Abstract
Objectives
To analyze the impact of surgeon’s experience on surgical margin status, postoperative continence and operative time after radical prostatectomy (RP) in a surgeon who performed more than 2000 open RP.
Patients and methods
We retrospectively analyzed 2269 patients who underwent RP by one surgeon from April 2004 to June 2012. Multivariable logistic models were used to quantify the impact of surgeon’s experience (measured by the number of prior performed RP) on surgical margin status, postoperative continence and operative time.
Results
Negative surgical margin rate was 86 % for patients with pT2 stage, and continence rate at 3 years after RP was 94 %. Patients with negative surgical margin had lower preoperative PSA level (p = 0.02), lower pT stage (p < 0.001) and lower Gleason score (p < 0.001). The influence of the experience of the surgeon was nonlinear, positive and highly significant up to 750 performed surgeries (75–90 % negative surgical margin) (p < 0.01). The probability of continence rises significantly with surgeon’s experience (from 88–96 %) (p < 0.05). A reduction in operative time (90–65 min) per RP was observed up to 1000 RP.
Conclusions
In the present study, we showed evidence that surgeon’s experience has a strong positive impact on pathologic and functional outcomes as well as on operative time. While significant learning effects concerning positive surgical margin rate and preserved long-term continence were detectable during the first 750 and 300 procedures, respectively, improvement in operative time was detectable up to a threshold of almost 1000 RP and hence is relevant even for very high-volume surgeons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical prostatectomy (RP) remains the standard treatment of clinically localized prostate cancer around the world, providing excellent long-term outcomes [1–3]. The procedure remains challenging because of its close relation to important anatomic structures.
Despite being one of the most striking problems in surgery, a precise definition of the surgeon’s learning curve is still lacking and its measurement remains difficult. The surgeon’s learning curve is usually defined as the period of time during which the surgical procedure is more difficult, less effective and accompanied by more complications due to surgeon’s inexperience [4]. Artibani et al. [5] referred to the surgeon’s learning curve as the period of time until a surgical procedure is performed within a reasonable operative time with acceptable complication rates as well as a proper oncologic and functional outcome. In the early 2000s, several studies focused on the impact of surgeon’s experience and found a significant correlation between hospital’s or surgeon’s volumes and perioperative outcomes (blood loss, duration of surgery, length of hospital stay, complication or readmission rates and perioperative mortality), functional outcomes (bladder neck strictures, continence rates) or oncologic outcomes (positive surgical margin rate, PSA value 3 months after surgery) [6–8]. Focusing on the long-term oncologic outcomes, Vickers et al. [9] reported that the risk of prostate cancer recurrence by 5 years is significantly lower if the patient was treated by an experienced surgeon with at least 250 prior cases compared to a less experienced surgeon with 10 prior cases (10.7 vs. 17.9 %). Similar findings were reported concerning the positive surgical margin rate (25 vs. 40 %) [10]. In a recent review, Trinh et al. [11] systematically analyzed 28 studies, which investigated the relation between surgeon’s volume and perioperative outcomes and confirmed a strong relationship between surgeon’s case load and parameters such as continence rates, perioperative blood loss, positive surgical margin rates, duration of hospital stay, hospital charges, perioperative complications as well as biochemical recurrence rates. In the last decade, a certain number of studies focused on the learning curves concerning the minimally invasive approach of RP. Vickers et al. [12] analyzed a cohort of 4702 patients and found an evident reduction in cancer recurrence when laparoscopic RP was performed by an experienced surgeon.
In this study, we focused on the learning curve of one highly experienced surgeon to investigate whether there is an improvement in oncologic and functional outcomes even after a large number of prior performed open RP. We therefore analyzed the impact of surgeon’s experience on surgical margin status, postoperative continence and operative time after open RP in a surgeon with more than 2000 performed open RP.
Methods
Surgical procedure
From April 2004 to June 2012, 2269 open retropubic radical prostatectomies (RP) were performed by one single experienced high-volume surgeon (CGS) at the Department of Urology, Ludwig-Maximilians-University Munich. No extensive changes in surgical technique were introduced during the period mentioned above. Nerve sparing was performed through careful incision of the lateral periprostatic endopelvic fascia above the vasa vesicales superiores and incision of the two fascias below, guaranteeing a complete and accurate preparation as well as lateral shift of the tissue with consecutive conservation of the crossing autonomic nerves as well as careful ventral luxation of the prostate to preserve nerves that are running ventrally of the rectum and accurate preparation of the lateral seminal vesicle region. Pelvic lymphadenectomy was regularly performed in intermediate- and high-risk patients. An 18F Foley catheter was placed in the bladder intraoperatively and left in situ for 7 days in average. Removal of the Foley catheter followed a cystography to document sufficiency of the vesicourethral anastomosis.
Statistical analysis and creation of learning curve
For comparison reasons, we partly followed Vickers et al. [10] in producing the learning curves. To evaluate the association between surgeon experience and surgical margin status, we ran a multivariable logistic regression model. Thereby, we focused on the subsample of patients with T2 tumors (n = 1637) as surgical margin status in these patients is influenced by the operating surgeon. As independent variables, surgeon experience (modeled as a cubic function and measured through the number of prior performed RP), age at surgery, preoperative PSA level, pathologic Gleason grade (categorized as ≤6, 7, and ≥8), performed lymphadenectomy, lymph node involvement and variables for the respective T2 subgroups were added to the regression. Continence was defined as 0–1 safety pads per day. Information on continence was collected by standardized self-administrated questionnaires which were routinely sent to all patients by our data manager. The probability of 3-year continence for patients with all tumor stages was computed from a second multivariable logistic regression using the same covariates as in the regression for surgical margin status, excluding the variables for T2 subgroups, and entering extraprostatic extension and seminal vesicle invasion. In both regressions, the total number of prior RP was used as surgeon experience regardless of the pathologic stage of the tumor. Furthermore, to check for a relationship between surgeon experience and operative time, a multivariable ordinary least squares regression was performed, including the same covariates as mentioned above. Operative time was defined from skin to skin. In all regressions, robust standard errors were used. As statistical software, STATA was used (version 11 for Windows, StataCorp LP, College Station, TX). To produce a learning curve, we used the mean values of covariates to estimate the probability of a positive surgical margin, 3-year rate of continence and operative time predicted by the model for each level of surgical experience. To check for differences in our respective subsamples, two-group mean-comparison t tests, Pearson’s Chi-squared tests and Wilcoxon–Mann–Whitney tests were performed.
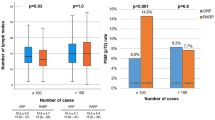
Results
Descriptive statistics of patient characteristics are summarized in Table 1. Overall, a negative surgical margin was documented in 73.3 % of patients with all pT stages, in 86.0 % with pT2 tumor stages and in 58.4 % of patients with pT3 tumors. Continence 3 years after RP was reached in 94.0 % of 947 patients who supplied sufficient information about their postoperative continence status. Patients with a negative surgical margin had a significantly higher rate of a low (<10 ng/mL) preoperative PSA level (p = 0.02), lower Gleason grades (p < 0.001) and lower pT2 subgroups (p < 0.001). In multivariable logistic regression analysis, preoperative PSA level <10 ng/mL (OR 1.43, 95 % CI 1.02–2.01, p = 0.04) and pT2a stage (vs. pT2c) (OR 2.37, 95 % CI 1.38–4.08, p < 0.01) had a significant positive impact on the probability of a negative surgical margin. A Gleason score of seven compared to a Gleason score ≤6 was associated with a higher proportion of negative surgical margins (OR 0.60, 95 % CI 0.43–0.82, p < 0.01). The influence of the experience of the surgeon on the probability of a negative surgical margin was nonlinear and positive up to 500–750 performed surgeries before it became flat and insensitive to a further increase in surgeon’s experience. At the starting point, the probability of a negative surgical margin is only a little above 70 %, while it rises to values of 90 % after 750 cases (Table 2; Fig. 1, p < 0.01).
Surgical learning curve for a negative surgical margin in patients with pT2 tumor stage. Predicted probability (solid graph) and 95 % confidence intervals (dotted graphs) of a negative surgical margin are plotted against the number of prior surgeries. Probabilities are evaluated at means of covariates and reflect a patient with typical sample characteristics
The probability of continence 3 years after surgery decreased with an increase in patients’ age (OR 0.93 per year, 95 % CI 0.88–0.98, p < 0.01). Again, the probability of continence rises nonlinearly and significantly with surgeons experience up to approximately 300 prior surgeries until a plateau is reached, where the probability of continence oscillates around 95 % (Table 2; Fig. 2, p < 0.05).
Surgical learning curve for 3-year postoperative continence. Predicted rate (solid graph) and 95 % confidence intervals (dotted graphs) for a 3-year postoperative continence are plotted against the number of prior surgeries. Probabilities are evaluated at means of covariates and reflect a patient with typical sample characteristics
Finally, operative time over surgeon’s experience is shown (after controlling for the above-mentioned covariates) in Fig. 3 (p < 0.001). A positive effect in terms of operative time saving can be shown up to the first 1000 RP. With increasing experience, operative time is reduced by 25 min from 90 min down to 65 min per RP. Beyond the threshold of approximately 1000 RP, no further influence on operative time was proven.
Discussion
Despite being challenged by a growing number of minimally invasive radical prostatectomies worldwide, the open retropubic radical prostatectomy is still a widely used definitive treatment option of localized prostate cancer in Europe [13].
Numerous studies, most of which originated from North America, focused on the influence of surgeon’s caseload on oncologic and functional outcomes as well as complication rates after radical prostatectomy. Concerning the latter, Begg et al. [6] found a significant reduction in postoperative morbidity (26 vs. 32 %, p < 0.001) as well as late urinary complications, if the radical prostatectomy was performed by a high-volume (33 or more cases) surgeon [6]. Hu et al. [7] analyzed more than 2200 radical prostatectomies and found a nearly twofold decrease in overall complications, if the radical prostatectomy was performed by a surgeon with an annual caseload of at least 40. Other studies, focusing on perioperative and urinary complications, corroborated these findings for open and minimally invasive radical prostatectomy [8, 12, 14]. Results from analyses by Vickers et al. [12] indicate that the learning curve for laparoscopic RP might be even flatter than for the open radical prostatectomy.
Surgeon’s impact on oncologic outcome is also well documented. Chun et al. [15] analyzed a single-center cohort of more than 2400 men undergoing radical prostatectomy and found the surgical volume to be a significant independent predictor of positive surgical margin rates (p < 0.001). Vickers et al. [10] included 7765 patients in a multi-institutional series and showed a strong association between surgeon’s experience and positive surgical margin rate in a multivariate analysis (p = 0.017). These findings were confirmed by Secin et al. [16] for laparoscopic radical prostatectomy. In a recent systematic review, Trinh et al. reviewed a total number of 28 studies analyzing radical prostatectomy surgeon volume and outcome. The authors concluded that increasing volume improves surgical outcome and gave preference to the hypothesis of a causal relationship between both of them [11].
In addition, there are numerous studies focusing on the annual hospital volume and its impact on general outcome after radical prostatectomy [17–19]. Trinh et al. [11] analyzed the volume–outcome relationship of 12 studies and concluded that increased hospital volume improved functional and oncologic outcomes. As it seems conclusive that high-volume surgeons practice at high-volume hospitals, these studies might possibly act as a reference for surgeon’s learning curve as well, but this implication remains to be proven.
Although the effect of the respective surgeons experience on surgical margin rate and continence rate is commonly accepted, to date there are only a few studies including subgroups of surgeons with 1000 prior cases or more [9, 10, 15, 16].
In the present study, we analyzed the impact of increasing surgical experience on negative surgical margin rates, continence rates and duration of surgical procedure within a time period of 8 years with an overall caseload of 2269. Naturally, a univariate analysis of the above-mentioned parameters would be inadequate, and oncologic as well as functional outcomes of patients have to be seen in an overall context considering tumor stage, Gleason pattern and clinical data such as age.
We documented an overall negative surgical margin in 73.3 % of all cases and 86.0 % in patients with pT2 tumor stage. This is comparable to previous literature. Chun et al. [15] found positive surgical margins in 20.2 % of 2402 patients, whereas Eastham et al. [20] found positive surgical margins in 10–48 % of 4629 men. In addition, Vesey et al. [14] analyzed a total number of 8032 patients and found 38 % positive margin rates (24 % for pT2 tumor stages). According to Vickers et al. [10], the probability of a positive surgical margin was 40 % for a low-volume surgeon (10 prior cases) and decreased to 25 % for a high-volume surgeon (250 prior cases). In this context, the limitations of the negative surgical margin rate have to be kept in mind as Vickers et al. [10] found that the negative surgical margin rate was not necessarily a strong surrogate marker for cancer control.
Analyzing the functional outcomes after radical prostatectomy, a continence rate of 94 % at 3 years postoperatively was documented. In literature, incontinence rates vary between 5 and 48 % depending on various definitions, methods of questioning patients and multiple patient factors [21–24]. In a recent study, Abdollah et al. [25] reported incontinence rates of 12 % 12 months after nerve sparing radical prostatectomy.
The presented individual learning curves of a very high-volume surgeon for both postoperative continence rates as well as negative surgical margin rates show similar findings. After a steep increase during the first 500 procedures, the slope flattens and a plateau is reached after 750 procedures which seems to be insensitive to an increasing experience of the surgeon. According to the “practice-makes-perfect” hypothesis, one could assume that according to our data, a surgeon needs at least 500–750 procedures until the results are comparable to a much more experienced surgeon with more than 2000 prior cases at this point. The shapes of the respective learning curves implicate another interesting phenomenon. The slope of the graph apparently decreases after roughly 500 (incontinence), respectively, 1000 (positive surgical margin) prior surgeries without reaching statistical significance and rises again during the final procedures (Figs. 1, 2). This might be due to a migration towards patients with unfavorable features requiring certain surgical expertise. However, as this analysis represents the learning curve of one single surgeon, no general implications can be made. The steep rise at the end of the depicted learning curve, representing a caseload of more than 2000 that indicates a possibly never ending learning curve.
When focusing on the operative time, an effect of increasing surgeon’s experience can be shown up to the first 1000 cases.
Vickers et al. [9] described a plateau for cancer control at 250 prior cases. In a recent study, the same working group reported a decrease in positive surgical margins until approximately 500 prior cases, but found wide variances of the shape of each individual learning curve. Interestingly, they failed to show a relation between the surgeon’s margin rates [10]. Regarding the laparoscopic radical prostatectomy, Secin et al. [16] found an apparent improvement in surgical margin rates up to a plateau at 200–250 surgeries.
When referring to ultra-high-volume surgeons, however, just two of 72 surgeons who were analyzed by Vickers et al. [9, 10] had a total caseload of more than 1000 previous procedures with an annual caseload of 82 and 113, respectively. Analyzing 2269 patients who underwent radical prostatectomy by one single surgeon between 2004 and 2012, the current study provides the learning curve of one single surgeon with an annual caseload of more than 280 procedures per year. To our knowledge, there is currently no study providing a comparable caseload. As indicated above, the current study is allowing an accurate predictive model of the “learning curve after the learning curve” on a wide base and consequently adds important knowledge in this certain area of research.
There are several important limitations to our study. First and foremost are the limitations inherent to retrospective analyses. Furthermore, it has to emphasize that the results of our study provide the learning curve of one single surgeon and cannot be representative for all surgeons. Thus, one has to be careful with general implications. Nevertheless, surgeons with an overall caseload of more than 2000 performed open RP are rare, and comparative studies of multiple very high-volume surgeons are difficult to realize. Moreover, information on relevant comorbidities, previous prostate surgery, adjuvant or salvage radiation treatment and nerve sparing was missing. Although characteristics of patients who provided information on continence and those who did not were comparable, a potential selection bias cannot be excluded. When describing the effects of the learning curve on operative time, it has to be stated that there is currently no evidence that a moderately decreased operative time has a measurable impact on complication rates as well as on functional and oncologic outcomes after radical prostatectomy.
We attempted to minimize well-known limitations of learning curve analysis. Opponents of the “practice-makes-perfect” hypothesis argue that there may be a selection bias with senior clinicians delegating unfavorable cases to their juniors in order not to deteriorate their own statistics [26]. In the present study, a high number of patients with high-risk tumor stages are included; thus, a selection bias is at least unlikely. Despite the recently reported disadvantages of predefined cutoff values [27], they are routinely used in multicentre studies due to presentation issues. Focusing on one single very high-volume surgeon, defining cutoff values for comparison reasons is not required. During the analyzed period of time (2004–2012), no fundamental changes in operation technique were introduced, reducing a potential mix of effects (learning curve vs. change in operation technique, as described by Vickers et al. [28]) to a minimum level.
Conclusions
Surgical experience has a strong positive impact on pathologic and functional outcomes as well as on operative time even in very high-volume surgeons. The learning effect concerning operative time was even detectable up to a threshold of almost 1000 RP. Despite its limitations, our single-center study provides insights into a potentially representative progress of the learning curve during 2269 procedures and documents that the learning curve is long and may never end.
References
Guillonneau BD, Fizazi K (2011) Natural history of patients presenting biochemical recurrence after radical prostatectomy: some good news? Eur Urol 59:900–901
Simmons MN, Stephenson AJ, Klein EA (2007) Natural history of biochemical recurrence after radical prostatectomy: risk assessment for secondary therapy. Eur Urol 51:1175–1184
Boorjian SA, Thompson RH, Tollefson MK et al (2011) Long-term risk of clinical progression after biochemical recurrence following radical prostatectomy: the impact of time from surgery to recurrence. Eur Urol 59:893–899
Herrell SD, Smith JA Jr (2005) Robotic-assisted laparoscopic prostatectomy: What is the learning curve? Urology 66:105–107
Artibani W, Novara G (2008) Cancer-related outcome and learning curve in retropubic radical prostatectomy: “if you need an operation, the most important step is to choose the right surgeon”. Eur Urol 53:874–876
Begg CB, Riedel ER, Bach PB et al (2002) Variations in morbidity after radical prostatectomy. N Engl J Med 346:1138–1144
Hu JC, Gold KF, Pashos CL et al (2003) Role of surgeon volume in radical prostatectomy outcomes. J Clin Oncol 21:401–405
Bianco FJ Jr, Riedel ER, Begg CB et al (2005) Variations among high volume surgeons in the rate of complications after radical prostatectomy: further evidence that technique matters. J Urol 173:2099–2103
Vickers AJ, Bianco FJ, Serio AM et al (2007) The surgical learning curve for prostate cancer control after radical prostatectomy. J Natl Cancer Inst 99:1171–1177
Vickers A, Bianco F, Cronin A et al (2010) The learning curve for surgical margins after open radical prostatectomy: implications for margin status as an oncological end point. J Urol 183:1360–1365
Trinh QD, Bjartell A, Freedland SJ et al (2013) A systematic review of the volume-outcome relationship for radical prostatectomy. Eur Urol 64:786–798
Vickers AJ, Savage CJ, Hruza M et al (2009) The surgical learning curve for laparoscopic radical prostatectomy: a retrospective cohort study. Lancet Oncol 10:475–480
Wallerstedt A, Tyritzis SI, Thorsteinsdottir T et al (2014) Short-term results after robot-assisted laparoscopic radical prostatectomy compared to open radical prostatectomy. Eur Urol 67:660–670
Vesey SG, McCabe JE, Hounsome L et al (2012) UK radical prostatectomy outcomes and surgeon case volume: based on an analysis of the British Association of Urological Surgeons Complex Operations Database. BJU Int 109:346–354
Chun FK, Briganti A, Antebi E et al (2006) Surgical volume is related to the rate of positive surgical margins at radical prostatectomy in European patients. BJU Int 98:1204–1209
Secin FP, Savage C, Abbou C et al (2010) The learning curve for laparoscopic radical prostatectomy: an international multicenter study. J Urol 184:2291–2296
Van Poppel H, Collette L, Kirkali Z et al (2001) Quality control of radical prostatectomy: a feasibility study. Eur J Cancer 37:884–891
Ellison LM, Heaney JA, Birkmeyer JD (2000) The effect of hospital volume on mortality and resource use after radical prostatectomy. J Urol 163:867–869
Yao SL, Lu-Yao G (1999) Population-based study of relationships between hospital volume of prostatectomies, patient outcomes, and length of hospital stay. J Natl Cancer Inst 91:1950–1956
Eastham JA, Kattan MW, Riedel E et al (2003) Variations among individual surgeons in the rate of positive surgical margins in radical prostatectomy specimens. J Urol 170:2292–2295
Peyromaure M, Ravery V, Boccon-Gibod L (2002) The management of stress urinary incontinence after radical prostatectomy. BJU Int 90:155–161
Mettlin CJ, Murphy GP, Sylvester J et al (1997) Results of hospital cancer registry surveys by the American College of Surgeons: outcomes of prostate cancer treatment by radical prostatectomy. Cancer 80:1875–1881
Catalona WJ, Basler JW (1993) Return of erections and urinary continence following nerve sparing radical retropubic prostatectomy. J Urol 150:905–907
Hautmann RE, Sauter TW, Wenderoth UK (1994) Radical retropubic prostatectomy: morbidity and urinary continence in 418 consecutive cases. Urology 43:47–51
Abdollah F, Sun M, Suardi N et al (2013) A novel tool to assess the risk of urinary incontinence after nerve-sparing radical prostatectomy. BJU Int 111:905–913
Nuttall M, Cathcart P, van der Meulen J et al (2005) A description of radical nephrectomy practice and outcomes in England: 1995–2002. BJU Int 96:58–61
Bennette C, Vickers A (2012) Against quantiles: categorization of continuous variables in epidemiologic research, and its discontents. BMC Med Res Methodol 12:21
Vickers AJ, Cronin AM, Masterson TA et al (2010) How do you tell whether a change in surgical technique leads to a change in outcome? J Urol 183:1510–1514
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
All patients gave their informed consent prior to data collection. The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Alexander Kretschmer and Philipp Mandel have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kretschmer, A., Mandel, P., Buchner, A. et al. Surgical learning curve for open radical prostatectomy: Is there an end to the learning curve?. World J Urol 33, 1721–1727 (2015). https://doi.org/10.1007/s00345-015-1540-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1540-5