Abstract
Purpose
To assess the effectiveness of acupuncture in treating female adult with overactive bladder.
Materials and methods
After we excluded other causes for storage symptoms, a total of 240 consecutive female patients with overactive bladder were enrolled and completed all aspects of this prospective randomized controlled trial, of which 118 cases were randomly assigned to receive a weekly acupuncture treatment (intervention group), while the other 122 cases were given a pharmacological treatment of oral tolterodine tartrate 2 mg twice daily (control group) for 4 weeks. Data on urgency, incontinence, micturition frequency, nocturia episodes and voided volume were collected and statistically analyzed before and after 4 weekly acupuncture treatments or 4 weeks’ pharmacological treatment using a 3-day micturition diary.
Results
The two groups of female patients with overactive bladder were given treatment with weekly acupuncture (n = 118), oral tolterodine tartrate (n = 122) for 4 weeks respectively. At weeks 4, subjects in both intervention and control groups had significant decreases in number of urinary urgency episodes, incontinence episodes, daytime frequency, nocturia episodes and increase in volume voided per micturition without a significant difference in the changes of overactive bladder symptoms between the groups. There were no serious adverse events during the study.
Conclusions
This randomized controlled trial demonstrates that acupuncture is safe with significant improvements in patient assessment of overactive bladder symptoms and may be considered a clinically alternative treatment for overactive bladder in female adult.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overactive bladder (OAB) is chronic condition that significantly affects quality of life in patients. It is defined as urgency, with or without urgency incontinence, usually with frequency and nocturia [1]. Urgency incontinence is the complaint of involuntary leakage accompanied by or immediately preceded by urgency. Urgency is the complaint of a sudden compelling desire to pass urine which is difficult to defer. Daytime frequency is the individual’s perception of urinating too often by day. Nocturia is the complaint that the individual has to wake at night one or more times to void. Based on the National Overactive Bladder Evaluation (NOBLE) study, the prevalence of OAB was 16.9 % in women in the USA and rose with age [2]. The cost of OAB is a substantial economic and human burden. The estimated average annual direct cost of OAB per patient ranged between €262 in Spain and €619 in Sweden. The estimated total direct cost burden for OAB per country ranges between €333 million in Sweden and €1.2 billion in Germany [3]. The symptoms of OAB have many potential causes and contributing factors, including lower urinary tract and neurologic conditions. Research focus has particularly concentrated on abnormalities of afferent signaling and mechanisms underlying detrusor overactivity, the former as the presumed basis of urgency, the latter as it is likely to contribute in a large number of people with OAB. OAB affects patients’ overall quality of life, causing depression and emotional distress, which in turn exacerbate symptoms of OAB. The management of OAB includes both behavioral modification and pharmacological methods [4]. Antimuscarinic agents, such as tolterodine, are the mainstay of pharmacological treatment of OAB. Tolterodine has been the active comparator in a number of studies. In clinical practice, it remains an effective and well-tolerated management option for patients with OAB, with less and mild adverse events, such as dry mouth, constipation, headache, nausea, blurred vision, dizziness and acute urinary retention. Dry mouth was the only adverse event that occurred significantly more often in patients treated with tolterodine in comparison with the placebo group in some studies [5, 6]. However, current available therapy for OAB is only partially effective and has some significant side effects [7, 8]. Some data support acupuncture as a potential treatment for female patients with OAB [9–11]. The scientific literature about acupuncture for OAB is increasing; however, in general, there are few large randomized controlled trials supporting acupuncture as a potentially successful treatment of OAB. The efficacy of acupuncture needs to be assessed critically to inform clinical practice and guides the continued search for new treatment regimens. The purpose of this trial was to investigate the effectiveness of acupuncture for OAB in female adult in a randomized controlled study, advancing the strategies for medical management of OAB.
Materials and methods
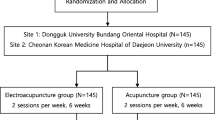
The study design was a randomized, control trial comparing weekly acupuncture with twice daily 2 mg tolterodine tartrate for the treatment of OAB in female adult. The study was approved by the local ethical committees (Dujiangyan Medical Center Ethics Committee) and was performed with the patients’ written informed consent. The authors confirmed that all related trials for this intervention are registered, and the clinical trial design is posted at http://www.chictr.org/cn/ (ID: ChiCTR-TRC-14005243). The study was conducted by urologists, physicians of Traditional Chinese Medicine and registered nurse practitioners at Dujiangyan Medical Center. We prospectively collected 272 consecutive female patients who presented with any chief complaint suggestive of OAB between July 1, 2010 and March 1, 2014, from the inpatient department and outpatient clinic of Dujiangyan Medical Center. In total, 240 patients completed all aspects of this study and were followed up (Fig. 1).
Inclusion and exclusion criteria
Women aged over 18 years old who have urinary urgency and nocturia with or without urgency incontinence or frequency for at least 6 months were included in this study. For the study, urgency was defined as the complaint of a sudden compelling desire to pass urine, which is difficult to defer. Urinary frequency is the complaint by the patient who considers that he/she voids too often by day. Nocturia is defined as the need to wake one or more times per night to void. Urgency incontinence is the complaint of involuntary leakage accompanied by or immediately preceded by urgency [1]. Exclusion criteria included the following: urinary tract infections, interstitial cystitis, polyuria, bladder tumor and underlying neurologic abnormalities (e.g., neuropathic bladder). Women who were taking medications for OAB or receiving acupuncture for any condition were excluded. Furthermore, women were also excluded if they were pregnant, recently gave birth (i.e., within 6 months preceding the referral), had previous prolapse or incontinence surgery, or not beginning sexual activities (due to ethics problems) were excluded from this study.
Study protocol and statistics
At enrollment, all the subjects were evaluated with medical, surgical, obstetric and gynecologic history, 3-day micturition diary, targeted physical examination and urinalysis. If necessary, cystoscopy, urodynamics or videourodynamics were performed to exclude other conditions causing OAB symptoms. The registered nurses on duty in the urological wards, outpatient clinic randomly assigned the enrolled patients to the weekly acupuncture treatment group (intervention) or the twice daily 2 mg tolterodine tartrate treatment group at admission or first referral, using a concealed allocation sequence. A computer-generated list of random numbers was used, and the allocation sequence was concealed in sequentially numbered, sealed and opaque envelopes by a doctor who did not participate in group assignment, data collection or statistical analysis. Envelopes were opened sequentially only after participant details had been written on the envelope. Blinding of the group assignment for the nurses and patients was not possible, but in this study, the data collection, processing and analysis were conducted by other doctors who did not participate in group assignment. What is more, the doctors who made the diagnosis of OAB and recruited the subjects did not also participate in group assignment, patients’ treatments, and data analysis. We chose the following needles insertion points for acupuncture treatment in intervention group: SP6 (Spleen Meridian, Sanyinjiao), SP9 (Spleen Meriian, Yinlingquan), KI3 (Kidney Meridian, Taixi), and CV4 (Conception Vessel, Guanyuan). SP6 is located on the tibial aspect of the leg, posterior to the medial border of the tibia, 3 cun superior to the prominence of the medial malleolus. SP9 is located in a depression at the angle formed by the inferior border of the medial condyle of the tibia and the posterior border of the tibia. KI3 is located in the depression between the medial malleolus and tendo calcaneus, at the level with the tip of the medial malleolus. CV4 is located on the midline of the abdomen, 3 cun below the umbilicus. Sterile disposable stainless steel acupuncture filiform needles (size 0.35 mm × 50 mm, Huatuo Brand, manufactured by Suzhou Medical Appliance, China) were used for the study. The patients were laid in the supine position. All acupuncture points were prepared with 75 % alcohol pads. Needles were inserted vertically 1–1.5 cm in depth and placed bilaterally at these points and rotated clockwise until the patient experienced Deqi, a characteristic sensation of numbness, soreness or slight pain [12], then were left in place without further stimulation for 20 min [13]. The acupuncture treatment was performed by licensed acupuncturists with more than 10 years’ experience as registered Traditional Chinese Medicine practitioners. The patients in control group received a treatment of oral tolterodine tartrate 2 mg, twice daily. Besides these, the patients did not receive any treatment education about behavioral changes for OAB. After 4 weeks’ treatment, all the enrolled subjects were asked to complete a 3-day micturition diary. Data on urgency, urgency incontinence, daytime micturition frequency, nocturia episodes and voided volume were collected. Subjects enrolled in the study were encouraged to report adverse events.
The primary outcomes involved the changes of urinary urgency, incontinence, daytime frequency, nocturia episodes and voided volume at the fourth week; while the secondary outcomes included the changes of voiding symptoms if any. Safety evaluation included some adverse events during and after acupuncture treatment, such as bruising and bleeding, acupuncture needle site pain/sensation, fainting due to needling, stuck needle, infections, and broken needle. In addition, adverse events of drug in the control group were also recorded, such as dry mouth, dry eye, blurred vision, constipation, headache, dizziness, nausea and acute urinary retention.
For statistical analysis, the unpaired Student’s t test was used to test for significant differences between the two groups in continuous variables. SPSS version 16.0 was used for all analyses. A p value <0.05 was considered statistically significant.
Results
Baseline characteristics and OAB symptoms for the study population are summarized in Table 1. A total of 240 women with OAB were enrolled and completed all aspects of the study between July 1, 2010 and March 1, 2014, of which 118 cases were in the intervention group while the other 122 cases in the control group. There were no significant adverse events occurred in the acupuncture treatment group. Ten women in the intervention group were lost of follow-up and did not complete the study because of personal reasons, such as difficulty in scheduling the treatment sessions around their work schedules. Two women discontinued intervention because of unsuccessful treatment or no significant symptom relief and switched to drug therapy. While in the control group six women were lost to follow-up because of personal reasons, and six discontinued treatment because of unsuccessful treatment, no significant symptom relief or moderate to severe dry mouth, three of which switched to bladder training and acupuncture treatment. Patients in the intervention group received 4 weekly acupuncture treatments while those in the control group received a treatment of oral tolterodine tartrate 2 mg twice a day for 4 weeks. Changes from baseline to endpoint in urgency, urgency incontinence, daytime frequency, voided volume and nocturia are summarized in Table 2. At week 4, the number of urgency episodes per 24 h in the intervention group decreased by 3.1 (−47.7 %), urgency incontinence episodes by 1 (−45.5 %), daytime frequency by 4.2 (−30.0 %), nocturia episodes by 1.5 (−37.5 %) and the volume voided per micturition increased by 68 ml (40.0 %), while in the control group, the number of urgency episodes per 24 h decreased by 3.5 (−50 %), urgency incontinence episodes by 1.2 (−48 %), daytime frequency by 4.3 (−32.6 %), nocturia episodes by 1.3 (−36.1 %) and the volume voided per micturition increased by 70 ml (43.2 %). The subjects in both intervention and control groups had significant decreases in number of urinary urgency episodes, incontinence episodes, daytime frequency, nocturia episodes and increase in volume voided per micturition without a significant statistical difference (p > 0.05) in the changes of OAB symptoms between the groups. There were no serious adverse events during the study. Adverse events were generally mild, well tolerated and occurred at very low rates in both groups. Dry mouth was most common with twice daily 2 mg tolterodine tartrate (11 cases), while needling pain was the most common adverse event in acupuncture treatment (9 cases).
Discussion
Overactive bladder is a symptom complex that is characterized by urinary urgency with or without urgency incontinence, urinary frequency and nocturia, for which no precise cause has been identified. It can have a profound effect on quality of life. The normal micturition involves the autonomic and central nervous system. Acupuncture, a unique therapeutic system, has been in constant use throughout the Chinese culture area for some 2500 years. There have been limited studies supporting acupuncture as an effective treatment option for OAB. Aydoğmuş [14] in 2014 reported acupuncture may be considered a treatment option when anticholinergic treatment is contraindicated in a randomized, placebo-controlled clinical trial. Paik [15] in 2013 demonstrated acupuncture exhibited favorable effects on OAB symptoms without any statistically significance in a review article. Although acupuncture as a treatment for OAB is widely accepted in China and other countries, large-scale randomized, controlled, double-blinded trials with high methodological quality are needed to investigate whether or not acupuncture is a potential therapy for female adult with OAB. In this randomized controlled trial, four sessions of weekly acupuncture treatment and 4 weeks’ pharmacological treatment with twice daily 2 mg tolterodine tartrate produced significant improvements in female OAB symptoms although there was no significant statistical difference in the changes of OAB symptoms between the groups. In addition, there were no serious adverse events during the study. Acupuncture is likely to produce its effect through the nervous system inhibiting sensory afferent nerves of bladder, changing the release of neurotransmitters, thus affecting the parts of the central nervous system involved in the control of micturition [16]. The use of acupuncture for OAB can be approached by needling some points such as SP6, SP9, KI3 and CV4, which will invoke a parasympathetic response at a spinal level. The reasoning for the use of these acupuncture points is explained in theory of Traditional Chinese Medicine. SP6 is indicated for disorders of urological, gynecology and genital systems [17, 18]. SP9 is indicated for continence generally. The KI3 is the best point linked to the urinary output. Therefore, it is chosen specially for treating urinary frequency and incontinence. CV4 treats kidney deficiency causing bladder complaints, such as incontinence, incomplete voiding, urinary frequency and urgency [18, 19]. The points were chosen for their direct links with bladder function and their influence on Qi. Acupuncture needle stimulation causing Deqi has been suggested to be important for achieving the maximum therapeutic effect [20]. However, there were considerable variations in selecting of needle insertion points, insertion depth, methods in details and duration across studies relating to acupuncture for OAB [15]. In addition, percutaneous tibial nerve stimulation (PTNS), a clinically significant treatment alternative for OAB, involves insertion of a needle electrode into a similar site to SP6 (Spleen Meridian, Sanyinjiao), thereby, further investigations are warranted to demonstrate the differences between PTNS and traditional Chinese acupuncture in the treatment of OAB [21–23]. However, we acknowledge that this was a short-term study and there might be a placebo effect, and significance for long-term benefit cannot be understood from this study.
Conclusions
This study demonstrates that acupuncture is a potential safe, effective alternative treatment for female adult with OAB. However, the exact mechanism still needs to be investigated and large, international, adequately powered randomized controlled trials are needed to further assess the efficacy of acupuncture for OAB.
References
Abrams P, Cardozo L, Fall M et al (2002) The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn 21:167–178
Stewart WF, Van Rooyen JB, Cundiff GW et al (2003) Prevalence and burden of overactive bladder in the United States. World J Urol 20(6):327–336
Irwin DE, Mungapen L, Milsom I et al (2009) The economic impact of overactive bladder syndrome in six Western countries. BJU Int 103(2):202–209
Lam S, Hilas O (2007) Pharmacologic management of overactive bladder. Clin Interv Aging 2(3):337–345
Ulahannan D, Wagg A (2009) The safety and efficacy of tolterodine extended release in the treatment of overactive bladder in the elderly. Clin Interv Aging 4:191–196
Chapple R, Cardozo L, Steers WD (2006) Solifenacin significantly improves all symptoms of overactive bladder syndrome. Int J Clin Pract 60(8):959–966
Appell RA (1997) Clinical efficacy and safety of tolterodine in the treatment of overactive bladder: a pooled analysis. Urology 50(suppl):90–96
Burgio KL, Locher JL, Goode PS, Hardin JM, McDowell BJ, Dombrowski M et al (1998) Behavioral vs drug treatment for urge urinary incontinence in older women: a randomized controlled trial. JAMA 280:1995–2000
Minni B, Capozza N, Creti G, De Gennaro M, Caione P, Bischko J (1990) Bladder instability and enuresis treated by acupuncture and electro-therapeutics: early urodynamic observations. Acupunct Electrother Res 15:19–25
Chang PL (1988) Urodynamic studies in acupuncture for women with frequency, urgency and dysuria. J Urol 140:563–566
Bergstrom K, Carlsson CP, Lindholm C, Widengren R (2000) Improvement of urge- and mixed-type incontinence after acupuncture treatment among elderly women—a pilot study. J Auton Nerv Syst 79:173–180
Bergström K, Carlsson CP, Lindholm C, Widengren R (2000) Improvement of urge- and mixed-type incontinence after acupuncture treatment among elderly women—a pilot study. J Auton Nerv Syst 79(2–3):173–180
Bradnam L (2007) A proposed clinical reasoning model for Western acupuncture. J Acupunct Assoc Chart Physiother 21–30. http://www.aacp.org.uk/journal-public-archive/194-journal-aacp-2007-spring
Aydoğmuş Y, Sunay M, Arslan H, Aydın A, Adiloğlu AK, Sahin H (2014). Acupuncture versus solifenacin for treatment of overactive bladder and its correlation with urine nerve growth factor levels: a randomized, placebo-controlled clinical trial. Urol Int [Epub ahead of print]
Paik SH, Han SR, Kwon OJ, Ahn YM, Lee BC, Ahn SY (2013) Acupuncture for the treatment of urinary incontinence: a review of randomized controlled trials. Exp Ther Med 6(3):773–780
Sung LM, Jiaqi W. (2006) Acupuncture for urinary incontinence in adults without neurological disease. Cochrane Database of Systematic Reviews: Protocols Issue 4 Wiley, Chichester, UK. Art. No. CD006235
Zhishun L, Baoyan L, Tao Y et al (2002) Clinical study of electroacupuncture treatment of senile urge urinary incontinence. Int J Clin Acupunct 13(4):255–262
Emmons SL, Otto L (2005) Acupuncture for overactive bladder: a randomized controlled trial. Obstet Gynecol 106(1):138–143
Philp T, Shah PJ, Worth PH (1988) Acupuncture in the treatment of bladder instability. Br J Urol 61(6):490–493
Zaslawski CJ, Cobbin D, Lidums E, Petocz P (2003) The impact of site specificity and needle manipulation on changes to pain pressure threshold following manual acupuncture: a controlled study. Complement Ther Med 11(1):11–21
Peters KM, Macdiarmid SA, Wooldridge LS, Leong FC, Shobeiri SA, Rovner ES, Siegel SW, Tate SB, Jarnagin BK, Rosenblatt PL, Feagins BA (2009) Randomized trial of percutaneous tibial nerve stimulation versus extended-release tolterodine: results from the overactive bladder innovative therapy trial. J Urol 182(3):1055–1061
Peters KM, Carrico DJ, Perez-Marrero RA, Khan AU, Wooldridge LS, Davis GL, Macdiarmid SA (2010) Randomized trial of percutaneous tibial nerve stimulation versus Sham efficacy in the treatment of overactive bladder syndrome: results from the SUmiT trial. J Urol 183(4):1438–1443
Finazzi-Agrò E, Petta F, Sciobica F, Pasqualetti P, Musco S, Bove P (2010) Percutaneous tibial nerve stimulation effects on detrusor overactivity incontinence are not due to a placebo effect: a randomized, double-blind, placebo controlled trial. J Urol 184(5):2001–2006
Acknowledgments
I would like to express my sincerest gratitude and appreciation to all those who gave me the possibility to complete this study. Especially, special recognition goes out to Ms Lei Jing and Mr Yuan Leilei, whose support, encouragement and patience helped me all my life.
Conflict of interest
We declare that we have no financial relationships with other people or companies that can inappropriately influence our work.
Ethical standard
The study has been approved by the hospital and the local ethics committee and it conforms to the provisions of the Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yuan, Z., He, C., Yan, S. et al. Acupuncture for overactive bladder in female adult: a randomized controlled trial. World J Urol 33, 1303–1308 (2015). https://doi.org/10.1007/s00345-014-1440-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-014-1440-0