Abstract
Purpose
Guidelines recommend risk-adapted follow-up (FU) strategies after (partial) nephrectomy in non-metastatic renal cell carcinoma (RCC). Since current systemic therapy does not cure metastatic RCC, only timely detected recurrence accessible for local therapy is potentially curable. This study analyzed the rate and management of potentially curable recurrences per risk group.
Methods
This is a retrospective study including non-metastatic RCC patients who underwent (partial) nephrectomy from 2004 to 2011, with a minimum follow-up of 4 years. Risk stratification was by Leibovich score (clear cell subtype) and UICC/AJCC grading (other subtypes). Recurrence, time to recurrence, symptoms and detection method were documented. Isolated local recurrence, solitary- and oligometastases (≤3 lesions, single site) were considered potentially curable.
Results
Among 234 patients, followed during a median of 61.9 months, 68 patients (29.1 %) developed a recurrence of which 28 (41.2 %) were considered potentially curable. The 5-year risk of recurrence for low-, intermediate- and high-risk patients was 7.8, 26.3 and 59.1 % of which 71.4, 52.2 and 23.1 % were considered potentially curable, respectively. In high-risk patients, incurable recurrence was detected after a median of 7.9 (3.7–17.2) months versus 13.9 (6–41.3) months for potentially curable lesions. Only 13 of potentially curable lesions (46 %) received local therapy.
Conclusion
FU protocols should be adapted to the recurrence pattern of potentially curable disease. Most of the benefit may be achieved in intermediate-risk and high-risk-patients free of recurrence 1 year after surgery. Despite frequent imaging, only 13 patients (5.6 % of all patients followed) were managed with local therapy of whom only 4 remained free of disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Up to 20–30 % of patients managed surgically for non-metastatic RCC develop local or distant recurrences in the follow-up (FU) period [1–4]. Some may be candidates for potentially curative surgical resection of their recurrent lesion(s), or other forms of local therapy [5–7]. However, metastatic RCC unsuitable for local therapeutic options requires systemic treatment which lacks long-term effectiveness. Therefore, advanced disease is generally considered incurable and the prognosis remains poor [8]. Currently, the European Association of Urology (EAU), American Urological Association (AUA) and National Comprehensive Cancer Network (NCCN) guidelines recommend oncological FU after nephrectomy for localized RCC. The goal of FU is to detect recurrent lesions at an early stage, based on the assumption that they are accessible for potentially curative local treatment [9, 10]. Numerous studies recommend FU protocols based on pattern of, and risk factors for, recurrence after resection of localized RCC, and several risk-stratification tools have been developed [1–3, 11–13]. However, none of these FU protocols have been compared prospectively. In addition, intense FU strategies for high-risk disease may rarely allow local treatment, as recurrence in these patients is often widespread. Delaying systemic therapy did not influence survival in placebo-controlled crossover studies, and often, systemic therapy is deferred until further progression occurs in these individuals [14, 15]. For patients with high risk of multiple-site progression, less-frequent and less-intense FU may therefore not negatively impact on treatment strategy and survival. For patients more likely to develop solitary and single-site recurrence, intensive surveillance may provide the opportunity for local salvage therapy and thus survival benefit. Previous studies have failed to clearly report the rate of, and prognostic factors for, patients presenting with potentially curable recurrent disease [1–3, 11–13]. Data on management after detection of potentially curable recurrence are lacking. We therefore analyzed the rate, management and outcome of potentially curable recurrences per risk group.
Patients and methods
Study design and patient selection
This retrospective study involved patients who underwent radical nephrectomy (RN) or partial nephrectomy (PN) for non-metastatic RCC, at two separate Dutch centers, between January 1, 2004, and July 31, 2011. Data were collected from institutional tumor registries with appropriate ethics approval. Criteria for exclusion from analysis were: (1) metastases at presentation, (2) hereditary RCC, (3) death within 90 days after surgery and (4) <48 months of FU.
Data extraction
Data on demographics, surgery, stage, histopathology and FU visits were collected from the medical records. Histopathology was based on the surgical specimen, not on biopsies. For pathological staging, the 7th UICC/AJCC TNM classification was used [16]. Histological subtype was determined according to the Vancouver classification [17]. All clear cell subtypes (ccRCC) were graded according to Fuhrman [18]. For risk stratification, the Leibovich score was calculated for ccRCC (Leibovich scores 0–2: low-risk; 3–5: intermediate-risk and ≥6: high-risk, respectively) [12]. Risk stratification for non-ccRCC was based on the UICC/AJCC staging system [16]. Stage 1 was considered low-risk, stage 2 intermediate-risk and stages 3 and 4 high-risk.
Follow-up analysis
In accordance with EAU [10] and AUA [9] guidelines, the first FU imaging was performed within 6 months after initial surgery. Further FU was performed by local standards, which differed between treating centers. Type of imaging and date during the FU period were documented.
The primary aim was to collect data on the occurrence of recurrent disease. Local renal fossa recurrence was defined as new tumor formation in the lumbar fossa, remaining renal vein or inferior vena cava after RN. Local intrarenal recurrence was defined as new tumor formation within the residual kidney after PN. Distant metastasis was defined as new lesion, at any other anatomical location. Histopathological confirmation was not mandatory for the diagnosis of recurrence. Recurrence was classified as potentially curable or incurable. For the purpose of this study, potentially curable metastases were defined as isolated local recurrence, solitary metastasis or oligometastases (≤3 at a single site) based on retrospective metastasectomy series [7, 19]. Occurrence of multiple metastases (>3) either at one or multiple sites was considered incurable.
In case of recurrence, the first management was documented and classified as either with curative intent, palliative intent or surveillance of lesions. The total duration of FU was calculated from date of initial surgery to either date of death or of last FU. Time to recurrence (TTR) was from date of surgery to detection of recurrence. FU duration after recurrence was from date of recurrence to either date of death or of last contact.
Statistical analysis
IBM© Statistical Package for the Social Sciences (SPSS), version 22.0 (IBM corporation, Armonk, New York, USA), was used. For the descriptive analysis, categorical variables were reported as percentages and continuous variables were presented as median with interquartile range (25th–75th ‰). For the analysis of differences between groups, Fisher’s exact test and Mann–Whitney U test were used. Cumulative incidence of recurrence and survival analysis were conducted using the Kaplan–Meier method. Differences were tested for significance with a log-rank test. In all tests, two-tailed p values were used, and a value <0.05 was regarded as statistically significant. Missing data were handled by pairwise deletion.
Results
Patients
A total of 310 patients had been surgically treated for localized RCC during the inclusion period, of whom 76 were excluded. Fifteen patients had distant metastasis at diagnosis, 29 patients had hereditary RCC, nine died within 90 days after surgery, and 23 had <48 months of FU. The baseline characteristics for the remaining 234 patients included are summarized in Table 1. A total of 3382 imaging modalities were performed.
Pattern of recurrence
During a median FU of 61.9 (49.3–83.3) months, 68 patients [29.1 % (95 % CI 23.3–34.9 %)] recurred with a median time to detection of 22.8 (5.8–44.6) months, 28 of whom [41.2 % (95 % CI 29.5–52.9)] were considered potentially curable (local isolated n = 5, solitary distant n = 15, oligometastatic at a single site n = 8) (Fig. 1). The median TTR for potentially curable recurrences was 23.8 (6.7–41.2) months and 17.6 (5.3–45.0) months for incurable recurrent disease (p = 0.778).
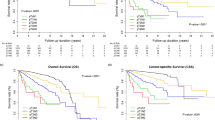
Patients were low-, intermediate- and high-risk in 41.0, 37.6 and 19.2 %, respectively. Risk group stratification significantly correlated with overall recurrence rate (RR) and TTR (p ≤ 0.001). The 5-year RR of and the proportion of potentially curable recurrences was risk-associated (Table 2). In particular, high-risk patients developed recurrence early during FU. Risk stratification also influenced the proportion of potentially curable recurrence and the TTR for potentially curable and incurable recurrence (Fig. 2a, b). Early recurrences within low-risk patients were mainly potentially curable, but within high-risk patients predominantly incurable. Furthermore, no significant difference in TTR between potentially curable and incurable recurrence was found within the intermediate-risk group (p = 0.621).
Kaplan–Meier curves for a cumulative incidence of recurrence for the potentially curable recurrence per risk group, hazard ratio’s with low-risk patients as reference group, b cumulative incidence of recurrence for incurable recurrence per risk group, hazard ratio’s with low-risk patients as reference group, c cumulative survival of patients with potentially curable disease according to treatment strategy and for d cumulative survival of patients with incurable recurrence according to treatment strategy
At univariate analysis, only pT stage of the primary tumor was a predictor for potentially curable recurrent lesion(s) (p = 0.049). There were no statistical differences in potential curability for lesions that were symptomatic (p = 0.206), found within the regular FU strategy (p = 0.059) or found with cross-sectional versus conventional imaging (p = 1.000).
Management and survival
Management of recurrences is described in Fig. 1. Those with locally treated disease had an 80 % (±12.6 SE) 5-year estimated cumulative survival rate, compared to 26.7 % (±11.4 SE) for patients with potentially curable disease without local treatment (Fig. 2c). After local treatment, only four patients are disease-free at 4, 68, 71 and 96 months after metastasectomy [1.7 % (95 % CI 0.05–3.3) of all patients followed and 5.9 % (95 % CI 0.29–11.47) of those diagnosed with recurrence], 75 % (95 % CI 50.5–99.5) recurred after a median of 15 (range 4–43) months, and only one died of disease.
For patients diagnosed with incurable recurrence (n = 40), survival was best in those with deferred treatment (Fig. 2d).
Discussion
Optimal strategies for FU after surgically managed non-metastatic RCC are unknown, owing to a lack of comparative studies [4, 10, 20, 21]. Little is known about the pattern of potentially curable recurrences after surgical resection for non-metastatic RCC. We found a RR comparable to previously reported figures [3, 11, 12, 20, 22–24]. The 5-year estimated RR per risk group was comparable to those in the original study [12] and external validations [23, 25]. Potentially curable recurrences were found in 12 % of the entire population and 41.2 % of all recurrences. Of all recurrences, 46 (67.6 %) were single-site recurrences, comparable to previous reports [11, 26–28]. However, these studies did not investigate the potential curability of single-site recurrence. In the current study, 39.1 % of single-site recurrences were multiple and therefore considered irresectable and incurable.
In 234 patients, a total of 3382 imaging modalities have been used during FU, but only 13 patients were eventually managed with potentially curative local therapy. Ultimately, 75 % suffered further recurrence, and only four patients have currently no evidence of disease. This suggests that only 1.7 % (95 % CI 0.05–3.3) of all patients followed may benefit from FU in terms of cure once a recurrence is detected. However, patients with potentially curable disease treated with curative intent did show superior survival over patients not treated locally.
The proportion of potentially curable recurrence was associated with the risk score, and also, differences in TTR were observed when stratifying for risk group. For low-risk patients, the 5-year cumulative risk of recurrence was 7.8 %, of whom 71.4 % had potentially curable disease. Only seven low-risk patients developed recurrent disease limiting statistically robust conclusions. Also, since the RR is low in low-risk, intensive FU is unlikely to be cost-effective. For intermediate-risk patients, 52.2 % of the recurrences were considered potentially curable and the risk of recurrence seemed to be consistent over time and similar for both potentially curable and incurable disease. Also, approximately half of the patients with potentially curable recurrence within this risk group were indeed treated with curative intent. Intensive FU may therefore reveal benefit in detecting curable lesions within this risk group.
High-risk patients had a high 5-year cumulative risk of recurrence (59.1 %), but only 23.1 % had potentially curable disease. Within this risk group, incurable recurrent disease developed earlier than potentially curable recurrence. However, the very early recurrences might have been occult M1 disease at initial diagnosis. Nevertheless, previous literature confirms that most recurrences in high-risk patients occur a short time after initial surgery and resulted in decreased survival [22–29]. Prior studies have therefore promoted intensive FU protocols for high-risk patients in the first period after surgically managed localized RCC [4, 10]. Our results suggest that early recurrences in the high-risk group were predominantly incurable. Within the first year after initial surgery, 86.7 % of the recurrences were multiple. Only 2 of 15 recurrences within the first year were potentially curable and in both cases, no curative treatment followed due to expected rapid multiple-site progression, which indeed occurred in both. Since deferred systemic therapy does not negatively influence survival in asymptomatic patients, intensive FU in the first year after initial nephrectomy for high-risk patients will most likely be inefficient. However, in patients surviving the first year without recurrence, intensified FU might effectively detect potentially curable lesions.
This retrospective study has several limitations. Outcome after local treatment of recurrence may be biased by better performance in patients treated with curative intent. Although all patients were followed by regular imaging, frequency and imaging modality varied which may have influenced TTR and RR. The amount of lesions accessible for complete resection and potential cure is debatable since long-term survival has even been described after metastasectomy of 32 pulmonary lesions [30]. Nevertheless, a systematic review revealed that in most publications, 1–3 lesions were resected on average with curative intent [7]. For the purpose of this study, an arbitrary number of ≤3 lesions at one anatomical site was therefore considered appropriate for surgical resection. We are aware of the limitation of this definition. However, to analyze potential associations, we decided to choose a cutoff which may reflect clinical practice in most cases.
In conclusion, FU should be adapted to the risk of potentially curable recurrence. Despite cure being rare after resection, treatment of potentially curable recurrence was associated with significant survival benefit. Potentially curable recurrent disease is mainly found within the low-risk group, but overall RR is low. Conversely, high-risk patients have a high RR of predominantly non-curable lesions early during FU. Therefore, most of the benefit of regular FU may be achieved in intermediate-risk and high-risk-patients free of recurrence 1 year after surgery.
Abbreviations
- AJCC:
-
American Joint Cancer Committee
- AUA:
-
American Urological Association
- ccRCC:
-
Clear cell renal cell carcinoma
- EAU:
-
European Association of Urology
- FU:
-
Follow-up
- NCCN:
-
National Comprehensive Cancer Network
- PN:
-
Partial nephrectomy
- RCC:
-
Renal cell carcinoma
- RFS:
-
Recurrence-free survival
- RN:
-
Radical nephrectomy
- SE:
-
Standard error
- TNM:
-
Tumor-node-metastasis
- TTR:
-
Time to recurrence
- UICC:
-
Union for International Cancer Control
References
Frank I, Blute ML, Cheville JC, Lohse CM, Weaver AL, Leibovich BC, Zincke H (2003) A multifactorial postoperative surveillance model for patients with surgically treated clear cell renal cell carcinoma. J Urol 170(6 Pt 1):2225–2232. doi:10.1097/01.ju.0000095541.10333.a7
Lam JS, Leppert JT, Figlin RA, Belldegrun AS (2005) Surveillance following radical or partial nephrectomy for renal cell carcinoma. Curr Urol Rep 6(1):7–18
Antonelli A, Cozzoli A, Zani D, Zanotelli T, Nicolai M, Cunico SC, Simeone C (2007) The follow-up management of non-metastatic renal cell carcinoma: definition of a surveillance protocol. BJU Int 99(2):296–300
van Oostenbrugge TJ, Kroeze SG, Bosch JL, van Melick HH (2015) The blind spots in follow-up after nephrectomy or nephron-sparing surgery for localized renal cell carcinoma. World J Urol 33(6):881–887. doi:10.1007/s00345-014-1390-6
Breau RH, Blute ML (2010) Surgery for renal cell carcinoma metastases. Curr Opin Urol 20(5):375–381
Ljungberg B (2013) The role of metastasectomy in renal cell carcinoma in the era of targeted therapy. Curr Urol Rep 14(1):19–25
Dabestani S, Marconi L, Hofmann F, Stewart F, Lam TBL, Canfield SE, Staehler M, Powles T, Ljungberg B, Bex A (2014) Local treatments for metastases of renal-cell carcinoma: a systematic review. Lancet Oncol 15(12):e549–e561
Klatte T, Lam JS, Shuch B, Belldegrun AS, Pantuck AJ (2008) Surveillance for renal cell carcinoma: why and how? When and how often? Urol Oncol 26(5):550–554. doi:10.1016/j.urolonc.2007.05.026
Donat SM, Diaz M, Bishoff JT, Coleman JA, Dahm P, Derweesh IH, Herrell SD 3rd, Hilton S, Jonasch E, Lin DW, Reuter VE, Chang SS (2013) Follow-up for clinically localized renal neoplasms: AUA guideline. J Urol 190(2):407–416. doi:10.1016/j.juro.2013.04.121
Ljungberg B, Bensalah K, Canfield S, Dabestani S, Hofmann F, Hora M, Kuczyk MA, Lam T, Marconi L, Merseburger AS, Mulders P, Powles T, Staehler M, Volpe A, Bex A (2015) EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol 67(5):913–924. doi:10.1016/j.eururo.2015.01.005
Stephenson AJ, Chetner MP, Rourke K, Gleave ME, Signaevsky M, Palmer B, Kuan J, Brock GB, Tanguay S (2004) Guidelines for the surveillance of localized renal cell carcinoma based on the patterns of relapse after nephrectomy. J Urol 172(1):58–62. doi:10.1097/01.ju.0000132126.85812.7d
Leibovich BC, Blute ML, Cheville JC, Lohse CM, Frank I, Kwon ED, Weaver AL, Parker AS, Zincke H (2003) Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: a stratification tool for prospective clinical trials. Cancer 97(7):1663–1671
Siddiqui SA, Frank I, Cheville JC, Lohse CM, Leibovich BC, Blute ML (2009) Postoperative surveillance for renal cell carcinoma: a multifactorial histological subtype specific protocol. BJU Int 104(6):778–785. doi:10.1111/j.1464-410X.2009.08499.x
Sternberg CN, Davis ID, Mardiak J, Szczylik C, Lee E, Wagstaff J, Barrios CH, Salman P, Gladkov OA, Kavina A, Zarba JJ, Chen M, McCann L, Pandite L, Roychowdhury DF, Hawkins RE (2010) Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol 28(6):1061–1068
Motzer RJ, Escudier B, Oudard S, Hutson TE, Porta C, Bracarda S, Grunwald V, Thompson JA, Figlin RA, Hollaender N, Kay A, Ravaud A (2010) Phase 3 trial of everolimus for metastatic renal cell carcinoma: final results and analysis of prognostic factors. Cancer 116(18):4256–4265. doi:10.1002/cncr.25219
Martinez-Salamanca JI, Huang WC, Millan I, Bertini R, Bianco FJ, Carballido JA, Ciancio G, Hernandez C, Herranz F, Haferkamp A, Hohenfellner M, Hu B, Koppie T, Martinez-Ballesteros C, Montorsi F, Palou J, Pontes JE, Russo P, Terrone C, Villavicencio H, Volpe A, Libertino JA (2011) Prognostic impact of the 2009 UICC/AJCC TNM staging system for renal cell carcinoma with venous extension. Eur Urol 59(1):120–127. doi:10.1016/j.eururo.2010.10.001
Srigley JR, Delahunt B, Eble JN, Egevad L, Epstein JI, Grignon D, Hes O, Moch H, Montironi R, Tickoo SK, Zhou M, Argani P (2013) The international society of urological pathology (ISUP) vancouver classification of renal neoplasia. Am J Surg Pathol 37(10):1469–1489. doi:10.1097/PAS.0b013e318299f2d1
Fuhrman SA, Lasky LC, Limas C (1982) Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol 6(7):655–663
Alt AL, Boorjian SA, Lohse CM, Costello BA, Leibovich BC, Blute ML (2011) Survival after complete surgical resection of multiple metastases from renal cell carcinoma. Cancer 117(13):2873–2882
Stewart SB, Thompson RH, Psutka SP, Cheville JC, Lohse CM, Boorjian SA, Leibovich BC (2014) Evaluation of the National Comprehensive Cancer Network and American Urological Association renal cell carcinoma surveillance guidelines. J Clin Oncol 32(36):4059–4065. doi:10.1200/jco.2014.56.5416
Zargar-Shoshtari K, Kim T, Simon R, Lin HY, Yue B, Sharma P, Spiess PE, Poch MA, Pow Sang J, Sexton WJ (2015) Surveillance following nephron-sparing surgery: an assessment of recurrence patterns and surveillance costs. Urology 86(2):321–326. doi:10.1016/j.urology.2015.05.013
Brookman-May SD, May M, Shariat SF, Novara G, Zigeuner R, Cindolo L, De Cobelli O, De Nunzio C, Pahernik S, Wirth MP, Longo N, Simonato A, Serni S, Siracusano S, Volpe A, Morgia G, Bertini R, Dalpiaz O, Stief C, Ficarra V (2013) Time to recurrence is a significant predictor of cancer-specific survival after recurrence in patients with recurrent renal cell carcinoma–results from a comprehensive multi-centre database (CORONA/SATURN-Project). BJU Int 112(7):909–916. doi:10.1111/bju.12246
Pichler M, Hutterer GC, Chromecki TF, Jesche J, Kampel-Kettner K, Rehak P, Pummer K, Zigeuner R (2011) External validation of the Leibovich prognosis score for nonmetastatic clear cell renal cell carcinoma at a single European center applying routine pathology. J Urol 186(5):1773–1777. doi:10.1016/j.juro.2011.07.034
Lam JS, Shvarts O, Leppert JT, Pantuck AJ, Figlin RA, Belldegrun AS (2005) Postoperative surveillance protocol for patients with localized and locally advanced renal cell carcinoma based on a validated prognostic nomogram and risk group stratification system. J Urol 174(2):466–472; discussion 472; quiz 801. doi:10.1097/01.ju.0000165572.38887.da
Beisland C, Gudbrandsdottir G, Reisaeter LA, Bostad L, Wentzel-Larsen T, Hjelle KM (2015) Contemporary external validation of the Leibovich model for prediction of progression after radical surgery for clear cell renal cell carcinoma. Scand J Urol 49(3):205–210. doi:10.3109/21681805.2014.980844
Bianchi M, Sun M, Jeldres C, Shariat SF, Trinh QD, Briganti A, Tian Z, Schmitges J, Graefen M, Perrotte P, Menon M, Montorsi F, Karakiewicz PI (2012) Distribution of metastatic sites in renal cell carcinoma: a population-based analysis. Ann Oncol 23(4):973–980
Meimarakis G, Angele M, Staehler M, Clevert DA, Crispin A, Ruttinger D, Lohe F, Preissler G, Hatz RA, Winter H (2011) Evaluation of a new prognostic score (Munich score) to predict long-term survival after resection of pulmonary renal cell carcinoma metastases. Am J Surg 202(2):158–167
Han KR, Pantuck AJ, Bui MH, Shvarts O, Freitas DG, Zisman A, Leibovich BC, Dorey FJ, Gitlitz BJ, Figlin RA, Belldegrun AS (2003) Number of metastatic sites rather than location dictates overall survival of patients with node-negative metastatic renal cell carcinoma. Urology 61(2):314–319
Abdollah F, Suardi N, Capitanio U, Matloob R, Fossati N, Castiglione F, Di Trapani E, Di Trapani D, Russo A, Carenzi C, Montorsi F, Rigatti P, Bertini R (2014) The key role of time in predicting progression-free survival in patients with renal cell carcinoma treated with partial or radical nephrectomy: conditional survival analysis. Urol Oncol. doi:10.1016/j.urolonc.2013.05.006
Piltz S, Meimarakis G, Wichmann MW, Hatz R, Schildberg FW, Fuerst H (2002) Long-term results after pulmonary resection of renal cell carcinoma metastases. Ann Thorac Surg 73(4):1082–1087
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Authors’ contribution
Each author certifies that he or she has participated sufficiently in the intellectual content, data analysis and writing of the work to take public responsibility for it. Each author has read the work, believes it represents valid work, and approves it for publication. We herewith state that all authors had an equal contribution to this study. Y.A.M. Kuijpers carried out the complete acquisition of data, carried out the full analysis and interpretation of data, and made the draft for the manuscript. R.P. Meijer was substantially involved in the development of the study protocol, carried out a substantial part of the data acquisition, and made revisions to the manuscript. J.L.H.R. Bosch and S. Horenblas were responsible for supervision and scientific revision of the manuscript. G.N. Jonges and J. de Jong were supervising pathologists and helped with data acquisition. A. Bex was responsible for the development of the study protocol, supervising the study design, contributed to data acquisition and data interpretations, and made revisions to the manuscript.
Conflict of interest
None of the authors declare to have any conflict of interest associated with the current study.
Rights and permissions
About this article
Cite this article
Kuijpers, Y.A.M., Meijer, R.P., Jonges, G.N. et al. Potentially curable recurrent disease after surgically managed non-metastatic renal cell carcinoma in low-, intermediate- and high-risk patients. World J Urol 34, 1073–1079 (2016). https://doi.org/10.1007/s00345-016-1822-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1822-6