Abstract
Purpose
To examine the complications and functional outcomes of high-risk patients on antithrombotic therapy (ATT) treated with photoselective vaporization of the prostate (PVP) using the Greenlight (GL) XPS-180 system.
Methods
A retrospective analysis of prospectively maintained institutional database was performed. Men with symptomatic LUTS related to BPH were treated with 523-nm GL PVP using the XPS-180 W system. They were stratified according to ATT status: group 1 (control group), group 2 (acetylsalicylic acid), group 3 (antiplatelet agents other than acetylsalicylic acid) and group 4 (anticoagulation agents). Postoperative adverse events at 30- and 90-days were prospectively recorded. Complications were stratified according to the Clavien-Dindo classification. Additionally, functional outcomes (IPSS, Qmax and PVR) were analyzed up to 48 months of follow-up after surgery. Multivariable logistic regression analyses were used to predict the effect of ATT on serious bleeding-associated complications that was defined as the sum of patients with hematuria Clavien grade ≥ 2, patients requiring transfusions and patient with postoperative hemoglobin drop ≥ 15 g/dl.
Results
274 (63%), 87 (21%), 24 (6%) and 37 (9%) patients were included in groups 1, 2, 3 and 4, respectively. Patients on antiplatelet (group 3) and anticoagulant medication (group 4) were older (median age 60 vs. 68 vs. 77 vs. 76 years, p < 0.001) and had more comorbidities (ASA 3–4: 9.5 vs. 27.6 vs. 66.7 vs. 64.9%; p < 0.001) than their counterparts. The overall 30-day complications rates were 31, 28.7, 45.8 and 45.9% of patients included in groups 1, 2, 3 and 4, respectively (p = 0.4). Hematuria Clavien 1 events (p < 0.001), readmissions rates (p = 0.02), length of post-operative hospital stay (p < 0.001) and catheterization time (p < 0.001) were significantly higher in patients on antiplatelet and anticoagulation medication. In multivariable analyses, ATT status was not a predictor of serious bleeding events after surgery (p > 0.5). Finally, functional outcomes were significantly improved accross the four groups.
Conclusion
GL PVP is safe and effective in treating high-risk patients on ATT. Although serious bleeding complications are rare and equivalent with non-high-risk patients, patients on antiplatelet and anticoagulation medication should be counseled on the increased risk of minor bleeding events and readmissions rates at 30 days after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Greenlight (GL) photoselective vaporization of the prostate (PVP) using the XPS 180 W system is a surgical treatment option for men with lower urinary tract symptoms (LUTS) secondary to benign prostate hyperplasia (BPH) [1, 2]. Randomized controlled trial data have demonstrated a similar 24-month efficacy and safety for GL PVP compared to the surgical gold standard transurethral resection of the prostate (TURP) in non-high-risk patients [3].
Given the fact that GL PVP provides excellent hemostatic potential compared to TURP [4], several investigators have evaluated the efficacy and safety of GL PVP in patients on antithrombotic therapy (ATT) [5,6,7,8]. However, limited quantity and quality of data have been the major drawbacks against the adoption of GL PVP as standard of care for management of high-risk patients with cardiovascular disease necessitating ATT [9].
Based on these considerations, we examined the safety of PVP in patients on ATT. More specifically, we sought to focus on bleeding-related complications, stratified according to Clavien-Dindo grading system, and long-term efficacy and durability of GL PVP in patients on ATT at 2 years.
Materials and methods
Patient population
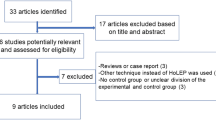
After obtaining institutional review board approval, we conducted a retrospective study of prospectively collected data of patients treated with GL PVP for benign prostate hyperplasia (BPH) using the XPS-180 W system (Boston Scientific, Boston, MA, USA). Surgeries were performed at a tertiary medical center between 2011 and 2016 by an expert high-volume surgeon. Inclusion criterion was all patients treated with GL PVP for symptomatic BPH. Exclusion criteria were patients with unknown coagulation status (n = 2) and patients treated with 120-W HPS system. Treatment indications were in accordance with the American, Canadian and European clinical practice guidelines [1, 2, 10].
Surgical technique
All patients underwent a 532-nm-laser PVP with GL 180 W XPS under general or spinal anesthesia as previously described [11]. Following the procedure, a 2-way 22 F silicone Foley catheter was inserted with a 30-cc balloon post-operatively and removed at the surgeon’s discretion typically 24 h after the procedure [12].
Antithrombotic status
ATT status was recorded preoperatively. Patients were stratified into four groups. Specifically, group 1 included patients without antithrombotic agents (control group). Group 2 included patients on acetylsalicylic acid. Group 3 included patients on antiplatelet agents other than acetylsalicylic acid such as clopidogrel, ticlopidine or ticagrelor. Additionally, group 3 encompassed patients on combined antiplatelet agents: acetylsalicylic acid and clopidogrel (n = 13). Group 4 included patients on anticoagulants medication: vitamin K antagonists (warfarin), direct thrombin inhibitor (dabigatran), direct factor Xa inhibitors (rivaroxaban and apixaban) and low-molecular weight heparin.
In general, decision to stop anticoagulant and antiplatelet agents was based on cardiology/internal medicine team recommendations. Specifically, acetylsalicylic acid and antiplatelet agents were stopped 5–7 days before surgery. Oral anticoagulants drugs were stopped 2–5 days before the procedure. Patients with mechanical valve disease (n = 9) and with atrial fibrillation (n = 21) were bridged with heparin or low-molecular weight heparin until 4–12 h before the surgery. All types of ATT (group 2, 3 and 4) were resumed within 24 h after the procedure. No patients were on non-steroidal anti-inflammatory medication.
Covariates
All men in the study underwent preoperative evaluation recommended by the American Urologic Association (AUA) prior to undergoing surgical intervention. Preoperative variables included: patients’ age, body mass index (BMI), comorbidity score stratified according to the American society of anesthesiology (ASA), previous history of BPH surgery, BPH medication use and preoperative retention status. Prostate volume was measured using a transrectal ultrasonography (TRUS). Additionally, operative characteristics were also recorded: operative time (min), lasing time (min), energy use (kJ), energy density (kJ/cc) as well as number of irrigation bags used during the procedure.
Endpoints
The primary endpoints of the study were the incidence of intraoperative and postoperative adverse events recorded at 30- and 90-days after PVP. Specifically, we examined bleeding complications stratified according to ATT status: intraoperative bleeding, postoperative hematuria, transfusions rates and hemoglobin drop after the surgery. The latter was calculated by subtracting recovery room hemoglobin value from preoperative value. All complications were graded according to Clavien-Dindo classification. [13].
The secondary endpoints of the study were improvements in symptoms score [international prostate symptoms score (IPSS)], and quality of life (QoL) as well as uroflowmetry parameters [Qmax and post void residual (PVR)]. Additionally, prostate-specific antigen (PSA) reduction was also recoded. Finally, treatment failure was defined as the need for second BPH surgery or the use of intermittent or permanent urinary catheter after surgery. Patients were followed at 3, 6 and 12 months after surgery, and then annually thereafter.
Statistical analyses
Descriptive statistics focused on frequencies and proportions for categorical variables. Means, medians and interquartile range were reported for continuous variables. The Wilcoxon signed-rank and Chi square test were used to compare statistical significance of differences in medians and proportions, respectively.
We have defined a composite variable of serious bleeding events after PVP. This variable was calculated as the sum of patients with hematuria Clavien grade ≥ 2, patients requiring transfusions and patient with postoperative hemoglobin drop ≥ 15 g/dl. This cutoff was chosen as the median of hemoglobin drop following surgery. Multivariable logistic regression analyses were fitted to predict the effect of ATT status on patients with serious bleeding events. Adjustment was made for age, TRUS prostate volume, ASA score, use of 5 alpha reductase inhibitors as well as preoperative retention status.
All statistical tests were performed using R software environment for statistical computing and graphics (Vienna, Austria, version 3.0.1). All tests were two sided with a significance level set at p < 0.05.
Results
Baseline characteristics
Descriptive statistic of patients demographic stratified according to ATT status is summarized in Table 1. Overall, 422 patients were treated with Greenlight 180 W XPS PVP for BPH. Specifically, 21 (n = 87), 6 (n = 24) and 9% (n = 37) of patients were on acetylsalicylic acid (group 2), antiplatelet agents (group 3) and anticoagulation medication (group 4), respectively. The median follow-up was 24 months (range 3- 60 months). Patients in groups 3 (median age: 77 years) and 4 (median age: 76 years) were older than patients in groups 1 (median age: 60 years) and 2 (median age: 68 years; p < 0.001). Additionally, patients on antiplatelet (group 3: ASA 3–4: 66.7%) or anticoagulation agents (group 4: ASA 3–4: 64.9%) were sicker than their counterparts (ASA 3–4: 9.5% for group 1 and 27.6% for group 2; p < 0.001). TRUS prostate volume was higher in group 3 patients (median: 86 cc) compared to the other groups (median: 61–67 cc; p = 0.02). No statistically significant differences between the four strata were recorded for BMI, preoperative retention status and BPH medication use (alpha blockers or 5 alpha reductase inhibitors).
Intraoperative parameters are described in Table 2. The median operative time, lasing time and energy density were not statistically significant between the four groups. Conversely, patients on antiplatelet agents (group 3) consumed more irrigation bags (median: 6 vs. 4–5 bags for the other groups) during the procedure (p = 0.02).
Adverse events
Postoperative adverse events are shown in Table 3. The overall 30-day complications rates were 31, 28.7, 45.8 and 45.9% of patients included in groups 1, 2, 3 and 4, respectively (p = 0.4). The 30-day readmission rates were higher in groups 3 (12.5%) and 4 (16.2%; p = 0.02). Regarding bleeding complications, hematuria grade I rates were higher in patients on antiplatelet (group 2: 25%) and anticoagulation agents (group 4: 27%) relative to patients on acetylsalicylic acid (group 2: 9.2%) and control patients (group 1: 8.4%; p < 0.001). Conversely, no statistically significant difference was recorded for hematuria grade 2. Only one patient on anticoagulation agents required a surgical intervention to stop the bleeding postoperatively (p = 0.02). The median hemoglobin drops after surgery was similar among the 4 groups (p = 0.8). Two patients with baseline hemoglobin value of 80 g/dl required blood transfusion after surgery. Serious bleeding events were present in 16.8, 16.1, 16.7 and 10.8% of patients included in groups 1, 2, 3 and 4, respectively. In multivariable logistic regression analyses (Table 4) after adjustment for all covariates, antithrombotic therapy status was not a predictor of increased serious bleeding events after PVP (all p > 0.5). Similarly, all other variables included in the multivariable analyses did not reached statistically significant differences. Hospital stay and catheterization time were longer in patients included in groups 3 and 4 (p < 0.001).
Efficacy and retreatment rates
Following PVP, IPSS was significantly decreased compared to baseline at all follow-up endpoints in the four groups (Fig. 1a). Similarly, uroflowmetry parameters (Qmax and PVR) were also significantly improved after surgery at all endpoints (Fig. 1b/c). PSA significantly decreased after surgery compared to baseline at all endpoints (Fig. 1d). PSA reduction rates at 12 months after surgery were 56, 51, 72 and 51% for patients in groups 1, 2, 3 and 4, respectively.
Retreatment rates were 1.5, 0, 4.2 and 0% for patients in groups 1, 2, 3 and 4, respectively (p = 0.3). Furthermore, 4, 3.4, 4.2 and 2.7% of patients in groups 1, 2, 3 and 4 required long-term intermittent or permanent catheterization (p = 0.9).
Discussion
Our results demonstrated that patients on antiplatelet and anticoagulation medications are not at increased risk of significant bleeding events [OR: 1.53 (antiplatelet vs. control) and OR: 0.84 (anticoagulation vs. control); all p > 0.5]. However, group 3 (25%) and group 4 (27%) experienced a higher rate of post-operative hematuria grade 1 relative to patients on acetylsalicylic acid (9.2%) and control patients (8.4%; p < 0.001). These increased rates of hematuria grade 1 translated into increased rates of emergency department visit or hospital admission (30-day readmissions rates 4 (group 1) vs. 8 (group 2) vs. 12.5 (group 3) vs. 16.2% (group 4); p = 0.02); whereas, the overall postoperative complications rates at 30- (range: 29–46%) and 90 days (range 21–33%) were similar among the four groups (all p > 0.06). Importantly, no patients in any of the groups required any post-operative blood transfusions related to bleeding events. Our findings confirm safety of GL PVP regarding significant bleeding-associated complications in patients on ATT. However, patients on ongoing ATT should expect longer duration of hematuria, especially after the re-start of their medications. Additionally, they should be counseled on the minor nature of their hematuria, as it does not require any medical or surgical intervention. These data support the use of GL PVP in high-risk ATT patients and open the door for non-interruption of ATT in the perioperative course.
Several investigators have reported on the safety of PVP GL in patients on ongoing ATT. Ruzat and colleagues, within a European cohort, were the first to study this topic. Within their cohort (n = 208), they used the GL XPS 80 Watt system. They stratified their cohort into 4 strata: aspirin vs. Coumadin vs. Clopidogrel vs. control group. No statistically significant differences were recorded for clot retention and blood transfusion. However, hematuria requiring bladder irrigation rates were higher in the Coumadin and Clopidogrel groups [8].
In 2016, the same group of investigators, within a bi-institutional dataset, re-visited the same topic using the GL XPS 180 W system. They showed that GL PVP in patients with ATT is associated with similar rates of postoperative 30-day complications, transfusions and readmissions relative to their counterparts [7]. In this study, patients on aspirin, Clopidogrel and anticoagulation were pooled together. Thus, these favorable complications rates could be diluted by the fact that 52% of their patients population were on aspirin as a single agent. Additionally, adverse events were not graded in a standardized fashion. We were different from the two aforementioned studies, as we have reported our complications rates in more detailed fashion according to the Clavien-Dindo grading system.
Knapp and colleagues have reported on perioperative adverse events in patients on continued anticoagulation using the GL PVP XPS 180 W system. They showed, within their univariate analyses, a non-statistical significant difference in perioperative adverse events between patients on anticoagulation vs. control group [6]. Here, we included multivariable analyses to adjust for potential confounders that can affect bleeding outcomes after surgery: retention status, 5 alpha reductase inhibitors use, prostate volume and age at surgery. In the present study, ATT were discontinued before surgery and resumed within 24 h. We believe that the major drawback of ATT in patients treated with GL PVP is their potential to increase postoperative bleeding events instead of intraoperative complications. In consequence, adverse events profile of patients with short discontinuation and continued ATT are almost similar.
Other surgical laser prostate techniques, including holmium laser enucleation of the prostate (HoLEP) and thulium laser vaporesection (ThuVARP), were adopted in treating patients with symptomatic BPH. In high-risk patients on ATT, HoLEP and ThuVARP showed an acceptable safety profile [14, 15]. However, all these series addressing this high-risk population are non-comparative and had limited sample size (n = 36–83). [14, 15] Thus, PVP GL represents the surgical technic with the highest level of evidence in treating patients on ATT.
Regarding functional outcomes after PVP GL, patients on ATT had similar decrease in IPSS and PSA reduction as well as improvement of uroflowmetry parameters, relative to the control group at 24 months. These findings corroborate previous studies but with median follow-up ranged between 6 and 12 months [7, 8]. Thus, our results represent the strongest evidence on the durability of GL PVP in patients with ATT compared to their counterparts.
Despite its important clinical implications, our study has limitations. First, it is a retrospective design like all the others. It is of note that a randomized trial in the setting of patients on ATT is not feasible because of the potential risk associated with the use of the gold standard TURP. Moreover, loss of follow-up represents another limitation of our study. Finally, all the procedures were performed by a single surgeon with high operative volume beyond the learning curve. This could limit the generalization of these results in the community setting.
In conclusion, GL PVP using the XPS 180 W system is considered safe and effective in treating symptomatic LUTS secondary to BPH in patients with high-risk cardiovascular disease necessitating ATT. However, patients on anticoagulation and antiplatelet medications should expect increased rates of hematuria Clavien 1. These patients have also higher comorbidities and, thus, require a tight collaboration with internal medicine/cardiology consultants. Increased length of hospitalization and post-operative emergency visit should be expected. In consequence, these findings warrant consideration at informed consent, patient counseling and expectation setting.
References
Gratzke C, Bachmann A, Descazeaud A et al (2015) EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 67:1099–1109
McVary KT, Roehrborn CG, Avins AL et al (2011) Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol 185:1793–1803
Thomas JA, Tubaro A, Barber N et al (2016) A multicenter randomized noninferiority trial comparing GreenLight-XPS laser vaporization of the prostate and transurethral resection of the prostate for the treatment of benign prostatic obstruction: two-yr outcomes of the GOLIATH study. Eur Urol 69:94–102
Herrmann TR, Liatsikos EN, Nagele U, Traxer O, Merseburger AS (2012) Guidelines on lasers and technologies. Eur Urol 61(4):783–795
Chung DE, Wysock JS, Lee RK et al (2011) Outcomes and complications after 532 nm laser prostatectomy in anticoagulated patients with benign prostatic hyperplasia. J Urol 186:977–981
Knapp GL, Chalasani V, Woo HH (2017) Perioperative adverse events in patients on continued anticoagulation undergoing photoselective vaporisation of the prostate with the 180-W Greenlight lithium triborate laser. BJU Int 119(Suppl 5):33–38
Lee DJ, Rieken M, Halpern J et al (2016) Laser vaporization of the prostate with the 180-W XPS-Greenlight laser in patients with ongoing platelet aggregation inhibition and oral anticoagulation. Urology 91:167–173
Ruszat R, Wyler S, Forster T et al (2007) Safety and effectiveness of photoselective vaporization of the prostate (PVP) in patients on ongoing oral anticoagulation. Eur Urol 51:1031–1038 (discussion 8–41)
GreenLight XPS for treating benign prostatic hyperplasia: (c) NICE (2016) (2017) GreenLight XPS for treating benign prostatic hyperplasia. BJU Int 119:823–830
Nickel JC, Herschorn S, Corcos J et al (2005) Canadian guidelines for the management of benign prostatic hyperplasia. Can J Urol. 12:2677–2683
Zorn KC, Liberman D (2011) GreenLight 180 W XPS photovaporization of the prostate: how I do it. Can J Urol 18:5918–5926
Valdivieso R, Meyer CP, Hueber PA et al (2016) Assessment of energy density usage during 180 W lithium triborate laser photoselective vaporization of the prostate for benign prostatic hyperplasia. Is there an optimum amount of kilo-Joules per gram of prostate? BJU Int 118:633–640
Mitropoulos D, Artibani W, Graefen M et al (2012) Reporting and grading of complications after urologic surgical procedures: an ad hoc EAU guidelines panel assessment and recommendations. Eur Urol 61:341–349
Macchione L, Mucciardi G, Gali A et al (2013) Efficacy and safety of prostate vaporesection using a 120-W 2-μm continuous-wave Tm:YAG laser (RevoLix 2) in patients on continuous oral anticoagulant or antiplatelet therapy. Int Urol Nephrol 45:1545–1551
Elzayat E, Habibi E, Elhilali M (2006) Holmium laser enucleation of the prostate in patients on anticoagulant therapy or with bleeding disorders. J Urol 175:1428–1432
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meskawi, M., Hueber, PA., Valdivieso, R. et al. Complications and functional outcomes of high-risk patient with cardiovascular disease on antithrombotic medication treated with the 532-nm-laser photo-vaporization Greenlight XPS-180 W for benign prostate hyperplasia. World J Urol 37, 1671–1678 (2019). https://doi.org/10.1007/s00345-018-2560-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2560-8