Abstract
Purpose
This study is a systematic analysis of the evidence regarding oncological, perioperative and postoperative outcomes and the cost of open retropubic radical prostatectomy (ORP), laparoscopic radical prostatectomy (LRP) and robotic-assisted laparoscopic radical prostatectomy (RALP).
Methods
Summary data was abstracted from 104 original research articles representing 227,400 patients. PubMed/Medline, Scopus, Google Scholar, EMBASE and the Cochrane Library were reviewed in December 2016. A total of 104 publications were selected for inclusion. The primary outcomes were positive surgical margin (PSM) and major complication rate according to Clavien classifications. Secondary outcomes were operative time, length of hospital stay, estimated blood loss, transfusions, conversions, rate of post-operative erectile dysfunction and incontinence and total cost of procedure.
Results
ORP had a significantly higher rate than RALP for PSM (OR: 1.18; 95% CI 1.05–1.32; p = 0.004), but the rate of PSM was not significantly different between ORP versus LRP (OR: 1.37; 95% CI 0.88–2.14; p = 0.17) and RALP versus LRP (OR: 0.83; 95% CI 0.40–1.72; p = 0.62). The major Clavien complication rate was significantly different between ORP and RALP (OR: 2.14; 95% CI 1.24–3.68; p = 0.006). Estimated blood loss, transfusions and length of hospital stay were low for RALP, moderate for LRP and high for ORP. The rate of erectile dysfunction (OR: 2.58; 95% CI 1.77–3.75; p < 0.001) and incontinence (OR: 3.57; 95% CI 2.28–5.58; p < 0.001) were significantly lower after RALP than LRP and equivalent for other comparisons. Total cost was highest for RALP, followed by LRP and ORP.
Conclusions
For PSM and peri- and post-operative complications, RALP showed better results than ORP and LRP. In the context of the biases between the studies, one should interpret the results with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the second leading cancer-related cause of death: [1]. For decades, open radical prostatectomy (ORP) has been the reference standard for treatment of localized prostate cancer [2]. More recently, surgical approaches to prostate cancer treatment have been replaced by minimally invasive techniques such as laparoscopic radical prostatectomy (LRP) and robotic-assisted laparoscopic radical prostatectomy (RALP) [3]. Minimally invasive approaches report improved post-operative outcomes with shorter recovery times and hospital stays and provide equivalent functional results [2, 4, 5].
Thus far, no difference in oncological outcomes has been demonstrated between RALP and ORP. Recent meta-analysis concluded that the positive surgical margin (PSM) was similar, regardless of technique [6]. There is an ongoing debate concerning real improvements for minimally invasive surgeries over the open approach because of the additional costs linked with the generalization of these procedures [7]. The present study conducted a systematic literature review to determine the current position of open, laparoscopic and robotic radical prostatectomy.
Methods and materials
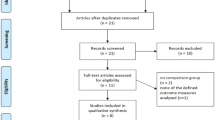
A systematic literature review was performed in December 2016 in multiple databases. The study design, search strategy, data abstraction and excluded studies were determined using Preferred Reporting Items for Systematic Reviews and Meta-analyses criteria (www.prisma-statement.org) (Table 1; Fig. 1). The items retrieved were restricted to publications in English.
Original research articles reporting on primary treatment of localized prostate cancer were included. The reference lists of prostatectomy review/meta-analysis articles that included articles not already in our database was also reviewed [8,9,10,11]. Conference abstracts were not included because they lacked detail and had not undergone rigorous peer review. The level of evidence of the studies included was rated according to criteria by the Center for Evidence-Based Medicine (http://www.cebm.net).
To assess the methodological quality of the studies included, they were initially reviewed by two independent reviewers using total quality assessment (QAS) (Table 1S). Although the QASs were reported for each study, they were not used to weigh the studies in the meta-analysis.
The same authors independently extracted the data, which were later jointly reviewed to reach agreement that the data was accurate. If disagreement existed, it was resolved by consensus or consultation with the senior authors. The data collected from all manuscripts regarding treatment groups included the radical prostatectomy surgical approach (retropubic open, laparoscopic, robotic), type of publication (retrospective, non-randomized trial or randomized trial), publication year (2002–2016; Fig. 1S), duration of follow-up, patient characteristics (number, age, preoperative Gleason score ≥ 8 and clinical stage; Table 2S), primary PSM rates, total intra- and perioperative major Clavien complication rates [12] and secondary outcomes (mean operative time, length of hospital stay, estimated blood loss, blood transfusions, rate of post-operative erectile dysfunction (definition: capability to achieve a spontaneous erection and/or maintain an erection adequate for intercourse after at least 12 month follow-up) and incontinence, conversion to ORP and total cost of procedure; Table 2S).
Statistical methods
Review Manager version 5.2 (downloaded from http://community.cochrane.org/tools/review-production-tools/revman-5) was used to analyze the selected studies. Continuous data for each arm of a particular study were expressed as mean and standard deviation (SD). Dichotomous data was expressed as proportions or risks and the treatment effect was reported as odds ratios (OR) with a 95% confidence interval (95% CI). To use all data, if only median and range were reported in an article, the median was substituted for the mean when the sample size was greater than 25. For range/4 [for moderately sized samples (15 < n ≤ 70)] or range/6 [for large samples (n > 70)], SD was reported as in Hozo et al. [13].
Heterogeneity between studies was assessed using the Chi squared test and I2 statistic. A p value of < 0.1 and an I2 value > 50% were considered suggestive of statistical heterogeneity, prompting a random-effects modeling estimate. A non-significant Chi squared test result (p ≥ 0.1 and I2 ≤ 50%) suggested that there was no evidence of heterogeneity and a random-effect model was used. Funnel plots were constructed for the outcomes to assess publication bias, which is defined as the tendency not to publish studies with a negative result. The more asymmetric the funnel plot was, the higher the potential bias was. Statistical significance was set at p < 0.05.
Results
This systematic review and meta-analysis included 227,400 patients, 86,568 undergoing ORP, 22,177 undergoing LRP and 118,655 undergoing RALP. There were differences in the number of publications over time (p < 0.0001). In particular, a statistically significantly greater proportion of ORP versus LRP studies appeared in early publications (2002–2009; Fig. 1S).
Of the preoperative data, there were significant differences in preoperative clinical stages between studies (ORP: T1 61.1%; T2 34.3%; T3 4.5%, LRP: T1 57.4%; T2 38.7%; T3 3.7% and RALP: T1 71.3%; T2 26.5%; T32.1%, p < 0.0001). There were also significant differences in the percentage of high-grade disease found in preoperative biopsies (Gleason score > 7) in the different surgical approaches (ORP: 13.1%; LRP: 6.4%; RALP: 8.3%; p < 0.001).
In regard to stage by stage comparison of preoperative data, we sub-grouped the clinical stages into two groups as followed: Stage I and II (in which the tumor is limited into the prostate); and stage III and IV (in which the tumor invades to adjusted organs). The results showed significant difference between ORP and RALP in frequencies of Stage I and II (p < 0.001) and Stage III and IV (p < 0.001) between the studies (Fig. 10S). Nevertheless, no significant differences were found between ORP and LRP (stage I and II: p = 0.64 and stage III and IV: p = 0.33) and RALP and LRP (stage I and II: p = 0.34 and stage III and IV: p = 0.30) due to rates of tumor stages.
Open versus robotic-assisted laparoscopic radical prostatectomy
There were significant heterogeneities between studies in PSM (I2 = 78%; p < 0.001), rate of major post-operative Clavien complications (I2 = 78%; p < 0.001), operative time (I2: 100%, p < 0.001), length of hospital stay (I2 = 100%; p < 0.001), estimated blood loss (I2 = 99%; p < 0.001), blood transfusion rate (I2 = 90%; p < 0.001), rate of erectile dysfunction (I2 = 84%; p < 0.001) and incontinency (I2 = 61%; p = 0.002), total cost of procedure (I2 = 100%; p < 0.001). Therefore, random effects were used to analyze these outcomes.
Positive surgical margins were significantly higher in ORP than RALP (OR: 1.18; 95% CI 1.05–1.32; p = 0.004; Fig. 2). Higher significant rate of major post-operative Clavien complications was detected for ORP than RALP (OR: 2.14; 95% CI 1.24–3.68; p = 0.006; Fig. 2S).
In order to compare mean operative time, higher significant operative time was found for RALP than ORP (mean difference: − 44.41 min; 95% CI − 64.79 to − 24.02; p < 0.001; Fig. 3S).
In order to comparison of ORP with RALP, there were longer hospital stays (mean difference: 1.20 day; 95% CI 0.66–1.75; p < 0.001; Fig. 4S), higher blood loss (mean difference: 473.46 ml; 95% CI 424.67–522.24: p < 0.001; Fig. 5S), higher rate of blood transfusion (OR: 6.18; 95% CI 4.37–8.74: p < 0.001; Fig. 6S) and lower total cost of procedure (mean difference: − $4727.36; 95% CI − 6487.89 to − 2926.83; p < 0.001; Fig. 9S) for ORP over RALP.
There was no significant difference between approaches in regard to rates of erectile dysfunction (OR: 1.12; 95% CI 0.75–1.66; p = 0.57; Fig. 7S) and incontinency (OR: 1.20; 95% CI 0.87–1.64; p = 0.26; Fig. 8S).
Considering of design weight in final analysis
The Yaxley study [14] is the only randomized controlled trial comparing open and robotic prostatectomy. This is a well-conducted study which is weighted only 1.6% in the review. We re-analyzed the outcomes due to giving more design weight (approximately 3.8%) to this study. There was a significant different in order to PSM between ORP and RALP (OR: 1.07; 95% CI 0.85–1.12; p = 0.02). Higher significant rate of major post-operative Clavien complications (OR: 1.84; 95% CI −1.34 to 2.54; p = 0.003) for ORP than RALP, longer mean operative time for RALP than ORP (mean difference: − 42.01 min; 95% CI − 54.16 to − 22.12; p < 0.001), longer hospital stays (mean difference: 1.30 day; 95% CI 0.71–1.72; p < 0.001); higher blood loss (mean difference: 443.16 ml; 95% CI 404.01–515.34: p < 0.001) and higher rate of blood transfusion (OR: 5.28; 95% CI 3.91–8.93; p < 0.001) for ORP than RALP.
Open versus laparoscopic radical prostatectomy
Table 2 shows the rate of heterogeneity and meta-analysis of the data. LRP was associated with a longer operative time and hospital stay, lower blood loss and higher rates of blood transfusion. PSM, rate of major complications and post-operative rates of erectile dysfunction and incontinence were comparable between approaches. LRP had a higher total cost than ORP.
Laparoscopic versus robotic-assisted laparoscopic radical prostatectomy
LRP is associated with longer hospital stays, greater blood loss, total cost and post-operative rate of erectile dysfunction and incontinence (Table 2). PSM, rate of major complication, operative time and need for blood transfusions was comparable between approaches. Table 3 lists the results of the meta-analysis of open, robotic and laparoscopic radical prostatectomy over time. The rates of PSM, major complications, erectile dysfunction and incontinence over time are shown in Fig. 3.
Discussion
This study is the largest compilation of comprehensive studies on radical prostatectomy patients to date. It is a systematic review and meta-analysis of this large body of literature. Due to the lack of randomized clinical trials (only one RCT exist [14]), differences in patient characteristics between the surgical cohorts could explain differences in outcomes between treatment groups. These differences cannot be fully corrected by statistical methods. Additionally, unknown differences in the attributes of the patients and physicians and/or the treatments administered could contribute to the highly heterogeneous outcomes between studies. Caution is advised when interpreting the findings of this meta-analysis within the context of the considerations just described. The large number of patients included in the meta-analysis means that the statistically significant results may not necessarily be clinically meaningful.
Traditionally, open radical prostatectomy was the treatment of choice for localized prostate cancer. Over the last two decades, surgical approaches have tended toward endoscopic and minimally invasive surgery such as LRP or RALP. The efficacy and safety of LRP has been questioned because of concerns about its technical difficulty, risk of complications and undefined benefits over open surgery. Previous studies have shown the rate of PSM to be 10–23% for ORP and 9–26% for LRP [14,15,16,17,18,19,20,21]. The results of the current study agree with these results and show no significant difference between ORP and LRP for PSM. Nevertheless, ORP has been associated with higher rates of transfusion and longer catheterization and hospital stays. These results have been confirmed by the results of the current study and of other studies [5, 15, 16, 22, 23].
Rassweiler et al. [5] reported a higher incidence of rectal injury in LRP over ORP (1.8 and 3.2%, respectively) and urinary leakage (0.5 and 2.3%, respectively). An increase in lymphoceles (6.9 and 0%, respectively), wound infection (2.3 and 0.5%, respectively), embolism/pneumonia (2.3 and 0.5%, respectively) and anastomotic strictures (15.9 and 6.4%, respectively) for ORP over LRP. Roumeguere et al. [24] postulated that this difference held true only for minor complications and both approaches experienced similar major complications (5% for ORP and 2.4% for LRP). Recent studies have shown the complication rate to be similar between these surgical methods [18]. This may be the result of the increase in experience and standardization of the approaches.
The previous studies for cohort design indicated several biases related to design. Guazzoni et al. [16] randomized 120, consecutive, age-matched patients into ORP (n = 60) and LRP (n = 60) groups. They showed the operating time was significantly shorter and blood loss and use of analgesia were significantly higher for the ORP group over the LRP group. The overall percentage of post-operative complications and positive margins were comparable. The current results were in agreement with this study.
Post-operative continence and potency are very important aspects, especially for the patient. Comparative studies reported the rate of post-operative continence to be 47–91% in ORP compared to 40–97% in LRP [5, 15, 18, 22, 25]. The potency rate was estimated to be 44–72.4% after ORP and 41–58% after LRP [15, 18].
The cost difference between studies was evaluated by Al-Shaji et al. [26]. They found that LRP costs are slightly lower than those for ORP. This may be because the longer operative time and disposable instrument expenses are offset by the shorter hospital stay, fewer blood transfusions and lower analgesic requirements for the LRP group. A recent study reported a higher total cost for LRP than ORP [27], possibly because of differences in hospital protocol.
Previous studies showed few advantages for LRP over ORP. The factors limiting the performance of LRP are the lack of 3D visualization and loss of freedom of motion using the robot in the laparoscopic approach. Menon et al. [28] showed that RALP is a longer procedure than ORP; however, blood loss is minimal and patients feel less pain and can be discharged from the hospital sooner. These results have been confirmed by other studies [29,30,31,32,33,34,35,36]. Wood et al. [30] found no difference between ORP and RALP for median time to normal activity, 100% activity, and time to driving. The results of the current study are in agreement with their findings.
The PSM has been shown to be 9–39% in RALP and was comparable between groups in most studies [19, 28, 32, 35, 37,38,39,40,41,42,43]. Yaxley et al. [14] conducted a randomized clinical trial with 326 patients who were randomly divided into ORP (n = 151) and RALP (n = 157) groups. Equivalence testing of PSM between groups [15 (10%) in ORP and 23 (15%) in RALP] showed similarity between the two techniques.
In the current study, a comparison of ORP and RALP for PSM showed significant differences, with higher rates for ORP. This result contrasts with that of Tewari et al. [44], who showed that, after propensity adjustment, the only significant differences were lower PSM rates for RALP compared with LRP. This difference may result from the high sample size of studies published after 2013 included in the meta-analysis [14, 45]. The current results are not in agreement with one randomized trial which compared ORP with RALP and showed no significant difference in PSM [14]. This may be because methods of detecting PSM vary depending on the pathologist’s experience and, in some cases, interpretation can be difficult and result in over-diagnosis [46]. It is also accepted that patients with extracapsular extension (pT3) have an increased risk of PSM; however, in RCT, the overall PSM for pT3 tumors was 10%, although the small sample size meant they could not be further analyzed.
Studies show that overall post-operative complications were similar between RALP and ORP [19, 28, 32, 37,38,39,40,41,42]. Krambeck et al. [31] postulated that wound herniation was more common after RALP (1.0% for RALP and none for ORP) and development of bladder neck contracture was more common after ORP. A recent study [47] showed that major complications (Clavien grade III–IV) were less common in the RALP group than in the ORP group (3.4 and 7.6%, respectively). These complications could lead to readmission. The results of the current study were similar and found that major complication rates were significantly higher in ORP over RALP.
Yaxley et al. [14] conducted a randomized clinical trial and showed that urinary function and sexual function scores did not differ significantly between the two methods. The rate of post-operative continence was estimated to be 76–95% [31, 32, 34, 39, 40, 42, 48, 49]. Son et al. [49] showed that of the factors affecting cessation of pad use, only operating method, age and membranous urethral length were significant. The current study found no significant differences in incontinence rates between ORP and RALP. This may be because of differences in patient age between studies, different urethral length retained and the type of questionnaire used to evaluate the post-operative contingencies.
The overall rate of post-operative potency in RALP was reported to be 31–70% [32, 34, 35, 39, 42, 43, 48]. In the results of an inter-subgroup analysis [42], recovery of potency was more rapid in patients who underwent RALP for a small-volume prostate than for those who underwent ORP for a small-volume prostate (3 months: 24 vs. 0%; 6 months: 36 vs 10%). Patients who underwent RALP for a large-volume prostate were less likely to recover continence than those patients who underwent ORP for a large-volume prostate (97 vs. 88%).
RALP is associated with substantially higher operative and total hospital charges in addition to capital expenses incurred by the hospital in acquiring and maintaining the robotic system. The operative charges decreased substantially (27%) once the learning curve had been overcome [50]. In another single-institution analysis, the total actual costs associated with RALP were significantly greater than those for ORP and could be attributed to the robotic equipment and supplies [51].
LRP and RALP are the members of the same family. Studies have demonstrated that extra peritoneal LRP is non-significantly better than RALP in the hands of a skilled laparoscopic urological surgeon with respect to operative time, operative blood loss, hospital stay and length of bladder catheterization [52, 53]. Nevertheless, Hakimi et al. [54] showed significant differences in LRP compared to RALP with regard to operative time, intraoperative blood loss, and length of stay. This can be explained by differences in surgeon experience and limitations in the studies. Porpiglia et al. [55] randomized 120 patients into LRP (n = 60) and RALP (n = 60) groups and showed no differences in terms of perioperative and pathologic results, complication rate, or PSM measurements. The current study found that RALP was associated with lower estimated blood loss and length of hospital stay. This difference may stem from different levels of surgical experience over time. Most studies which compared LRP and RALP found more experience with LRP and less experience with RALP, but that over time, the outcomes were better with RALP. The current study found that over time (Fig. 3), major complication rates decreased with RALP but were steady between 2006 and 2009 and 2014 and 2016.
The continence rate was found to be higher for RALP group at every time point. Continence after 3 months was 80% in the RALP group and 61.6% in the LRP group. After 1 year, the continence rate was 95.0 and 83.3%, respectively. Among preoperative potent patients treated with nerve-sparing techniques, the rate of erection recovery was 80.0 and 54.2%, respectively.
Overall PSM was estimated to be 13–77% [52, 53, 55,56,57] and was comparable between approaches [52, 58, 59]. The current results were in agreement with these studies; however, in a non-randomized study, Magheli et al. [56] found a higher overall PSM rate for the RALP group compared to the LRP group. There was no difference with respect to biochemical recurrence-free survival between groups.
The rates of post-operative continence and potency were comparable between approaches at 82–95% for continence and 56–80% for potency in LRP [53,54,55]; however, analysis showed that incontinence and erectile dysfunction was significantly lower in RALP compared with RLP. These differences could result from factors affecting post-operative continence and potency and the assessment tools used.
After analysis using preoperative data, it is clear that significant differences existed between studies in the preoperative clinical stages. Pathology has changed, evolved over time and this may favor the results of more recent studies, which indicates possible bias in comparison of PSM between studies.
As for PSM, different major Clavien complication rates were found only with comparison of ORP and RALP and not for other comparisons. The complications included in this meta-analysis were abstracted from articles that reported them using a standardized method such as the Clavien classification system [12]; therefore, it is not possible that differential reporting of complications affected the findings. It could also be the reason for the difference in findings compared to other recent meta-analyses [38]. With the increased use of robots in urological surgery, surgeon experience has increased and the expected lower rate of complications in recent studies could weigh the current meta-analysis.
Studies were analyzed for timespan distribution of publications with regard to comparison of the outcomes of the three surgical approaches. The analysis showed that earlier studies favored ORP and more recent studies favored RALP. This could be because of greater surgeon experience with ORP than LRP in earlier studies and, more recently, with RALP.
Centralization of the care of prostate cancer has resulted in better outcomes. This is often not captured in the studies, therefore, the incidence of complications, PSM, continence and erectile dysfunction for different procedures were assessed with regard to the timespan of the publication. Nevertheless, the graphs showed no predictable trend and the incidence of the outcomes did not follow the same pattern. This could result from the use of different questionnaires to evaluate erectile dysfunction and incontinence and the factors that affected the PSM report.
This meta-analysis had the largest sample size of comprehensive studies that compared the three surgical methods for radical prostatectomy in many outcomes. Nevertheless, there were some limitations. The study only included retropubic OP and not studies which evaluated perineal OP. Only English literature was included and only included extraperitoneal LRP studies were examined. Studies which did not determine the mean and SD were estimated from the median and range, which may have slightly differed from the real numbers. The included studies reported different definitions for erectile dysfunction, incontinency and operative time. Therefore, we just analyzed the report of the authors for these outcomes and determining standard definitions for future study are warranted.
Conclusion
Our study showed RALP showed obviously better results than ORP and LRP for PSM and peri- and post-operative complications. Nevertheless, LRP and ORP had comparable outcomes.
In the context of the considerations just described, one should interpret this meta-analysis with caution. The quality of the results of systematic reviews and meta-analyses depend on the quality of the studies included. Sylvester et al. [60] described the ways to resolve discrepancies when findings from RCTs and meta-analyses disagree and showed a correlation between methodological quality and discrepancies in the results of large and small studies included in a meta-analysis. As the quality of the studies included in the current analysis were evaluated by questionnaire, it showed that some studies were not of good quality and also most of the outcomes were not evaluated clinically stage by stage for these three approaches. Therefore, a well-powered study with a good volume of candidate articles is suggested to better evaluate the outcomes of the three surgical approaches especially with the help of International Prostate Cancer Outcomes Registry such as Prostate Cancer Outcomes Registry-Australia and New Zealand (PCOR-ANZ) [61]. Also, to avoid the heterogeneity of future studies to be compared, a standardized international protocol for this type of research could be drafted (by CROES for example) to facilitate the comparison of future similar studies.
References
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T et al (2012) Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin 62(4):220–241
Eggleston JC, Walsh PC (1985) Radical prostatectomy with preservation of sexual function: pathological findings in the first 100 cases. J Urol 134(6):1146–1148
Lein M, Stibane I, Mansour R, Hege C, Roigas J, Wille A et al (2006) Complications, urinary continence, and oncologic outcome of 1000 laparoscopic transperitoneal radical prostatectomies-experience at the Charite Hospital Berlin. Campus Mitte. Eur Urol. 50(6):1278–1282 (discussion 83–4)
Boccon-Gibod L (2006) Radical prostatectomy: open? laparoscopic? robotic? Eur Urol 49(4):598–599
Rassweiler J, Seemann O, Schulze M, Teber D, Hatzinger M, Frede T (2003) Laparoscopic versus open radical prostatectomy: a comparative study at a single institution. J Urol 169(5):1689–1693
Novara G, Ficarra V, Mocellin S, Ahlering TE, Carroll PR, Graefen M et al (2012) Systematic review and meta-analysis of studies reporting oncologic outcome after robot-assisted radical prostatectomy. Eur Urol 62(3):382–404
Kim SP, Boorjian SA, Shah ND, Weight CJ, Tilburt JC, Han LC et al (2013) Disparities in access to hospitals with robotic surgery for patients with prostate cancer undergoing radical prostatectomy. J Urol 189(2):514–520
Ficarra V, Novara G, Artibani W, Cestari A, Galfano A, Graefen M et al (2009) Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol 55(5):1037–1063
Parsons JK, Bennett JL (2008) Outcomes of retropubic, laparoscopic, and robotic-assisted prostatectomy. Urology 72(2):412–416
Ficarra V, Cavalleri S, Novara G, Aragona M, Artibani W (2007) Evidence from robot-assisted laparoscopic radical prostatectomy: a systematic review. Eur Urol 51(1):45–55 (discussion 6)
Artibani W, Ficarra V, Guillonneau BD (2007) Open to debate. The motion: a robot is needed to perform the best nerve sparing prostatectomy. Eur Urol 52(1):275–278
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Yaxley JW, Coughlin GD, Chambers SK, Occhipinti S, Samaratunga H, Zajdlewicz L et al (2016) Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. Lancet 388(10049):1057–1066
Ghavamian R, Knoll A, Boczko J, Melman A (2006) Comparison of operative and functional outcomes of laparoscopic radical prostatectomy and radical retropubic prostatectomy: single surgeon experience. Urology. 67(6):1241–1246
Guazzoni G, Cestari A, Naspro R, Riva M, Centemero A, Zanoni M et al (2006) Intra- and peri-operative outcomes comparing radical retropubic and laparoscopic radical prostatectomy: results from a prospective, randomised, single-surgeon study. Eur Urol 50(1):98–104
Poulakis V, Witzsch U, de Vries R, Dillenburg W, Becht E (2007) Laparoscopic radical prostatectomy in men older than 70 years of age with localized prostate cancer: comparison of morbidity, reconvalescence, and short-term clinical outcomes between younger and older men. Eur Urol 51(5):1341–1348 (discussion 9)
Wagner AA, Link RE, Trock BJ, Sullivan W, Pavlovich CP (2007) Comparison of open and laparoscopic radical prostatectomy outcomes from a surgeon’s early experience. Urology 70(4):667–671
Drouin SJ, Vaessen C, Hupertan V, Comperat E, Misrai V, Haertig A et al (2009) Comparison of mid-term carcinologic control obtained after open, laparoscopic, and robot-assisted radical prostatectomy for localized prostate cancer. World J Urol 27(5):599–605
Dahl DM, Barry MJ, McGovern FJ, Chang Y, Walker-Corkery E, McDougal WS (2009) A prospective study of symptom distress and return to baseline function after open versus laparoscopic radical prostatectomy. J Urol 182(3):956–965
Louie-Johnsun MW, Handmer MM, Calopedos RJ, Chabert C, Cohen RJ, Gianduzzo TR et al (2016) The Australian laparoscopic non robotic radical prostatectomy experience–analysis of 2943 cases (USANZ supplement). BJU Int. 118(Suppl 3):43–48
Artibani W, Grosso G, Novara G, Pecoraro G, Sidoti O, Sarti A et al (2003) Is laparoscopic radical prostatectomy better than traditional retropubic radical prostatectomy? An analysis of peri-operative morbidity in two contemporary series in Italy. Eur Urol 44(4):401–406
Remzi M, Klingler HC, Tinzl MV, Fong YK, Lodde M, Kiss B et al (2005) Morbidity of laparoscopic extraperitoneal versus transperitoneal radical prostatectomy versus open retropubic radical prostatectomy. Eur Urol 48(1):83–89 (discussion 9)
Roumeguere T, Bollens R, Vanden Bossche M, Rochet D, Bialek D, Hoffman P et al (2003) Radical prostatectomy: a prospective comparison of oncological and functional results between open and laparoscopic approaches. World J Urol 20(6):360–366
Greco F, Wagner S, Hoda MR, Kawan F, Inferrera A, Lupo A et al (2010) Laparoscopic vs open retropubic intrafascial nerve-sparing radical prostatectomy: surgical and functional outcomes in 300 patients. BJU Int 106(4):543–547
Al-Shaiji TF, Kanaroglou N, Thom A, Prowse C, Comondore V, Orovan W et al (2010) A cost-analysis comparison of laparoscopic radical prostatectomy versus open radical prostatectomy: the McMaster Institute of Urology experience. Can Urol Assoc J 4(4):237–241
Sugihara T, Yasunaga H, Horiguchi H, Matsui H, Fujimura T, Nishimatsu H et al (2014) Robot-assisted versus other types of radical prostatectomy: population-based safety and cost comparison in Japan, 2012–2013. Cancer Sci 105(11):1421–1426
Menon M, Tewari A, Baize B, Guillonneau B, Vallancien G (2002) Prospective comparison of radical retropubic prostatectomy and robot-assisted anatomic prostatectomy: the Vattikuti Urology Institute experience. Urology 60(5):864–868
Ahlering TE, Woo D, Eichel L, Lee DI, Edwards R, Skarecky DW (2004) Robot-assisted versus open radical prostatectomy: a comparison of one surgeon’s outcomes. Urology 63(5):819–822
Wood DP, Schulte R, Dunn RL, Hollenbeck BK, Saur R, Wolf JS Jr et al (2007) Short-term health outcome differences between robotic and conventional radical prostatectomy. Urology. 70(5):945–949
Krambeck AE, DiMarco DS, Rangel LJ, Bergstralh EJ, Myers RP, Blute ML et al (2009) Radical prostatectomy for prostatic adenocarcinoma: a matched comparison of open retropubic and robot-assisted techniques. BJU Int 103(4):448–453
Rocco B, Matei DV, Melegari S, Ospina JC, Mazzoleni F, Errico G et al (2009) Robotic vs open prostatectomy in a laparoscopically naive centre: a matched-pair analysis. BJU Int. 104(7):991–995
D’Alonzo RC, Gan TJ, Moul JW, Albala DM, Polascik TJ, Robertson CN et al (2009) A retrospective comparison of anesthetic management of robot-assisted laparoscopic radical prostatectomy versus radical retropubic prostatectomy. J Clin Anesth 21(5):322–328
Di Pierro GB, Baumeister P, Stucki P, Beatrice J, Danuser H, Mattei A (2011) A prospective trial comparing consecutive series of open retropubic and robot-assisted laparoscopic radical prostatectomy in a centre with a limited caseload. Eur Urol 59(1):1–6
Philippou P, Waine E, Rowe E (2012) Robot-assisted laparoscopic prostatectomy versus open: comparison of the learning curve of a single surgeon. J Endourol 26(8):1002–1008
Jackson MA, Bellas N, Siegrist T, Haddock P, Staff I, Laudone V et al (2016) Experienced open vs early robotic-assisted laparoscopic radical prostatectomy: a 10-year prospective and retrospective comparison. Urology 91:111–118
Fracalanza S, Ficarra V, Cavalleri S, Galfano A, Novara G, Mangano A et al (2008) Is robotically assisted laparoscopic radical prostatectomy less invasive than retropubic radical prostatectomy? Results from a prospective, unrandomized, comparative study. BJU Int 101(9):1145–1149
Tewari A, Srivasatava A, Menon M (2003) Members of the VIPT. A prospective comparison of radical retropubic and robot-assisted prostatectomy: experience in one institution. BJU Int 92(3):205–210
Nadler RB, Casey JT, Zhao LC, Navai N, Smith ZL, Zhumkhawala A et al (2010) Is the transition from open to robotic prostatectomy fair to your patients? A single-surgeon comparison with 2-year follow-up. J Robot Surg 3(4):201–207
Lo KL, Ng CF, Lam CN, Hou SS, To KF, Yip SK (2010) Short-term outcome of patients with robot-assisted versus open radical prostatectomy: for localised carcinoma of prostate. Hong Kong Med J 16(1):31–35
Doumerc N, Yuen C, Savdie R, Rahman MB, Rasiah KK, Pe Benito R et al (2010) Should experienced open prostatic surgeons convert to robotic surgery? The real learning curve for one surgeon over 3 years. BJU Int. 106(3):378–384
Choo MS, Choi WS, Cho SY, Ku JH, Kim HH, Kwak C (2013) Impact of prostate volume on oncological and functional outcomes after radical prostatectomy: robot-assisted laparoscopic versus open retropubic. Korean J Urol 54(1):15–21
Lott FM, Favorito LA (2015) Is previous experience in laparoscopic necessary to perform robotic radical prostatectomy? A comparative study with robotic and the classic open procedure in patients with prostate cancer. Acta Cir Bras 30(3):229–234
Tewari A, Sooriakumaran P, Bloch DA, Seshadri-Kreaden U, Hebert AE, Wiklund P (2012) Positive surgical margin and perioperative complication rates of primary surgical treatments for prostate cancer: a systematic review and meta-analysis comparing retropubic, laparoscopic, and robotic prostatectomy. Eur Urol 62(1):1–15
Pearce SM, Pariser JJ, Karrison T, Patel SG, Eggener SE (2016) Comparison of perioperative and early oncologic outcomes between open and robotic assisted laparoscopic prostatectomy in a contemporary population based cohort. J Urol 196(1):76–81
Chuang AY, Epstein JI (2008) Positive surgical margins in areas of capsular incision in otherwise organ-confined disease at radical prostatectomy: histologic features and pitfalls. Am J Surg Pathol 32(8):1201–1206
Ryu J, Kwon T, Kyung YS, Hong S, You D, Jeong IG et al (2013) Retropubic versus robot-assisted laparoscopic prostatectomy for prostate cancer: a comparative study of postoperative complications. Korean J Urol 54(11):756–761
Haglind E, Carlsson S, Stranne J, Wallerstedt A, Wilderang U, Thorsteinsdottir T et al (2015) Urinary incontinence and erectile dysfunction after robotic versus open radical prostatectomy: a prospective, controlled, nonrandomised trial. Eur Urol 68(2):216–225
Son SJ, Lee SC, Jeong CW, Jeong SJ, Byun SS, Lee SE (2013) Comparison of continence recovery between robot-assisted laparoscopic prostatectomy and open radical retropubic prostatectomy: a single surgeon experience. Korean J Urol 54(9):598–602
Burgess SV, Atug F, Castle EP, Davis R, Thomas R (2006) Cost analysis of radical retropubic, perineal, and robotic prostatectomy. J Endourol 20(10):827–830
Tomaszewski JJ, Matchett JC, Davies BJ, Jackman SV, Hrebinko RL, Nelson JB (2012) Comparative hospital cost-analysis of open and robotic-assisted radical prostatectomy. Urology 80(1):126–129
Rozet F, Jaffe J, Braud G, Harmon J, Cathelineau X, Barret E et al (2007) A direct comparison of robotic assisted versus pure laparoscopic radical prostatectomy: a single institution experience. J Urol 178(2):478–482
Trabulsi EJ, Zola JC, Gomella LG, Lallas CD (2010) Transition from pure laparoscopic to robotic-assisted radical prostatectomy: a single surgeon institutional evolution. Urol Oncol. 28(1):81–85
Hakimi AA, Blitstein J, Feder M, Shapiro E, Ghavamian R (2009) Direct comparison of surgical and functional outcomes of robotic-assisted versus pure laparoscopic radical prostatectomy: single-surgeon experience. Urology 73(1):119–123
Porpiglia F, Morra I, Lucci Chiarissi M, Manfredi M, Mele F, Grande S et al (2013) Randomised controlled trial comparing laparoscopic and robot-assisted radical prostatectomy. Eur Urol 63(4):606–614
Magheli A, Gonzalgo ML, Su LM, Guzzo TJ, Netto G, Humphreys EB et al (2011) Impact of surgical technique (open vs laparoscopic vs robotic-assisted) on pathological and biochemical outcomes following radical prostatectomy: an analysis using propensity score matching. BJU Int 107(12):1956–1962
Busch J, Gonzalgo ML, Leva N, Ferrari M, Cash H, Kempkensteffen C et al (2015) Matched comparison of robot-assisted, laparoscopic and open radical prostatectomy regarding pathologic and oncologic outcomes in obese patients. World J Urol 33(3):397–402
Asimakopoulos AD, Pereira Fraga CT, Annino F, Pasqualetti P, Calado AA, Mugnier C (2011) Randomized comparison between laparoscopic and robot-assisted nerve-sparing radical prostatectomy. J Sex Med 8(5):1503–1512
Villamil W, Billordo Peres N, Martinez P, Giudice C, Liyo J, Garcia Marchinena P et al (2013) Incidence and location of positive surgical margins following open, pure laparoscopic, and robotic-assisted radical prostatectomy and its relation with neurovascular preservation: a single-institution experience. J Robot Surg 7(1):21–27
Sylvester RJ, Canfield SE, Lam TB, Marconi L, MacLennan S, Yuan Y et al (2016) Conflict of evidence: resolving discrepancies when findings from randomized controlled trials and meta-analyses disagree. Eur Urol 71:811–819
Evans SM, Nag N, Roder D, Brooks A, Millar JL, Moretti KL et al (2016) Development of an international prostate cancer outcomes registry. BJU Int 117(Suppl 4):60–67
Author information
Authors and Affiliations
Contributions
AB: Protocol/project development; data collection or management. JJR: protocol/project development; data collection or management. ST: protocol/project development; data collection or management, manuscript writing/editing. HHW: manuscript writing/editing, data analysis. MPL: manuscript writing/editing, data analysis. HS: protocol/project development; data collection or management, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest existed.
Research involving human participants and/or animals
The data was gathered as systematic review and no human/animal was involved.
Informed consent
The data was gathered as systematic review and no human/animal was involved.
Electronic supplementary material
Below is the link to the electronic supplementary material.
345_2018_2174_MOESM4_ESM.png
Forest plot of included studies which comparing major complication rate in open versus robotic-assisted laparoscopic radical prostatectomy (PNG 24 kb)
345_2018_2174_MOESM5_ESM.png
Forest plot of included studies which comparing operative time in open versus robotic-assisted laparoscopic radical prostatectomy (PNG 43 kb)
345_2018_2174_MOESM6_ESM.png
Forest plot of included studies which comparing length of hospital stay in open versus robotic-assisted laparoscopic radical prostatectomy (PNG 39 kb)
345_2018_2174_MOESM7_ESM.png
Forest plot of included studies which comparing estimated blood loss in open versus robotic-assisted laparoscopic radical prostatectomy (PNG 37 kb)
345_2018_2174_MOESM8_ESM.png
Forest plot of included studies which comparing transfusion rate in open versus robotic-assisted laparoscopic radical prostatectomy (PNG 43 kb)
345_2018_2174_MOESM9_ESM.png
Forest plot of included studies which comparing erectile dysfunction rate in open versus robotic-assisted laparoscopic radical prostatectomy (PNG 20 kb)
345_2018_2174_MOESM10_ESM.png
Forest plot of included studies which comparing incontinency rate in open versus robotic-assisted laparoscopic radical prostatectomy (PNG 22 kb)
345_2018_2174_MOESM11_ESM.png
Forest plot of included studies which comparing total cost in open versus robotic-assisted laparoscopic radical prostatectomy (PNG 16 kb)
Rights and permissions
About this article
Cite this article
Basiri, A., de la Rosette, J.J., Tabatabaei, S. et al. Comparison of retropubic, laparoscopic and robotic radical prostatectomy: who is the winner?. World J Urol 36, 609–621 (2018). https://doi.org/10.1007/s00345-018-2174-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2174-1