Abstract
Purpose
To analyze the impact of urinary diversion type following radical cystectomy (RC) on readmission and short-term mortality rates.
Methods
Patients who underwent RC for bladder cancer in the National Cancer Data Base were grouped based on the type of urinary diversion performed: non-continent [ileal conduit (IC)] or two continent techniques [continent pouch (CP) and orthotopic neobladder (NB)]. We used propensity score matching and multivariable logistic regression models to compare 30-day readmission and 30- and 90-day mortality between the different types of urinary diversion.
Results
Among 11,933 patients who underwent RC, we identified 10,197 (85.5%) IC, 1044 (8.7%) CP, and 692 (5.8%) NB. Patients who received IC were significantly older and had more comorbidities (p < 0.0001). Continent diversions were more likely to be performed at an academic center (p < 0.0001). Surgery performed at a non-academic center was an independent predictor of 30-day readmission (OR 1.19, p = 0.010) and 30-day mortality (OR 1.27, p = 0.043). Patients undergoing NB had an increased likelihood of being readmitted (OR 1.41, p = 0.010). There was no significant difference in short-term mortality between groups.
Conclusions
Patients undergoing NB had marginally increased rates of readmission compared to IC. Surgery performed at a non-academic center was associated with higher readmission and 30-day mortality. Similar short-term mortality rates were observed among the different types of urinary diversion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical cystectomy (RC) remains the gold-standard treatment approach for muscle-invasive bladder cancer [1]. It is well known that RC is a complex and morbid procedure, primarily due to the urinary reconstruction required after removal of the bladder [2]. Although several techniques of urinary diversion have been described, there are basically 3 types of reconstruction: non-continent diversion [ileal conduit (IC)] and two continent techniques [continent pouch (CP) and orthotopic neobladder (NB)]. Choosing the optimal diversion type can be challenging and depends on clinical parameters, as well as the potential morbidity related to each approach.
Since its creation in the 1940s, IC has been the most common type of urinary diversion [3] presumably because of its surgical simplicity and decreased rate of complications compared to CP and NB. However, given improvements in surgical technique and postoperative care [4], continent diversions have gained popularity [5, 6]. Several studies have shown that urinary diversions are associated with significant complication rates [7,8,9]. However, limited data are available comparing different types of urinary diversion and postoperative outcomes [10,11,12].
We analyzed the National Cancer Data Base (NCDB) and compared 30-day readmission rates, as well as 30- and 90-day mortality rates between different types of urinary diversion among patients undergoing RC.
Materials and methods
The National Cancer Data Base is an oncology registry in the USA that compiles approximately 70% of all national cancer cases each year, receiving cases from over 1400 healthcare centers. For quality assurance purposes, cases that do not meet standardized requirements are returned to their respective facilities. Data on patient socio-demographics, tumor characteristics, staging details, surgical and adjuvant treatments, and outcomes are all reported, while simultaneously ensuring both hospital and patient anonymity [13].
Using NCDB registry data from 2004 to 2013, we identified 439,188 patients who were diagnosed with bladder cancer. We selected patients who underwent RC for primary bladder cancer (n = 41,060). We also excluded patients diagnosed at death or autopsy (n = 11), with missing/unknown (X or 88) clinical TNM stage (n = 18,310), or with missing/unknown type of urinary diversion (n = 9451). The final cohort was limited to patients with known 30- and 90-day mortality and unplanned readmission data within 30 days of hospital discharge, resulting in 11,933 patients for analysis.
The primary outcome of the study was unplanned hospital readmission within 30 days. Secondary outcomes of the study were 30- and 90-day mortality. All outcome measurements were binary variables. Mortality was defined as whether the patient died within a given number of days after undergoing RC for primary bladder cancer. All outcomes were considered to be complications from RC. Urinary diversion type was considered as the primary predictive variable, and patients were grouped according to three types of urinary diversion: IC (Code 61), CP (Codes 62 and 63), or NB (Code 64).
Socio-demographic variables included age at diagnosis (years), sex, and race (white, black, other/unknown). Clinical variables included AJCC clinical T stage (T1–T4, Ta, or Tis), histology (papillary transitional cell carcinoma, squamous cell carcinoma, micropapillary transitional cell carcinoma), and facility type. We split facility type in 2 groups (academic and non-academic) according to the NCDB definition. Facilities with a residency program and more than 500 cancer cases diagnosed yearly were included in the academic group. All others were defined as non-academic. Comorbidity status was categorized according to the Charlson–Deyo Score and further stratified into yes (score of ≥ 1) or no (score of 0).
Patient characteristics (age, sex, race), tumor characteristics such as AJCC tumor stage, and facility type were summarized using descriptive statistics for overall sample as well as by type of urinary diversion. Frequencies and percentages were obtained for categorical variables, while mean, standard deviation, and median with 25th and 75th percentiles were used for continuous variables.
Univariate and multivariable logistic regression models were fitted to each complication outcome. These models included type of diversion (IC, CP, or NB) as the primary predictor variable, where IC was considered the reference group in regression models. Age in years, sex, race, comorbidity, academic program, AJCC clinical T, and histology were also included in the models as co-variables to adjust for differences in patient socio-demographic and clinical characteristics. This allowed for identification of whether diversion type was considered as a risk factor for the likelihood of each complication outcome. Crude and adjusted odds ratios (OR) and 95% confidence intervals (95% CI) were calculated.
We identified possible confounding by indication, where patients with worse clinical and pathological characteristics were more likely to be allocated to the IC group. Propensity score matching was performed for mortality analysis in order to control for residual confounding factors after multivariable analysis. IC and NB patients were matched 1:1 by calculating propensity scores for each patient based upon age, race, gender, AJCC clinical stage, facility type, histology, and comorbidity.
All statistical analyses were performed using SAS version 9.4 statistical software for Windows (SAS Institute Inc., Cary, NC, USA).
Results
Demographic and clinical characteristics by urinary diversion type are shown in Table 1. Among 439,188 patients who were diagnosed with bladder cancer, a total of 11,933 patients met study inclusion criteria. IC (85.5%) was the most frequently performed procedure, followed by CP (8.7%) and NB (5.8%). The majority of patients were male (87.4%), white (90.6%), without comorbidity (68.7%), treated at an academic center (56.2%), and on average 68 years old. Patients who received IC were significantly older on average (69 years) than those who underwent CP (61 years) or NB (63 years) (p < 0.0001). Patients with IC (33%) were more likely to have at least one comorbidity compared to CP (21.7%) or NB (21%) patients (p < 0.0001). CP (66.7%) and NB (80.6%) were more likely to be performed at an academic center than IC (53.5%) (p < 0.0001). Furthermore, patients undergoing IC (19.3%) were more likely to present at an advanced stage (AJCC clinical stage > T3) compared to CP (16.4%) and NB (13.3%) (p < 0.0001). There were no statistically significant differences in race, histology, and length of stay among urinary diversion types.
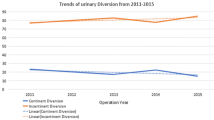
As displayed in Table 2, overall unplanned readmission within 30 days was 8.3%. NB (10.3%) had the highest rate, followed by CP (9.1%) and IC (8.1%). Analysis of 30-day mortality revealed that IC (2.7%) patients had higher rates of mortality than CP (1.9%) or NB (1.0%). Mortality within 90 days was also higher for IC (7.1%) compared to CP (4.8%) or NB (1.9%).
Table 3 shows univariate and multivariable logistic regression analysis for each study outcome. In univariate analysis, patients undergoing NB (OR 1.30, 95% CI 1.01–1.68, p = 0.044) had an increased likelihood of unplanned readmission within 30 days compared to IC. This relationship was also valid in multivariable analysis (NB: OR 1.41, 95% CI 1.09–1.84, p = 0.010). We also saw a trend toward a higher readmission rate for CP; however, it was not statistically significant. Furthermore, patients undergoing any type of urinary diversion at a non-academic center had an increased likelihood of being readmitted within 30 days compared to surgery performed at an academic center (OR 1.19; 95% CI 1.04–1.36, p = 0.010).
In univariate analysis, NB patients (OR 0.40, 95% CI 0.19–1.83, p = 0.014) had a lower likelihood of 30-day mortality than IC patients, but this association was not statistically significant in multivariable analysis. Performing surgery at a non-academic center was independently associated with 30-day mortality (OR 1.27 1.01–1.60, p < 0.043). While a similar trend was observed for 90-day mortality, it was not statistically significant. After adjusting for other factors in multivariable analysis, age (OR 1.06, 95% CI 1.05–1.06, p < 0.001) and comorbidity (OR 1.60, 95% CI 1.38–1.86, p = 0.001) were significantly associated with 90-day mortality. Although there was a decreased likelihood of dying within 90 days for patients undergoing CP (OR 0.67, 95% CI 0.50–0.89, p = 0.007) and NB (OR 0.26, 95% CI 0.15–0.45, p < 0.001) compared to IC in the univariate model, this relationship was true only for NB patients (OR 0.47, 95% CI 0.27–0.81, p < 0.007) in multivariable analysis.
A 1:1 propensity score matching for patients undergoing IC and NB was performed to control for confounding factors, and mortality analysis was repeated. No patients were excluded, leaving a final cohort of 692 patients in each group in this analysis. There was no statistically significant difference in 90-day mortality between IC and NB patients (Table 4).
Discussion
Patient selection is crucial when choosing the appropriate urinary diversion following RC. Clinical characteristics such as performance status and comorbidities are important considerations for optimizing surgical outcomes and decreasing complication rates [14]. It is important for physicians to be aware of risks associated with each type of urinary diversion before deciding which technique is most appropriate.
Our study demonstrates an unplanned readmission rate within 30 days after RC of 8.3%, which is lower than other published series [15,16,17,18,19,20]. We speculate that there are many possible explanations for this finding. First, the relatively low median age of the cohort (69 years) and low incidence of comorbidities (31%) might have positively impacted readmission rates. Secondly, the fact that 56% of centers performing RC were academic may also have contributed to this finding. Furthermore, 67% of CP and 81% of NB, which are more complex procedures, were performed at academic centers. An unexpected finding was that among all urinary diversions performed, less than 6% were NB. This is even more surprising if we take into consideration the fact that most procedures were performed at academic institutions, 76% of patients presented with clinical stage 1 or 2 disease, and almost 70% of patients had no reported comorbidities. When RC with urinary diversion was performed at a non-academic program, there was a 19% increase in the odds of having an unplanned readmission within 30 days compared to an academic center (OR 1.19, p = 0.010). Additionally, the risk of dying within 30 days increased by 27% when surgery was performed outside of an academic setting (OR 1.27, p < 0.043). These findings are in agreement with previous studies, which have shown that increased surgical volume is associated with a decreased risk of perioperative complications [21, 22].
Loew et al. [23] showed that surgeons with the highest volume (> 28 cases per year) had not only lower odds of major complications, but also lower direct hospital costs compared to surgeons with the lowest volumes. The authors also reported that among the 49,540 patients included in their cohort, almost 70% had surgery performed by a surgeon with less than 3 cases per year. While selecting the appropriate urinary diversion is crucial for patients, our analysis suggests that choosing an appropriate institution may be even more important. Therefore, centralization of care to hospitals with a high volume of cystectomies may reduce the risk of complications and overall cost.
Several other variables may also influence perioperative outcomes such as age, comorbidity, gender, stage, grade, histology type, and use of perioperative chemotherapy. Our main finding indicated that, after controlling for these factors, type of urinary diversion was an independent predictor of unplanned readmission within 30 days. Patients who underwent NB had a significantly higher probability of being readmitted within 30 days (OR 1.41, p = 0.010) compared to the IC group. This finding supports our hypothesis that the higher complexity of NB diversion would be associated with higher complication rates, and consequently higher readmission rates.
Few studies have compared perioperative outcomes between the three most common types of urinary diversion. Monn et al. [11] showed similar readmission rates between IC, NB, and Indiana Pouch (12 vs 11 vs 13%, p = 0.999); however, there were few patients in the NB and Indiana Pouch groups (55 and 39, respectively). Furthermore, nearly half of the patients in the IC group had more locally advanced disease (pathologic stage T3 and T4) compared to a significantly lower incidence of advanced stage disease in the NB and Indiana Pouch groups (45 vs 20 vs 31%, p < 0.001). Antonelli et al. [10] compared IC to NB in a matched cohort of 85 patients and showed no difference in postoperative complication rates using the Clavien–Dindo classification. Similarly, Kim et al. [12] showed no difference with respect to early or late complications between IC and NB. While these studies reported outcomes from single institutions with small sample sizes, our data originate from a large national registry that collects information on approximately 70% of all newly diagnosed cases of cancer in the USA. Results from our study may therefore be more generalizable to contemporary clinical practice.
The overall mortality rate within 30 and 90 days from the date of surgery was 2.5 and 6.6%, respectively. The finding that increased age and comorbidity status were predictors of 90-day mortality is not surprising. Age has been shown to be associated with postoperative outcomes [24, 25]. Previous studies have shown that perioperative mortality in octogenarians can be as high as 14% [26, 27]. Interestingly, our data indicate that more than 90% of patients who died were in the IC group. This finding was most likely due to confounding by indication, since surgeons may choose to perform IC instead of other diversion types for patients with less favorable clinical and pathological characteristics. In fact, patients undergoing IC were older, had more comorbidities, and presented with more advanced disease. To address this issue, we performed multivariable analysis controlling for these variables. Interestingly, patients undergoing NB were less likely to die within 90 days compared to IC even in the multivariable analysis. We therefore performed propensity score matching and found no difference in short-term mortality between patients undergoing NB and IC.
This study has limitations related to the nature of the NCDB. First, there is concern for under-reporting of readmission rates by academic centers, since patients might be admitted to non-index hospitals not covered by the NCDB. Secondly, no information is provided regarding postoperative quality of life, which is often believed to be an advantage for any continent diversion. However, data in the literature comparing long-term quality of life between types of diversion are conflicting. Furthermore, there are no data available related to complications or specific comorbidities, which can have an impact on perioperative outcomes. Finally, a weakness of retrospective studies is that confounding factors may impact study outcomes. However, we also performed propensity score matching, which has been shown to be a more robust tool to control for imbalances between covariates [28].
Conclusion
Selecting the most appropriate urinary diversion for patients undergoing RC, as well as facility type is important for maximizing quality of life and minimizing perioperative complications. Readmission rates within 30 days are marginally higher for NB compared to IC. However, the type of urinary diversion does not impact short-term mortality. Furthermore, surgery performed at a non-academic center was an independent predictor of readmission. Patients and physicians should be informed about these factors when deciding on the best surgical management for bladder cancer.
References
Witjes JA, Comperat E, Cowan NC, De Santis M, Gakis G, Lebret T, Ribal MJ, Van der Heijden AG, Sherif A (2014) EAU guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2013 guidelines. Eur Urol 65(4):778–792. https://doi.org/10.1016/j.eururo.2013.11.046
Malavaud B, Vaessen C, Mouzin M, Rischmann P, Sarramon J, Schulman C (2001) Complications for radical cystectomy. Impact of the American Society of Anesthesiologists score. Eur Urol 39(1):79–84. https://doi.org/10.1159/000052416
Gore JL, Saigal CS, Hanley JM, Schonlau M, Litwin MS (2006) Variations in reconstruction after radical cystectomy. Cancer 107(4):729–737. https://doi.org/10.1002/cncr.22058
Collins JW, Patel H, Adding C, Annerstedt M, Dasgupta P, Khan SM, Artibani W, Gaston R, Piechaud T, Catto JW, Koupparis A, Rowe E, Perry M, Issa R, McGrath J, Kelly J, Schumacher M, Wijburg C, Canda AE, Balbay MD, Decaestecker K, Schwentner C, Stenzl A, Edeling S, Pokupic S, Stockle M, Siemer S, Sanchez-Salas R, Cathelineau X, Weston R, Johnson M, D’Hondt F, Mottrie A, Hosseini A, Wiklund PN (2016) Enhanced recovery after robot-assisted radical cystectomy: EAU robotic urology section scientific working group consensus view. Eur Urol. https://doi.org/10.1016/j.eururo.2016.05.020
Hautmann RE, de Petriconi RC, Volkmer BG (2011) 25 years of experience with 1,000 neobladders: long-term complications. J Urol 185(6):2207–2212. https://doi.org/10.1016/j.juro.2011.02.006
Parekh DJ, Donat SM (2007) Urinary diversion: options, patient selection, and outcomes. Semin Oncol 34(2):98–109. https://doi.org/10.1053/j.seminoncol.2006.12.010
Sogni F, Brausi M, Frea B, Martinengo C, Faggiano F, Tizzani A, Gontero P (2008) Morbidity and quality of life in elderly patients receiving ileal conduit or orthotopic neobladder after radical cystectomy for invasive bladder cancer. Urology 71(5):919–923. https://doi.org/10.1016/j.urology.2007.11.125
Porter MP, Penson DF (2005) Health related quality of life after radical cystectomy and urinary diversion for bladder cancer: a systematic review and critical analysis of the literature. J Urol 173(4):1318–1322. https://doi.org/10.1097/01.ju.0000149080.82697.65
Ali AS, Hayes MC, Birch B, Dudderidge T, Somani BK (2015) Health related quality of life (HRQoL) after cystectomy: comparison between orthotopic neobladder and ileal conduit diversion. Eur J Surg Oncol 41(3):295–299. https://doi.org/10.1016/j.ejso.2014.05.006
Antonelli A, Belotti S, Cristinelli L, De Luca V, Simeone C (2015) Comparison of perioperative morbidity of radical cystectomy with neobladder versus ileal conduit: a matched pair analysis of 170 patients. Clin Genitour Cancer. https://doi.org/10.1016/j.clgc.2015.07.011
Monn MF, Kaimakliotis HZ, Cary KC, Pedrosa JA, Flack CK, Koch MO, Bihrle R (2014) Short-term morbidity and mortality of Indiana pouch, ileal conduit, and neobladder urinary diversion following radical cystectomy. Urol Oncol 32(8):1151–1157. https://doi.org/10.1016/j.urolonc.2014.04.009
Kim SH, Yu A, Jung JH, Lee YJ, Lee ES (2014) Incidence and risk factors of 30-day early and 90-day late morbidity and mortality of radical cystectomy during a 13-year follow-up: a comparative propensity-score matched analysis of complications between neobladder and ileal conduit. Jpn J Clin Oncol 44(7):677–685. https://doi.org/10.1093/jjco/hyu051
Bilimoria KY, Stewart AK, Winchester DP, Ko CY (2008) The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol 15(3):683–690. https://doi.org/10.1245/s10434-007-9747-3
Shimko MS, Tollefson MK, Umbreit EC, Farmer SA, Blute ML, Frank I (2011) Long-term complications of conduit urinary diversion. J Urol 185(2):562–567. https://doi.org/10.1016/j.juro.2010.09.096
Minnillo BJ, Maurice MJ, Schiltz N, Pillai AC, Koroukian SM, Daneshgari F, Kim SP, Abouassaly R (2015) Few modifiable factors predict readmission following radical cystectomy. Can Urol Assoc J 9(7–8):E439–E446. https://doi.org/10.5489/cuaj.2793
Aghazadeh MA, Barocas DA, Salem S, Clark PE, Cookson MS, Davis R, Gregg J, Stimson CJ, Smith JA Jr, Chang SS (2011) Determining factors for hospital discharge status after radical cystectomy in a large contemporary cohort. J Urol 185(1):85–89. https://doi.org/10.1016/j.juro.2010.08.016
Moschini M, Gandaglia G, Dell’Oglio P, Fossati N, Cucchiara V, Burgio G, Mattei A, Damiano R, Shariat SF, Salonia A, Montorsi F, Briganti A, Colombo R, Gallina A (2015) Incidence and predictors of 30-day readmission in patients treated with radical cystectomy: a single center european experience. Clin Genitour Cancer. https://doi.org/10.1016/j.clgc.2015.12.017
Stimson CJ, Chang SS, Barocas DA, Humphrey JE, Patel SG, Clark PE, Smith JA Jr, Cookson MS (2010) Early and late perioperative outcomes following radical cystectomy: 90-day readmissions, morbidity and mortality in a contemporary series. J Urol 184(4):1296–1300. https://doi.org/10.1016/j.juro.2010.06.007
Hu M, Jacobs BL, Montgomery JS, He C, Ye J, Zhang Y, Brathwaite J, Morgan TM, Hafez KS, Weizer AZ, Gilbert SM, Lee CT, Lavieri MS, Helm JE, Hollenbeck BK, Skolarus TA (2014) Sharpening the focus on causes and timing of readmission after radical cystectomy for bladder cancer. Cancer 120(9):1409–1416. https://doi.org/10.1002/cncr.28586
Schmid M, Chiang HA, Sood A, Campbell L, Chun FK, Dalela D, Okwara J, Sammon JD, Kibel AS, Menon M, Fisch M, Trinh QD (2016) Causes of hospital readmissions after urologic cancer surgery. Urol Oncol 34(5):236.e211–236.e231. https://doi.org/10.1016/j.urolonc.2015.11.019
Nielsen ME, Mallin K, Weaver MA, Palis B, Stewart A, Winchester DP, Milowsky MI (2014) Association of hospital volume with conditional 90-day mortality after cystectomy: an analysis of the National Cancer Data Base. BJU Int 114(1):46–55. https://doi.org/10.1111/bju.12566
Porter MP, Gore JL, Wright JL (2011) Hospital volume and 90-day mortality risk after radical cystectomy: a population-based cohort study. World J Urol 29(1):73–77. https://doi.org/10.1007/s00345-010-0626-3
Leow JJ, Reese S, Trinh QD, Bellmunt J, Chung BI, Kibel AS, Chang SL (2015) Impact of surgeon volume on the morbidity and costs of radical cystectomy in the USA: a contemporary population-based analysis. BJU Int 115(5):713–721. https://doi.org/10.1111/bju.12749
Prout GR Jr, Wesley MN, Yancik R, Ries LA, Havlik RJ, Edwards BK (2005) Age and comorbidity impact surgical therapy in older bladder carcinoma patients: a population-based study. Cancer 104(8):1638–1647. https://doi.org/10.1002/cncr.21354
Nielsen ME, Shariat SF, Karakiewicz PI, Lotan Y, Rogers CG, Amiel GE, Bastian PJ, Vazina A, Gupta A, Lerner SP, Sagalowsky AI, Schoenberg MP, Palapattu GS (2007) Advanced age is associated with poorer bladder cancer-specific survival in patients treated with radical cystectomy. Eur Urol 51(3):699–706. https://doi.org/10.1016/j.eururo.2006.11.004 (discussion 706–698)
Izquierdo L, Peri L, Leon P, Ramirez-Backhaus M, Manning T, Alcaraz A, Roupret M, Solsona E, Rubio J, Sengupta S, Chan Y, Liodakis P, Gyomber D, Bolton D, Lawrentschuk N (2015) The role of cystectomy in elderly patients—a multicentre analysis. BJU Int 116(Suppl 3):73–79. https://doi.org/10.1111/bju.13227
Comploj E, West J, Mian M, Kluth LA, Karl A, Dechet C, Shariat SF, Stief CG, Trenti E, Palermo S, Lodde M, Horninger W, Madersbacher S, Pycha A (2015) Comparison of complications from radical cystectomy between old-old versus oldest-old patients. Urol Int 94(1):25–30. https://doi.org/10.1159/000358731
Roobol MJ, Heijnsdijk EA (2011) Propensity score matching, competing risk analysis, and a competing risk nomogram: some guidance for urologists may be in place. Eur Urol 60(5):931–933. https://doi.org/10.1016/j.eururo.2011.07.039 (discussion 933–934)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nahar, B., Koru-Sengul, T., Miao, F. et al. Comparison of readmission and short-term mortality rates between different types of urinary diversion in patients undergoing radical cystectomy. World J Urol 36, 393–399 (2018). https://doi.org/10.1007/s00345-017-2140-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-017-2140-3