Abstract
Purpose
Physical activity and body mass index (BMI) are involved in prostate cancer etiology; possible biologic mechanisms include their effects on hormonal levels. Our aim was to investigate the relationship between physical activity, obesity, and prostate cancer.
Methods
We followed a cohort of 13,109 Swedish men for 13 years and investigated the association of self-reported physical activity and BMI at baseline with prostate cancer incidence. We further analyzed whether BMI could modulate effects of physical activity. Occupational, recreational, and total physical activity were analyzed in relation to overall, localized, and advanced prostate cancer.
Results
During the study follow-up, we observed a total of 904 cases of prostate cancer (429 localized, 407 advanced, and 68 unclassified). High levels of occupational physical activity were associated with a nonsignificantly decreased risk of overall (HR 0.81, 95 % CI 0.61–1.07), localized (HR 0.75, 95 % CI 0.51–1.12), and advanced (HR 0.85, 95 % CI 0.55–1.31) prostate cancer. We found no association between high BMI and risk of prostate cancer incidence: We observed, however, a significant interaction between BMI and leisure physical activity.
Conclusion
No association was confirmed between total physical activity and localized or advanced prostate cancer. The highest, relative to the lowest, level of occupational physical activity tended to be linked to a lower risk of prostate cancer, with a suggested dose–response relationship. We found no association between high BMI and risk of prostate cancer incidence; however, our analyses suggested an interaction between BMI and physical activity during recreational time that merits further investigation in future studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A causal association between high levels of physical activity and reduced risk of colon and breast cancer has become increasingly well established [1, 2]; some studies even suggest that physical activity might improve the clinical outcome following diagnosis [3]. A large prospective cohort study conducted on 293,902 men has shown no relationship between physical activity and risk of prostate cancer [4]. However, the epidemiologic evidence on physical activity before diagnosis and prostate cancer is inconsistent with no obvious biologic mechanism supporting a causal association. Besides physical activity, the role of body mass index (BMI) and other anthropometric measures has been investigated. Despite several studies have reported a positive association between obesity and risk of death from prostate cancer [5], the overall evidence is still inconclusive.
Only large, well-designed prospective studies can advance our understanding of the association between physical activity, obesity, and prostate cancer. If causal associations do indeed exist, this would provide a realistic opportunity for primary prevention of this dominating malignancy. We therefore analyzed a large Swedish cohort of men with detailed exposure assessment and follow-up during 13 years.
Materials and methods
Study cohort
In 1997, the Swedish Cancer Society organized a four-day national fund raising event in almost 3,600 cities and villages all around the country. In conjunction with this, the Swedish National March Cohort was established. Participants were expected to be particularly motivated to provide valid information. They filled out a 32-page questionnaire with detailed questions about physical activity, anthropometric measures, and wide variety of other background factors. The availability of individually unique national registration numbers assigned to all Swedish residents permitted accurate follow-up of health status through continuously updated nationwide databases. In total, 43,863 subjects returned a completed questionnaire. Our initial cohort comprised 15,662 men. After linkage to the Swedish registries of total population, migration, death, and cancer, we excluded subjects who reported an incorrect national registration number (n = 6), had a history of cancer (n = 868), emigrated before the start of follow-up (n = 148), or were below the age of 20 years at the beginning of follow-up (n = 1,550). The final cohort used in the analyses consisted of 13,109 men. The study was approved by the Research Ethics Review Committee at the Karolinska Institutet. All subjects provided informed consent.
Baseline measures
Exposure and covariate data were based on self-reported information collected in the questionnaire given at cohort enrollment. Physical activity was estimated using the validated energy expenditure questionnaire (EEQ) [6, 7]. The EEQ comprises nine physical activity steps grading physical activity according to intensity levels, and an estimated value of metabolic energy turnover (MET) was assigned to each activity level. One MET is equivalent to an energy expenditure of 1 kcal/kg body weight per hour [7]. Participants reported the time spent on each intensity level during a typical day and night over the previous 12 months. Hence, the total physical activity time reported allowed estimating a total amount of MET-hours per day (MET-h/day) [6].
Occupational physical activity was assessed through the question “How physically demanding has your daily occupation been during the past 12 months?” with four possible answers (“light, mostly sedentary,” “light, but I have moved a little,” “rather strenuous,” and “very strenuous”). Information on muscular/locomotive activity during working hours was also collected. To assess leisure physical activity, participants were asked to report the average weekly time spent on different exercise/outdoor life activities, for example, jogging or swimming, in the previous 12 months. Moreover, participants were asked about average weekly time spent in household and commuting. Each activity was assigned a MET value; hence, leisure physical activity time was calculated as an average of MET-h per day. Number of hours spent in light-, moderate-, and high-intensity leisure physical activities was also computed.
The questionnaire included questions on weight, height, alcohol consumption, smoking status, educational level, and medical history, including diagnosis of diabetes. BMI was computed as weight divided by height squared (kg/m2). No information on family history of prostate cancer was collected.
Percentages of missing values were 12 % for total physical activity, 1 % for occupation physical activity, 1 % for leisure physical activity, and 4 % for BMI. For covariates, percentages were 10 % for smoking, 5 % for diabetes, and less than 1 % for education and alcohol consumption.
The National Prostate Cancer Register (NPCR) of Sweden
A prostate cancer register was established in Sweden in 1987, and coverage became nationwide in 1998. At the time of diagnosis, the NPCR collects information on tumor stage according to the TNM (T, tumor size; N, involvement of lymph nodes; and M, presence of distant metastasis) classification system, Gleason tumor grade, and prostate-specific antigen level (PSA) [8]. A total of 98 % of all diagnosed prostate cancers found in the Swedish National Cancer Register were also found in NPCR.
We defined cancers with a clinical T1–2 stage, Gleason sum score lower or equal to seven and serum PSA lower or equal to 20 ng/ml as localized cancers. Subjects meeting one or more of the following criteria at diagnosis were classified as having advanced cancers: T3 or higher, Gleason sum score higher than seven, serum PSA higher than 20 ng/ml, lymph node involvement, and/or presence of distant metastases.
Follow-up
The cohort was followed through record linkages from October 1, 1997, to December 31, 2010. Follow-up ended at the time of prostate or other cancer diagnosis, death, emigration, or December 31, 2010, whichever occurred first. We obtained information on cancer occurrence through linkage with the Swedish National Cancer Register. Clinical data on diagnosed prostate cancers were available through linkage with the NPCR. Men diagnosed only at death and having prostate cancer as main cause of death were included in the analysis. Mortality data were obtained from the Swedish Death Register.
Statistical analyses
We categorized total physical activity in MET-h/day into low, medium, and high levels by dividing the distribution into tertiles, with cutoffs at 34.34 and 45.17 MET-h/day, and occupational physical activity into “light,” “some movement,” and “strenuous,” combining “rather strenuous” and “very strenuous” into one category. We created binary variables (low/high) for muscular and locomotive activity during working hours. Leisure physical activity was categorized into low, medium, and high levels by creating tertiles of the distribution, with cutoffs at 3.25 and 5.54 MET-h/day. BMI was categorized according to the WHO cutoffs: normal weight (<25 kg/m2), overweight (≥25; <30 kg/m2), and obese (≥30 kg/m2).
We used Cox proportional hazards regression models with age as underlying time scale to estimate hazard ratios (HRs) and 95 % confidence intervals (95 % CI) of prostate cancer incidence at different levels of BMI, occupational, leisure time, and total physical activity. Normal BMI and low physical activity were the reference categories. Ties were handled using the Breslow method. We tested the proportional hazards assumption by using Schoenfeld’s residuals. The potential interaction with age was assessed by stratifying the analyses on age (≤70, >70), where each subject could contribute person-years at risk to one or both of these groups. Statistical significance of interaction with age was tested with the likelihood ratio test. Cox models were adjusted for alcohol drinking (nondrinkers, light drinkers, and heavy drinkers), smoking status (non-smokers, former smoker, and current smoker), level of education (≤12 and >12 years), and diabetes (yes/no); all estimates were also implicitly adjusted by age, the underlying time scale.
Linear trends of HRs were tested by using the median value of each category (for total and leisure physical activity, and BMI) or the category level (for occupational physical activity) as a numerical variable in the Cox regression model. We assessed multiplicative interaction between occupational and leisure time and total physical activity and BMI, by including the cross-product interaction terms with the main effect terms. Statistical significance of interaction was assessed through the likelihood ratio test. In addition, we tested additive interaction using relative excess risk due to interaction (RERI), after dichotomizing the previous variables [9]. To explore potential nonlinear dose–response relations, we modeled BMI and both total and leisure physical activity as continuous variables through restricted cubic splines. In a sensitivity analysis to assess potential reverse causality bias, we excluded the first two years of follow-up because physical inactivity potentially could be related to subclinical disease.
All statistical analyses were performed with Stata version 13.1 (Stata Corporation, College Station, TX, USA). All reported P values were two sided. P values <0.05 were considered statistically significant.
Results
During the study follow-up, we identified 904 incident cases of prostate cancer (429 localized, 407 advanced, and 68 unclassified). Of these, 133 died of prostate cancer during the follow-up period. The demographic characteristics of the cohort are shown in Table 1. At baseline, men with higher levels of total physical activity were more likely to be younger, less educated, and less likely to have diabetes, to smoke, and to have a high intake of alcohol compared with men with lower physical activity. Normal-weight men were more educated, more physically active, and less likely to have diabetes or to have ever smoked than overweight and obese men.
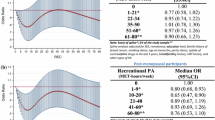
While there was no significant association between prostate cancer incidence and total physical activity, we noted an inverse trend with occupational physical activity (Table 2). Although short of statistical significance, this trend was observed for overall, localized, and advanced prostate cancer. When we analyzed occupational physical activity separately for muscular or locomotion activity, an inverse nonsignificant association was observed between muscular activity and overall (HR 0.80, 95 % CI 0.60–1.06), localized (HR 0.78, 95 % CI 0.52–1.18), and advanced (HR 0.81, 95 % CI 0.52–1.25) prostate cancer. We found no significant association of leisure physical activity on prostate cancer risk (Table 2). When we analyzed the effect of light-, moderate-, and high-intensity leisure physical activities, modeled as continuous variables, no significant associations were found (data not shown).
We found little evidence that BMI is associated with prostate cancer incidence (data not shown). To further explore possible nonlinear relations, we used restricted cubic splines, separately for overall, localized, and advanced prostate cancer. We found some evidence of an inverse U-shaped relation for localized, but not advanced prostate cancer (data not shown). We did not find evidence of deviation from the proportionality assumption, and when computing age-specific HR, no statistically significant differences were observed (data not shown).
No statistically significant interactions were found between occupational physical activity and BMI, whether on multiplicative or on additive scale. However, when we stratified on different levels of BMI, obese men exhibited a slightly stronger inverse association of occupational physical activity with both overall (second tertile HR 0.55, 95 % CI 0.23–1.31; third tertile HR 0.53, 95 % CI 0.18–1.63) and localized (second tertile HR 0.25, 95 % CI 0.08–0.79; third tertile HR 0.18, 95 % CI 0.03–0.95) prostate cancer incidence. A significant multiplicative interaction between leisure physical activity and BMI was found in the model for overall prostate cancer (P value = 0.043): In obese men, high levels of physical activity were associated with higher risks of developing prostate cancer (second tertile HR 1.33, 95 % CI 0.54–3.27; third tertile HR 2.42, 95 % CI 1.06–5.56).
After excluding the first two years of follow-up, results remained essentially unchanged (data not shown).
Discussion
In this large prospective cohort study, we found that prostate cancer incidence was not significantly associated with total physical activity. Although the incidence rates were larger in the highest occupational physical activity level than in the lower level, the difference was not statistically significant. Also, BMI did not appear to be an independent risk factor for prostate cancer; however, our analyses suggest that it may potentially modify the association between recreational physical activity and total prostate cancer.
Several studies have investigated the relationship between physical activity and prostate cancer risk [10–18], but their results were either inconclusive or inconsistent across the studies. Some highlighted a protective role of physical activity [10–12] even if most of them reported small effect sizes [19]. On the contrary, other studies did not show any significant associations [13, 14]. Many studies highlighted an inverse association between occupational physical activity and prostate cancer [12, 15]. Our results seem to support previous findings of such an association, with a noteworthy inverse trend for localized prostate cancer incidence [12].
The association between leisure time physical activity and prostate cancer risk has been extensively investigated [11, 20]. The evidence accumulated so far suggests a small association, if any at all. A recent meta-analysis, including 88,294 prostate cancer cases, revealed a risk ratio of 0.95 (P value = 0.07) when comparing the highest versus lowest levels of recreational physical activity [21].
Obesity has been found to be potentially associated with both risk and progression of prostate cancer, since BMI could affect hormonal and metabolic pathways involved in the disease [22, 23]. In particular, there is evidence of a positive association between high BMI and aggressive prostate cancer as well as higher prostate cancer mortality [5, 24, 25] and a negative association with localized cancer [24, 26]. To explain these relationships, it had been suggested that PSA testing and digital rectal examination result in lower biopsy rates among obese compared with normal-weight men, possibly leading to lower number of diagnosed cases in pre-advanced phase [27]. However, findings from a recent study showed that obesity increases risk of high-grade prostate cancer and decreases risk of low-grade cases, independently of PSA levels [27]. Our results did not indicate any direct association, but showed an inverse U-shaped relationship between BMI and localized prostate cancer incidence, as previously found by Discacciati et al. [26] in a cohort of 36,959 Swedish men.
Among obese men, occupational physical activity might have a greater protective impact on localized prostate cancer risk than among normal and overweight subjects, although confounding by lower diagnostic intensity and less PSA-testing could explain this finding. Localized prostate cancers are increasingly being discovered through PSA screening which is associated with socioeconomic status [28]. Educational level is a proxy for socioeconomic status, and in our study population, low educational level was associated with obesity.
Our results suggested that high levels of leisure physical activity may significantly increase risk of localized prostate cancer among obese men. This finding is not easy to interpret. However, differential effects of exercise in normal-weight and obese men were found in other large studies [18, 29].
Our study has several strengths, including its prospective design, high-quality exposure data, and a large sample size. We minimized misclassification of the outcome through exact linkages to essentially complete high-quality national registries using individually unique national registration numbers. The large sample size ensured adequate statistical power for our tests.
A limitation of this study is that both BMI and physical activity were determined from self-reported data, with a possibility of misclassification of exposures. Another potential limitation is that we only have baseline lifestyle assessment which could potentially dilute an effect if activity changes over time and patients are misclassified. However, in the same cohort, we documented a convincing, statistically significant inverse dose–response relationship between physical activity and risk of breast cancer, giving support to the validity of both our data and approach [30].
Our analyses are based on a large prospective study with meticulous exposure assessment and complete follow-up with detailed clinical information on disease stage and grade. The results, however, do not provide conclusive evidence of an association between physical activity, BMI, and overall prostate cancer risk.
References
Friedenreich CM, Orenstein MR (2002) Physical activity and cancer prevention: etiologic evidence and biological mechanisms. J Nutr 132(11 Suppl.):3456S–3464S
Courneya KS, Friedenreich CM (2007) Physical activity and cancer control. Semin Oncol Nurs 23(4):242–252. doi:10.1016/j.soncn.2007.08.002
Kenfield SA, Stampfer MJ, Giovannucci E, Chan JM (2011) Physical activity and survival after prostate cancer diagnosis in the health professionals follow-up study. J Clin Oncol 29(6):726–732. doi:10.1200/jco.2010.31.5226
Moore SC, Peters TM, Ahn J, Park Y, Schatzkin A, Albanes D, Ballard-Barbash R, Hollenbeck A, Leitzmann MF (2008) Physical activity in relation to total, advanced, and fatal prostate cancer. Cancer Epidemiol Biomark Prev 17(9):2458–2466. doi:10.1158/1055-9965.epi-08-0403
Häggström C, Stocks T, Ulmert D, Bjørge T, Ulmer H, Hallmans G, Manjer J, Engeland A, Nagel G, Almqvist M, Selmer R, Concin H, Tretli S, Jonsson H, Stattin P (2012) Prospective study on metabolic factors and risk of prostate cancer. Cancer 118(24):6199–6206. doi:10.1002/cncr.27677
Lagerros YT, Bellocco R, Adami H-O, Nyrén O (2009) Measures of physical activity and their correlates: the Swedish National March Cohort. Eur J Epidemiol 24(4):161–169. doi:10.1007/s10654-009-9327-x
Lagerros YT, Mucci LA, Bellocco R, Nyrén O, Bälter O, Bälter KA (2006) Validity and reliability of self-reported total energy expenditure using a novel instrument. Eur J Epidemiol 21(3):227–236. doi:10.1007/s10654-006-0013-y
Van Hemelrijck M, Wigertz A, Sandin F, Garmo H, Hellström K, Fransson P, Widmark A, Lambe M, Adolfsson J, Varenhorst E, Johansson E, Stattin P, NPCR F, Sweden P (2013) Cohort profile: the national prostate cancer register of Sweden and prostate cancer data base Sweden 2.0. Int J Epidemiol 42(4):956–967. doi:10.1093/ije/dys068
Knol MJ, van der Tweel I, Grobbee DE, Numans ME, Geerlings MI (2007) Estimating interaction on an additive scale between continuous determinants in a logistic regression model. Int J Epidemiol 36(5):1111–1118. doi:10.1093/ije/dym157
Clarke G, Whittemore AS (2000) Prostate cancer risk in relation to anthropometry and physical activity: the National Health and Nutrition Examination Survey I Epidemiological Follow-Up Study. Cancer Epidemiol Biomark Prev 9(9):875–881
Patel AV, Rodriguez C, Jacobs EJ, Solomon L, Thun MJ, Calle EE (2005) Recreational physical activity and risk of prostate cancer in a large cohort of US men. Cancer Epidemiol Biomark Prev 14(1):275–279
Orsini N, Bellocco R, Bottai M, Pagano M, Andersson SO, Johansson JE, Giovannucci E, Wolk A (2009) A prospective study of lifetime physical activity and prostate cancer incidence and mortality. Br J Cancer 101(11):1932–1938
Lee IM, Sesso HD, Paffenbarger RS Jr (2001) A prospective cohort study of physical activity and body size in relation to prostate cancer risk (United States). Cancer Causes Control 12(0957-5243 SB - IM):187–193
Lagiou A, Samoli E, Georgila C, Minaki P, Barbouni A, Tzonou A, Trichopoulos D, Lagiou P (2008) Occupational physical activity in relation with prostate cancer and benign prostatic hyperplasia. Eur J Cancer Prev 17(1473-5709 (Electronic)):336–339
Norman A, Moradi T, Gridley G, Dosemeci M, Rydh B, Nyren O, Wolk A (2002) Occupational physical activity and risk for prostate cancer in a nationwide cohort study in Sweden. Br J Cancer 86(1):70–75. doi:10.1038/sj.bjc.6600023
Nilsen TIL, Romundstad PR, Vatten LJ (2006) Recreational physical activity and risk of prostate cancer: a prospective population-based study in Norway (the HUNT study). Int J Cancer 119(12):2943–2947. doi:10.1002/ijc.22184
Krishnadasan A, Kennedy N, Zhao Y, Morgenstern H, Ritz B (2008) Nested case–control study of occupational physical activity and prostate cancer among workers using a job exposure matrix. Cancer Causes Control 19(1):107–114. doi:10.1007/s10552-007-9076-7
Wiklund F, Lageros YT, Chang E, Bälter K, Johansson J-E, Adami H-O, Grönberg H (2008) Lifetime total physical activity and prostate cancer risk: a population-based case–control study in Sweden. Eur J Epidemiol 23(11):739–746. doi:10.1007/s10654-008-9294-7
Young-McCaughan S (2012) Potential for prostate cancer prevention through physical activity. World J Urol 30:167–179. doi:10.1007/s00345-011-0812-y
Johnsen NF, Tjønneland A, Thomsen BL, Christensen J, Loft S, Friedenreich C, Key TJ, Allen NE, Lahmann PH, Mejlvig L, Overvad K, Kaaks R, Rohrmann S, Boing H, Misirli G, Trichopoulou A, Zylis D, Tumino R, Pala V, Bueno-de-Mesquita HB, Kiemeney LA, Suarez LR, Gonzalez CA, Sanchez MJ, Huerta JM, Gurrea AB, Manjer J, Wirfalt E, Khaw KT, Wareham N, Boffetta P, Egevad L, Rinaldi S, Riboli E (2009) Physical activity and risk of prostate cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Int J Cancer 125(4):902–908. doi:10.1002/ijc.24326
Liu Y, Hu F, Li D, Wang F, Zhu L, Chen W, Ge J, An R, Zhao Y (2011) Does physical activity reduce the risk of prostate cancer? A systematic review and meta-analysis. Eur Urol 60:1029–1044. doi:10.1016/j.eururo.2011.07.007
Bonn S, Wiklund F, Sjölander A, Szulkin R, Stattin P, Holmberg E, Grönberg H, Bälter K (2014) Body mass index and weight change in men with prostate cancer: progression and mortality. Cancer Causes Control 25(8):933–943. doi:10.1007/s10552-014-0393-3
Cao Y, Ma J (2011) Body mass index, prostate cancer–specific mortality, and biochemical recurrence: a systematic review and meta-analysis. Cancer Prev Res 4(4):486–501. doi:10.1158/1940-6207.capr-10-0229
Wright ME, Chang S-C, Schatzkin A, Albanes D, Kipnis V, Mouw T, Hurwitz P, Hollenbeck A, Leitzmann MF (2007) Prospective study of adiposity and weight change in relation to prostate cancer incidence and mortality. Cancer 109(4):675–684. doi:10.1002/cncr.22443
Rodriguez C, Freedland SJ, Deka A, Jacobs EJ, McCullough ML, Patel AV, Thun MJ, Calle EE (2007) Body mass index, weight change, and risk of prostate cancer in the Cancer Prevention Study II Nutrition Cohort. Cancer Epidemiol Biomark Prev 16(1):63–69. doi:10.1158/1055-9965.EPI-06-0754
Discacciati A, Orsini N, Andersson SO, Andrén O, Johansson JE, Wolk A (2011) Body mass index in early and middle-late adulthood and risk of localised, advanced and fatal prostate cancer: a population-based prospective study. Br J Cancer 105(7):1061–1068. doi:10.1038/bjc.2011.319
Vidal AC, Howard LE, Moreira DM, Castro-Santamaria R, Andriole GL, Freedland SJ (2014) Obesity increases the risk for high-grade prostate cancer: results from the REDUCE study. Cancer Epidemiol Biomark Prev. doi:10.1158/1055-9965.epi-14-0795
Holmberg L (2013) Obesity, nutrition, and prostate cancer: insights and issues. Eur Urol 63(5):821–822. doi:10.1016/j.eururo.2013.01.033
Zeegers MPA, Dirx MJM, van den Brandt PA (2005) Physical activity and the risk of prostate cancer in the Netherlands cohort study, results after 9.3 years of follow-up. Cancer Epidemiol Biomark Prev 14(6):1490–1495. doi:10.1158/1055-9965.epi-04-0771
Bellocco R, Marrone G, Weimin Y, Nyrén O, Adami H-O, Mariosa D, Lagerros YT Prospective study of physical activity, anthropometric measures and risk of post-menopausal breast cancer. (in preparation)
Acknowledgments
The authors express sincere gratitude to the Swedish Cancer Society and volunteers who worked with the National March. Furthermore, the authors thank Andrea Discacciati, Stephanie Bonn, Hatef Darabi, and Andrea Ganna for their useful comments on the manuscript. This work was supported by ICA AB, Telefonaktiebolaget LM Ericsson, the Swedish Cancer Society (Grant CAN 2012/591), Karolinska Institutet Distinguished Professor Award (H-OA Grant 2368/10-221), Minister of University and Research, Italy (RB Grant PRIN 2009 X8YCBN), and the regional agreement on medical training and clinical research between Stockholm County Council and Karolinska Institutet (YTL). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
This study was approved by Regional Ethics Review Board at the Karolinska Institutet.
Author information
Authors and Affiliations
Corresponding author
Additional information
Rino Bellocco and Ylva Trolle Lagerros have contributed equally to the work and are listed alphabetically.
Rights and permissions
About this article
Cite this article
Grotta, A., Bottai, M., Adami, HO. et al. Physical activity and body mass index as predictors of prostate cancer risk. World J Urol 33, 1495–1502 (2015). https://doi.org/10.1007/s00345-014-1464-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-014-1464-5