.00015
Hansen EL, Hvistendahl GM, Rawashdeh YFH, Olsen LH (2013) Promising long-term outcome of bladder autoaugmentation in children with neurogenic bladder dysfunction. J Urol. https://doi.org/10.1016/j.juro.2013.05.035
González R, Ludwikowski BM (2013) Alternatives to conventional enterocystoplasty in children: a critical review of urodynamic outcomes. Front Pediatr. https://doi.org/10.3389/fped.2013.00025
Kumar SPV, Abrams PH (2005) Detrusor myectomy: long-term results with a minimum follow-up of 2 years. BJU Int 96:341–344
Poppas DP, Uzzo RG, Britanisky RG et al (1996) Laparoscopic laser assisted auto-augmentation of the pediatric neurogenic bladder: early experience with urodynamic followup. J Urol. https://doi.org/10.1016/S0022-5347(01)66390-0
Cartwright PC, Snow BW (1989) Bladder autoaugmentation: early clinical experience. J Urol 142:505–508 (discussion 520–1)
Marte A, Di Meglio D, Cotrufo AM et al (2002) A long-term follow-up of autoaugmentation in myelodysplastic children. BJU Int. https://doi.org/10.1046/j.1464-410X.2002.02781.x
MacNeily AE, Afshar K, Coleman GU, Johnson HW (2003) Autoaugmentation by detrusor myotomy: its lack of effectiveness in the management of congenital neuropathic bladder. J Urol 170:1643–1646. https://doi.org/10.1097/01.ju.0000083800.25112.22(discussion 1646)
Gurocak S, De Gier RPE, Feitz W (2007) Bladder augmentation without integration of intact bowel segments: critical review and future perspectives. J Urol 177:839–844
Rocha FT, Bruschini H, Figueiredo JA et al (2011) Use of an inflatable silicone balloon improves the success rate of bladder autoaugmentation at long-term followup. J Urol 185:2576–2581
Djordjevic ML, Vukadinovic V, Stojanovic B et al (2015) Objective long-term evaluation after bladder autoaugmentation with rectus muscle backing. J Urol. https://doi.org/10.1016/j.juro.2014.11.081
Gamé X, Mouracade P, Chartier-Kastler E et al (2009) Botulinum toxin-A (Botox®) intradetrusor injections in children with neurogenic detrusor overactivity/neurogenic overactive bladder: a systematic literature review. J Pediatr Urol 5:156–164
Altaweel W, Jednack R, Bilodeau C, Corcos J (2006) Repeated intradetrusor botulinum toxin type A in children with neurogenic bladder due to myelomeningocele. J Urol 175:1102–1105. https://doi.org/10.1016/S0022-5347(05)00400-3
Verpoorten C, Buyse GM (2008) The neurogenic bladder: medical treatment. Pediatr Nephrol 23:717–725. https://doi.org/10.1007/s00467-007-0691-z
Lendvay TS, Cowan CA, Mitchell MM et al (2006) Augmentation cystoplasty rates at children’s hospitals in the United States: a pediatric health information system database study. J Urol 176:1716–1720. https://doi.org/10.1016/S0022-5347(06)00615-X
Author information
Authors and Affiliations
Contributions
I (RS) am the sole author for this manuscript and responsible for all aspects of this manuscript including data analysis and writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
I have no disclosures and no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (M4 V 266844 kb)
Rights and permissions
About this article
Cite this article
Subramaniam, R. Experience with detrusorotomy in children by open and robotic approach. World J Urol 38, 1869–1874 (2020). https://doi.org/10.1007/s00345-019-02777-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02777-9