Abstract
Purpose
To evaluate the stone-free rates (SFRs) and stone clearance rates (SCRs) of extracorporeal shock-wave lithotripsy (SWL), retrograde intrarenal surgery (RIRS), and percutaneous nephrolitholapaxy (PCNL) according to non-contrast computer tomography (NCCT) findings.
Methods
Original articles were identified from PubMed. After exclusion of ineligible papers, twenty-three studies with 2494 cases were included in the review.
Results
Six SWL, five RIRS and eight PCNL studies were selected. Additionally, four comparative articles were identified. SWL presents SFRs ranging 35–61.3 % and SCRs for residuals <4 mm being 43.2–92.9 %. RIRS studies report SFRs of 34.8–59.7 % and SCRs for residuals <4 mm ranging 48–96.7 %. Finally, PCNL presents SFRs of 20.8–100 % and SCRs for residuals <4 mm being 41.5–91.4 %. According to the comparative studies, SFRs are 17–61.3 % for SWL, 50 % for RIRS, and 95–100 % for PCNL.
Conclusions
According to NCCT findings, it seems that PCNL provides better SFRs than ESWL and RIRS. However, further research with comparable and complete preoperative parameters and outcomes could reduce the heterogeneity of current data.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
SWL, RIRS, and PCNL are the standard options for active treatment of nephrolithiasis. According to the European Association of Urology guidelines, all three modalities can be used selectively depending on stone size and location [1].
Successful active stone treatment is mainly defined either by the complete absence of residual stones or by the presence of clinically insignificant residual fragments. SFRs and SCRs quantify the above states, respectively. At the same time, the treatment should be characterized by minimal hospitalization and complication rates (CRs). By definition, SWL offers an outpatient, noninvasive, treatment with the drawback of limited SFRs, often requiring further treatment [2]. A recent meta-analysis by De et al. [3] corroborates the high SFRs but also the higher CRs and longer hospital stay reported for PCNL. Finally, RIRS has been also greatly evolving, being utilized in the management of even larger or multiple renal stones throughout the entire pelvicalyceal system [4, 5]. The main drawbacks of retrograde access include a potential violation of the ureter [6], as well as the limited visualization [7].
There has been a great scientific effort to elucidate the SFRs and SCRs of the different techniques and implement the correct indications for treating different types of stones according to stone size and localization. Undeniably, NCCT is the most sensitive diagnostic tool, for detecting residual fragments as it offers higher sensitivity regardless of stone size, compared to plain kidney–ureter–bladder X-ray and ultrasonography [8–14]. Additionally, NCCT has a higher capability of predicting occurrence of stone-related events [15]. Different NCCT modalities include regular-dose NCCT and low-dose NCCT, which reduces the radiation risk by offering a sensitivity of 96.6 % and specificity of 94.9 % [16, 17]. At the same time, accuracy of stone detection increases by decreasing the NCCT slice thickness, which nowadays can be as low as 0.625 mm [18, 19]. Yet, most of the studies have not utilized NCCT during in their postoperative follow-up. The aim of this review is to compare the SFRs and SCRs of the three modalities according to NCCT findings.
Materials and methods
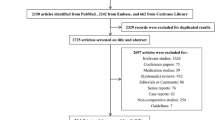
Literature search and article selection (fig)
A systematic literature review was performed up to November 2015 using PubMed in order to identify relevant original studies (“Appendix 1, 2”). Different keywords included “extracorporeal shock wave lithotripsy,” “retrograde intrarenal surgery,” “RIRS,” “flexible ureteroscopy,” “percutaneous nephrolithotomy,” “mini PCNL,” “micro PCNL.” Six hundred and twenty six records were identified through database searching. After duplicates were removed, 465 records remained. After record screening, 136 records, which were not written in English or were in vitro and pediatric studies, were excluded. From the 330 full-text articles assessed, complex lithiasis studies, papers not reporting SCRs and SFRs and studies that did not use NCCT in their follow-up, or did not define the method used, were also excluded. Cited references from the selected articles retrieved in the search were also assessed for significant papers. Two independent reviewers (TT, MH) performed the literature search, and twenty-three studies were judged as eligible by their consensus. The quality of the studies was graded according to the Grading of Recommendations, Assessment, Development, and Evaluation system [20]. Levels of evidence (LEs) and grade of guideline recommendations were rated in accordance with the European Association of Urology guidelines [1].
Data extraction
Two independent reviewers (TT, MH) extracted the data of the selected studies. More specifically, six SWL studies (Table 1), five RIRS studies (Table 2), eight PCNL studies (Table 3), and four comparative studies (Tables 1–3) were reviewed. The data reviewed from the different studies included the number of procedures, number of stones (mean, range), the stone size and location (mean, range), the duration of the procedures (mean, range), the slice thickness of CT images (collimation), the CT quality parameters (in mA and kV), the timing of post-treatment CT performance, and the stone size thresholds used to name residuals as clinically insignificant. The CRs, duration of hospitalization, and need for ancillary procedures were also recorded. The primary endpoint of the review is the SFRs and SCRs of the different procedures (Fig. 1).
Outcomes
SWL outcomes (Table 1)
A total of 10 studies with 933 cases were identified [2, 21–29]. Six of them were descriptive non-comparative studies (LE 4) [21–26], one was a cohort study (LE 3) [2], and three were randomized controlled trials (LE 2) [27–29]. The range of maximal stone diameter was 5–25 mm. The NCCTs were mainly performed at 3 months [2, 21, 22, 24–29]. The SFRs reported were 35–61.3 % [21, 23, 24, 27–29] and the SCRs with residual stone size ≤4 mm 43.2–92.9 % [2, 22–26, 28]. The rates for further treatment need ranged 16–67.7 % [2, 21, 23, 27–29].
RIRS outcomes (Table 2)
Overall, a total of seven RIRS studies with 563 cases were selected as eligible [2, 28, 30–34]. Five of them were descriptive non-comparative studies (LE 4) [30–34], one was a cohort study (LE 3) [2], and one was a randomized controlled trial (LE 2) [28]. The stone size range was 5–50 mm. The NCCTs were mainly performed 1–3 months postoperatively [2, 28, 30–32, 34], except in the study by Takazawa in which they were performed earlier than 2 weeks after the procedures [33]. The SFRs reported were 34.8–59.7 % [28, 30, 31, 34]. In particular, for stones with diameter greater than 2 cm, the SFRs were 59.7 % [34]. The SCRs for residual stone size ≤4 mm were 48–96.7 % [2, 28, 30–33]. The need for further active treatment was presented in four studies and was 3.7–35 % [2, 28, 30, 33].
PCNL outcomes (Table 3)
Eight PCNL single-arm (LE: 4) studies [9, 11, 12, 14, 35–38], one cohort study (LE 3) [2], and two randomized controlled trials (LE 2) with a total of 998 cases were selected in this review. The stone size could not be clearly assessed. In all studies, procedures were performed with standard PCNL instruments. Interestingly, most NCCTs were performed mainly either direct postoperatively [35] or during the first two postoperative weeks [9, 12, 14, 36–38]. Nevertheless, the three comparative [2, 27, 29] and two single-arm studies [11, 37] reported outcomes after 1–12 months. The SFRs reported are 20.8–100 % [9, 11, 12, 14, 27, 29, 36, 37]. The SCRs for residual stone size ≤4 mm were 41.5–91.4 % [2, 9, 11, 14, 35, 37, 38]. The necessity for ancillary procedures reported was 0.00–30.18 % [2, 9, 11, 12, 14, 27, 29, 37].
Discussion
Selecting the optimal renal stone treatment can be challenging, as each technique is characterized by unique benefits and drawbacks. Furthermore, the absence of high-quality comparative trials or reviews and meta-analyses comparing the three modalities is more than apparent. Only recently, a meta-analysis by De et al. [3] compared RIRS with PCNL and minimally invasive PCNL (MIP). The authors concluded that PCNL offers higher SFRs than MIP and RIRS. They also purported that RIRS provides better SFRs than MIP and should be the standard of care for renal stones with diameter <20 mm. However, most of the studies included did not utilize NCCT to detect stone residuals. We tried to assess the SFRs and SCRs of all treatment modalities according to postoperative CT follow-up.
By examining the single-arm studies, the outcomes presented are less favorable than the ones reported by using other means to estimate residual fragments [39–45]. Interestingly, by examining the results of the four comparative studies, the results are significantly different in favor of PCNL. More specifically, the SFRs reported were 17–61.3 % for SWL, 50 % for RIRS, and 95–100 % for PCNL [2, 27–29]. Pearle et al. [28] reported SFRs of 35 % and 50 % for SWL and RIRS, respectively (p = 0.92). The SFRs presented by Yuruk and associates [29] were 96.7 and 32.2 % for PCNL and SWL (p < 0.001). Deem et al. [27] presented SFRs at 3 months 85 and 33 % (p = 0.006) for PCNL and SWL, respectively. Finally, Resorlu et al. [2] presented SCRs at 1–2 months for stone residual diameter <4 mm of 91.4, 87.0 and 66.5 % for PCNL, RIRS and SWL, respectively (p < 0.001). These outcomes remain less favorable than the already reported for SWL [39–41] and RIRS [42–45], but are comparable for PCNL [42–45].
Albeit our efforts to reduce heterogeneity of studies dealing with active stone treatment, we should be cognizant that a relative deficiency and heterogeneity of data still exists. First, the quality of the different studies varies, with most of them being descriptive, single-arm, retrospective cohorts (LE 4) and only three of them being randomized prospective trials [27–29]. Moreover, the sample size difference between the three different treatment modalities is undeniable as nine SWL studies with 863 cases, seven SIRS studies with 563 cases, and 11 PCNL studies with 998 patients were included.
The stone characteristics are not clearly defined in all studies. Regarding stone size, some cohorts use the maximum diameter in mm, while others, mainly PCNL, studies the stone surface in mm2 [11, 37, 38]. Additionally, active stone treatment differs according to stone location and size, making a cumulative presentation of outcomes a great challenge. Three of the SWL groups treated single calculi [22–24], while another two reported results by also treating multiple stones [21, 25]. Two studies included only lower pole stones [21, 24], while the rest also reported non-lower and pelvic stones [22, 23, 25]. The stone number range reported in the RIRS studies was 1–3 and all cohorts included lower pole as well as non-lower pole stones. However, the stone number and location in the PCNL groups could not be clearly assessed, possibly because of the high presence of multiple as well as staghorn calculi. Resorlu et al. [2] admit that the size of the stones treated by PCNL was significantly greater than the mean stone sizes of RIRS and SWL. Additionally, especially for SWL, the stone type is an independent predictor for treatment success. However, stone composition is only reported in two studies [2, 29]. The rest of the studies mainly reports stone maximal density in Hounsfield Units [22–25, 27, 28].
Furthermore, no SWL study provides information regarding the possible use of adjuvant expulsive therapy, which can facilitate passage of stones and improve SFRs. Additionally, many SWL studies present their cumulative outcomes and not the SFRs and SCRs after the first session [2, 21, 26–29]. However, many patients required more than one session in order to achieve the desirable result [2, 21, 26, 27, 29]. Stent placement after RIRS as well as the timing of stent removal in relation to performing NCCT could also add important information. Only two RIRS groups placed stents in all patients [30, 33], the rest leaving stent placement in surgeon discretion [2, 28, 31, 32, 34]. Two groups reported the times of stent removal ranging from 1 to 2 weeks postoperatively [2, 30]. Finally, stone dusting during RIRS could present misleading results, as a possible dust accumulation postoperatively does not necessarily mean the presence of significant residual fragments. The use of CT-magnified bone windows can overcome this impediment [46].
Other important intraoperative and postoperative parameters that could influence the results, like surgeon experience, procedure time, CRs, and length of hospitalization constitute possible drawbacks that reflect the greater invasiveness of PCNL [2, 3, 28]. The mean duration of RIRS and PCNL procedures ranged from 43 to 114 min [2, 28–30, 33, 34] and 46.7–149.44 min [2, 28, 29, 38], respectively. However, the authors did not define if the PCNL duration refers to the total duration or the time starting from the kidney puncture and finishing at the end of the procedure. In one study, RIRS had more intraoperative (20 vs. 3 %) but comparable postoperative complications (21.3 vs. 23 %) with SWL [28], and in another, PCNL presented equal complication rates with SWL (6.4 %) [29]. Finally, in the study by Resorlu, the complication rates were significantly higher (p < 0.001) for PCNL (22.1 %) in comparison to RIRS (10.9 %) and SWL (7.6 %) [2]. Nevertheless, only one PCNL study used the Clavien classification system to classify complications [38]. The duration of hospitalization was evident only in two comparative studies ranging 0.06–1.3 days for RIRS and 2.6 days for PCNL [2, 28]. Additionally, as success of PNL is highly surgeon dependent, data on the surgeon experience are of paramount importance for outcome assessment. Unfortunately, this information is unreported in many studies. Finally, although mini-, micro-, and minimally invasive PCNL technology is recently introduced, presenting favorable outcomes and minimizing CRs, no such study presents outcomes according to NCCT follow-up.
The post-treatment imaging utilized to detect stone residuals, but also the best time to perform it, are additional but critical parameters that should always be precisely reported. Currently, many studies substantiate the superiority of NCCT over kidney–ureter–bladder (KUB) X-ray, intravenous pyelography, or ultrasonography in detection and evaluation of residual stones after active treatment, as well as prediction of residual stone-related events and detection of complications of treatment [8–12, 14]. Furthermore, in many occasions, trying to detect residual fragments with plain KUB is like throwing a coin. Park et al. [11] showed that 45.5 % of patients who were stone free with KUB had actually residual stones larger than 4 mm in diameter (mean size: 7.4 mm) detected by CT. In that way, NCCT secures a better treatment plan and the avoidance of unnecessary ancillary treatment. There is also evidence that CT-magnified bone windows are the most accurate method of stone measurement [46]. To our knowledge, this is the first systematic review trying to estimate the treatment outcomes based exclusively on CT findings. Nevertheless, it is of utmost importance to fully describe the technique and equipment used, and the CT exposure data, as well as the length of the sections taken, a factor that also greatly varied in our study. Imaging at the end of the first month after treatment is considered optimal as it gives enough time for stone debris and small insignificant residual fragments to be excreted [11, 47]. Surprisingly, in almost all the PCNL single-arm studies, NCCT was performed before this time period or even direct postoperatively. As a consequence, most probably their presented SFRs and SCRs do not reflect the reality [9, 12, 14, 35–38].
Finally, the most important parameter is the proper definition of the significant residual stone size, as small residual fragments may pass spontaneously without creating stone-related events. In our study, all SWL studies define a cut-off value of 4 mm [21–25] as clinically insignificant. Nevertheless, even smaller residual fragments could cause symptoms and require active intervention [37, 48, 49]. Hence, in the CT-era, and preferably utilizing low-dose CT, trying to achieve a stone-free status should be the absolute target of every endourologist, especially in infected stones. Finally, the need for additional treatment or, in other words, the ancillary procedure rates, are not always reported. Nevertheless, as presented by De et al. [3], the need for further treatment appears to be less in PCNL.
Summarizing the apparent shortcomings of the present review, the selected studies often lack important information regarding stone characteristics like size, number, location, and composition. In particular, for SWL studies, the exact number of sessions is not always reported. Additionally, postoperative CT timing differs between different articles and CT characteristics like quality and collimation are often missing. Finally, heterogeneity of SCRs due to variable definitions of significant residual lithiasis greatly impedes a precise outcome evaluation.
Conclusion
The current data for active stone treatment characteristics and outcomes remain incomplete and greatly heterogeneous. By using NCCT for residual stone size evaluation as a filter, it appears that PCNL offers better SFRs than SWL and RIRS. In light of these results, future studies should adapt to the suggested standardizations and postoperative NCCT control in order to improve the quality of presented data.
References
Turk C, Petrik A, Sarica K, Seitz C, Skolarikos A, Straub M, Knoll T (2016) EAU guidelines on interventional treatment for urolithiasis. Eur Urol 69(3):475–482. doi:10.1016/j.eururo.2015.07.041
Resorlu B, Unsal A, Ziypak T, Diri A, Atis G, Guven S, Sancaktutar AA, Tepeler A, Bozkurt OF, Oztuna D (2013) Comparison of retrograde intrarenal surgery, shockwave lithotripsy, and percutaneous nephrolithotomy for treatment of medium-sized radiolucent renal stones. World J Urol 31(6):1581–1586. doi:10.1007/s00345-012-0991-1
De S, Autorino R, Kim FJ, Zargar H, Laydner H, Balsamo R, Torricelli FC, Di Palma C, Molina WR, Monga M, De Sio M (2015) Percutaneous nephrolithotomy versus retrograde intrarenal surgery: a systematic review and meta-analysis. Eur Urol 67(1):125–137. doi:10.1016/j.eururo.2014.07.003
Breda A, Ogunyemi O, Leppert JT, Lam JS, Schulam PG (2008) Flexible ureteroscopy and laser lithotripsy for single intrarenal stones 2 cm or greater—is this the new frontier? J Urol 179(3):981–984. doi:10.1016/j.juro.2007.10.083
Breda A, Ogunyemi O, Leppert JT, Schulam PG (2009) Flexible ureteroscopy and laser lithotripsy for multiple unilateral intrarenal stones. Eur Urol 55(5):1190–1196. doi:10.1016/j.eururo.2008.06.019
Traxer O, Thomas A (2013) Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J Urol 189(2):580–584. doi:10.1016/j.juro.2012.08.197
Schoenthaler M, Wilhelm K, Katzenwadel A, Ardelt P, Wetterauer U, Traxer O, Miernik A (2012) Retrograde intrarenal surgery in treatment of nephrolithiasis: is a 100% stone-free rate achievable? J Endourol 26(5):489–493. doi:10.1089/end.2011.0405
Pearle MS, Watamull LM, Mullican MA (1999) Sensitivity of noncontrast helical computerized tomography and plain film radiography compared to flexible nephroscopy for detecting residual fragments after percutaneous nephrostolithotomy. J Urol 162(1):23–26. doi:10.1097/00005392-199907000-00006
Waldmann TB, Lashley DB, Fuchs EF (1999) Unenhanced computerized axial tomography to detect retained calculi after percutaneous ultrasonic lithotripsy. J Urol 162(2):312–314
Kupeli B, Gurocak S, Tunc L, Senocak C, Karaoglan U, Bozkirli I (2005) Value of ultrasonography and helical computed tomography in the diagnosis of stone-free patients after extracorporeal shock wave lithotripsy (USG and helical CT after SWL). Int Urol Nephrol 37(2):225–230. doi:10.1007/s11255-004-7975-z
Park J, Hong B, Park T, Park HK (2007) Effectiveness of noncontrast computed tomography in evaluation of residual stones after percutaneous nephrolithotomy. J Endourol 21(7):684–687. doi:10.1089/end.2006.0352
Osman Y, El-Tabey N, Refai H, Elnahas A, Shoma A, Eraky I, Kenawy M, El-Kapany H (2008) Detection of residual stones after percutaneous nephrolithotomy: role of nonenhanced spiral computerized tomography. J Urol 179(1):198–200. doi:10.1016/j.juro.2007.08.175 (Discussion 200)
Guner B, Gurbuz C, Canat L, Caskurlu T (2012) Place of non contrast thin-slice spiral computed tomography in evaluation of stone-free ratio after percutaneous nephrolithotomy. Curr Urol 6(2):71–75. doi:10.1159/000343512
Gokce MI, Ozden E, Suer E, Gulpinar B, Gulpinar O, Tangal S (2015) Comparison of imaging modalities for detection of residual fragments and prediction of stone related events following percutaneous nephrolitotomy. Int Braz J Urol 41(1):86–90. doi:10.1590/s1677-5538.ibju.2015.01.12
Semins MJ, Bartik L, Chew BH, Hyams ES, Humphreys M, Miller NL, Shah O, Paterson RF, Matlaga BR (2011) Multicenter analysis of postoperative CT findings after percutaneous nephrolithotomy: defining complication rates. Urology 78(2):291–294. doi:10.1016/j.urology.2010.11.008
Jellison FC, Smith JC, Heldt JP, Spengler NM, Nicolay LI, Ruckle HC, Koning JL, Millard WW 2nd, Jin DH, Baldwin DD (2009) Effect of low dose radiation computerized tomography protocols on distal ureteral calculus detection. J Urol 182(6):2762–2767. doi:10.1016/j.juro.2009.08.042
Niemann T, Kollmann T, Bongartz G (2008) Diagnostic performance of low-dose CT for the detection of urolithiasis: a meta-analysis. AJR Am J Roentgenol 191(2):396–401. doi:10.2214/ajr.07.3414
Berkenblit R, Hoenig D, Lerer D, Moses M, Minsky L (2013) Comparison of 0.625-mm source computed tomographic images versus 5-mm thick reconstructed images in the evaluation for renal calculi in at-risk patients. J Endourol 27(2):238–241. doi:10.1089/end.2012.0157
Ketelslegers E, Van Beers BE (2006) Urinary calculi: improved detection and characterization with thin-slice multidetector CT. Eur Radiol 16(1):161–165. doi:10.1007/s00330-005-2813-y
Clark HD, Wells GA, Huet C, McAlister FA, Salmi LR, Fergusson D, Laupacis A (1999) Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials 20(5):448–452
Madbouly K, Sheir KZ, Elsobky E (2001) Impact of lower pole renal anatomy on stone clearance after shock wave lithotripsy: fact or fiction? J Urol 165(5):1415–1418
Ng CF, Luke S, Chiu PK, Teoh JY, Wong KT, Hou SS (2015) The effect of renal cortical thickness on the treatment outcomes of kidney stones treated with shockwave lithotripsy. Korean J Urol 56(5):379–385. doi:10.4111/kju.2015.56.5.379
Ouzaid I, Al-qahtani S, Dominique S, Hupertan V, Fernandez P, Hermieu JF, Delmas V, Ravery V (2012) A 970 Hounsfield units (HU) threshold of kidney stone density on non-contrast computed tomography (NCCT) improves patients’ selection for extracorporeal shockwave lithotripsy (ESWL): evidence from a prospective study. BJU Int 110(11 Pt B):E438–E442. doi:10.1111/j.1464-410X.2012.10964.x
Torricelli FC, Marchini GS, Yamauchi FI, Danilovic A, Vicentini FC, Srougi M, Monga M, Mazzucchi E (2015) Impact of renal anatomy on shock wave lithotripsy outcomes for lower pole kidney stones: results of a prospective multifactorial analysis controlled by computerized tomography. J Urol 193(6):2002–2007. doi:10.1016/j.juro.2014.12.026
Wang LJ, Wong YC, Chuang CK, Chu SH, Chen CS, See LC, Chiang YJ (2005) Predictions of outcomes of renal stones after extracorporeal shock wave lithotripsy from stone characteristics determined by unenhanced helical computed tomography: a multivariate analysis. Eur Radiol 15(11):2238–2243. doi:10.1007/s00330-005-2742-9
El-Nahas AR, El-Assmy AM, Mansour O, Sheir KZ (2007) A prospective multivariate analysis of factors predicting stone disintegration by extracorporeal shock wave lithotripsy: the value of high-resolution noncontrast computed tomography. Eur Urol 51(6):1688–1693. doi:10.1016/j.eururo.2006.11.048 (discussion 1693–1684)
Deem S, Defade B, Modak A, Emmett M, Martinez F, Davalos J (2011) Percutaneous nephrolithotomy versus extracorporeal shock wave lithotripsy for moderate sized kidney stones. Urology 78(4):739–743. doi:10.1016/j.urology.2011.04.010
Pearle MS, Lingeman JE, Leveillee R, Kuo R, Preminger GM, Nadler RB, Macaluso J, Monga M, Kumar U, Dushinski J, Albala DM, Wolf JS Jr, Assimos D, Fabrizio M, Munch LC, Nakada SY, Auge B, Honey J, Ogan K, Pattaras J, McDougall EM, Averch TD, Turk T, Pietrow P, Watkins S (2005) Prospective, randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J Urol 173(6):2005–2009. doi:10.1097/01.ju.0000158458.51706.56
Yuruk E, Binbay M, Sari E, Akman T, Altinyay E, Baykal M, Muslumanoglu AY, Tefekli A (2010) A prospective, randomized trial of management for asymptomatic lower pole calculi. J Urol 183(4):1424–1428. doi:10.1016/j.juro.2009.12.022
Portis AJ, Rygwall R, Holtz C, Pshon N, Laliberte M (2006) Ureteroscopic laser lithotripsy for upper urinary tract calculi with active fragment extraction and computerized tomography followup. J Urol 175(6):2129–2133. doi:10.1016/s0022-5347(06)00311-9 (discussion 2133–2124)
Macejko A, Okotie OT, Zhao LC, Liu J, Perry K, Nadler RB (2009) Computed tomography-determined stone-free rates for ureteroscopy of upper-tract stones. J Endourol 23(3):379–382. doi:10.1089/end.2008.0240
Rippel CA, Nikkel L, Lin YK, Danawala Z, Olorunnisomo V, Youssef RF, Pearle MS, Lotan Y, Raman JD (2012) Residual fragments following ureteroscopic lithotripsy: incidence and predictors on postoperative computerized tomography. J Urol 188(6):2246–2251. doi:10.1016/j.juro.2012.08.040
Takazawa R, Kitayama S, Tsujii T (2012) Successful outcome of flexible ureteroscopy with holmium laser lithotripsy for renal stones 2 cm or greater. Int J Urol 19(3):264–267. doi:10.1111/j.1442-2042.2011.02931.x
Ito H, Sakamaki K, Kawahara T, Terao H, Yasuda K, Kuroda S, Yao M, Kubota Y, Matsuzaki J (2015) Development and internal validation of a nomogram for predicting stone-free status after flexible ureteroscopy for renal stones. BJU Int 115(3):446–451. doi:10.1111/bju.12775
Roy OP, Angle JF, Jenkins AD, Schenkman NS (2012) Cone beam computed tomography for percutaneous nephrolithotomy: initial evaluation of a new technology. J Endourol 26(7):814–818. doi:10.1089/end.2011.0478
Geterud K, Henriksson C, Pettersson S, Zachrisson BF (1987) Computed tomography after percutaneous renal stone extraction. Acta Radiol 28(1):55–58
Portis AJ, Laliberte MA, Tatman P, Lendway L, Rosenberg MS, Bretzke CA (2014) Retreatment after percutaneous nephrolithotomy in the computed tomographic era: long-term follow-up. Urology 84(2):279–284. doi:10.1016/j.urology.2014.02.041
Akhavein A, Henriksen C, Syed J, Bird VG (2015) Prediction of single procedure success rate using S.T.O.N.E. nephrolithometry surgical classification system with strict criteria for surgical outcome. Urology 85(1):69–73. doi:10.1016/j.urology.2014.09.010
White W, Klein F (2006) Five-year clinical experience with the Dornier Delta lithotriptor. Urology 68(1):28–32. doi:10.1016/j.urology.2006.01.031
Chung VY, Turney BW (2016) The success of shock wave lithotripsy (SWL) in treating moderate-sized (10–20 mm) renal stones. Urolithiasis. doi:10.1007/s00240-015-0857-2
Alexander CE, Gowland S, Cadwallader J, Reynard JM, Turney BW (2016) Shock wave lithotripsy (SWL): outcomes from a national SWL database in New Zealand. BJU Int 117(Suppl 4):76–81. doi:10.1111/bju.13431
Akman T, Binbay M, Ozgor F, Ugurlu M, Tekinarslan E, Kezer C, Aslan R, Muslumanoglu AY (2012) Comparison of percutaneous nephrolithotomy and retrograde flexible nephrolithotripsy for the management of 2–4 cm stones: a matched-pair analysis. BJU Int 109(9):1384–1389. doi:10.1111/j.1464-410X.2011.10691.x
Bozkurt OF, Resorlu B, Yildiz Y, Can CE, Unsal A (2011) Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J Endourol 25(7):1131–1135. doi:10.1089/end.2010.0737
Bryniarski P, Paradysz A, Zyczkowski M, Kupilas A, Nowakowski K, Bogacki R (2012) A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal surgery in the management of renal stones more than 2 cm in diameter. J Endourol 26(1):52–57. doi:10.1089/end.2011.0235
Ozturk U, Sener NC, Goktug HN, Nalbant I, Gucuk A, Imamoglu MA (2013) Comparison of percutaneous nephrolithotomy, shock wave lithotripsy, and retrograde intrarenal surgery for lower pole renal calculi 10-20 mm. Urol Int 91(3):345–349. doi:10.1159/000351136
Eisner BH, Kambadakone A, Monga M, Anderson JK, Thoreson AA, Lee H, Dretler SP, Sahani DV (2009) Computerized tomography magnified bone windows are superior to standard soft tissue windows for accurate measurement of stone size: an in vitro and clinical study. J Urol 181(4):1710–1715. doi:10.1016/j.juro.2008.11.116
Portis AJ, Laliberte MA, Holtz C, Ma W, Rosenberg MS, Bretzke CA (2008) Confident intraoperative decision making during percutaneous nephrolithotomy: does this patient need a second look? Urology 71(2):218–222. doi:10.1016/j.urology.2007.08.063
Osman Y, Harraz AM, El-Nahas AR, Awad B, El-Tabey N, Shebel H, Shoma AM, Eraky I, El-Kenawy M (2013) Clinically insignificant residual fragments: an acceptable term in the computed tomography era? Urology 81(4):723–726. doi:10.1016/j.urology.2013.01.011
El-Nahas AR, El-Assmy AM, Madbouly K, Sheir KZ (2006) Predictors of clinical significance of residual fragments after extracorporeal shockwave lithotripsy for renal stones. J Endourol 20(11):870–874. doi:10.1089/end.2006.20.870
Author’s contribution
T Tokas contributed to project development, data collection, data analysis and manuscript writing. M Habicher contributed to data collection and data analysis. D Junker helped in manuscript editing. T Herrmann contributed to manuscript editing. JP Jessen contributed to manuscript editing. T Knoll helped in manuscript editing. U Nagele contributed to project development and manuscript editing.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
This review does not involve human participants and/or animals.
Appendices
Appendix 1
The pubMed search was performed by two independent reviewers (TT, MH) and the keywords used were selected after their consensus and the suggestions of the senior author.
Appendix 2
Criteria for considering studies
-
patients/participants: Healthy non-obese adults (mean age: 29.6–62)
-
interventions: SWL, RIRS and standard PCNL
-
comparators: NCCT
-
outcomes: Stone-free rates and stone clearance rates according to NCCT findings.
Rights and permissions
About this article
Cite this article
Tokas, T., Habicher, M., Junker, D. et al. Uncovering the real outcomes of active renal stone treatment by utilizing non-contrast computer tomography: a systematic review of the current literature. World J Urol 35, 897–905 (2017). https://doi.org/10.1007/s00345-016-1943-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1943-y