Abstract
Introduction
To evaluate the current role of thulium vapoenucleation of the prostate (ThuVEP) for the treatment of benign prostatic obstruction (BPO).
Methods
A Medline search for randomized trials, case series, and comparative studies being published since the initial description of the ThuVEP procedure (2009–2014) was performed to assess the safety, the perioperative morbidity, the efficacy, and the durability of the technique.
Results
A total of 14 peer-reviewed original articles, seven case series [level of evidence (LOE) 4] and seven comparative studies (LOE 3b), have been identified. ThuVEP has been shown to be a size-independent, safe, efficacious, and durable procedure for the treatment of BPO in large, prospective, and retrospective series (LOE 4/3b). The feasibility and safety of the ThuVEP procedure has also been confirmed in patients at high cardiopulmonary risk on oral anticoagulants (LOE 4). It has also been demonstrated that the erectile function is not impaired by the ThuVEP procedure (LOE 4). However, published ThuVEP series are from very few centers of excellence not exceeding a LOE of 3b. Randomized controlled trials comparing ThuVEP with standard procedures for the treatment of BPO, namely transurethral resection of the prostate, open prostatectomy, or holmium laser enucleation of the prostate, have not been published so far.
Conclusions
ThuVEP appears to be a size-independent, safe, efficacious, and durable procedure for the treatment of BPO (LOE 4/3b). Multicentric PRT are however needed to define the current role of ThuVEP in the armamentarium of minimally invasive transurethral surgery of the prostate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transurethral resection of the prostate (TURP) and open prostatectomy (OP) have been over decades the standard treatment of benign prostatic obstruction (BPO) due to lower urinary tract symptoms (LUTS). However, since the first description of holmium laser enucleation of the prostate (HoLEP) for the treatment of BPO in 1998, the HoLEP technique has gained increasing popularity around the world due to its major advantage of combining complete dissection of the adenoma from the surgical pseudocapsule with very low perioperative morbidity [1]. Since then, the HoLEP procedure has been shown in numerous studies to be a size-independent, safe, and efficacious procedure with excellent long-term results in terms of reoperation and complication rates [2, 3]. Based on the HoLEP technique, a vast variety of so-called me too techniques using different energy sources have been described during the past decade: i.e., transurethral enucleation of the prostate using thulium, diode, and potassium-titanyl-phosphate (KTP) lasers or bipolar energy sources [4]. However, long-term data as well as the number randomized controlled trials (RCT) for transurethral enucleation procedures other than HoLEP are rather limited [2, 3]. One prominent representative of these “new” types of energy sources for transurethral enucleation of the prostate is the thulium:yttrium–aluminum-garnet (Tm:YAG) laser [4]. Bach et al. [5, 6] first described the thulium vapoenucleation of the prostate (ThuVEP) procedure combined with mechanical morcellation in 2009 as a safe and durable procedure. This review focuses on the literature that has been published since the initial description of the ThuVEP procedure to assess the safety, efficacy, and long-term durability of the procedure.
Materials and methods
A Medline search with these keywords was performed: benign prostatic hyperplasia, bladder outlet obstruction, laser, RevoLix, enucleation, prostate enucleation transurethral, ThuVEP, 2 µm continuous wave laser, and ThuLEP. We reviewed the literature regarding the ThuVEP procedure that has been published since its initial description in 2009. Papers dealing with techniques other than the ThuVEP technique, i.e., Tm:YAG vaporization of the prostate (ThuVAP), Tm:YAG vaporesection (ThuVARP), and Tm:YAG laser enucleation of the prostate (ThuLEP), were excluded from further analysis. Therefore, a total of 14 peer-reviewed original articles, seven case series [level of evidence (LOE) 4] and seven comparative studies (LOE 3b), have been identified.
Technical aspects
Three types of thulium lasers have been introduced for the treatment of BPO: a 2.013 nm Tm:YAG laser (2 µm RevoLix®, LISA Laser products, Katlenburg, Deutschland), a 1.940 nm Tm:fiber laser (1.9 µm Vela® XL, Starmedtec, Starnberg, Deutschland), and a 2,010 nm Tm:YAG laser (2 µm Cyber™, QuantaSystem, Solbiate Olona, Italia), respectively. The target chromophore is water, with radiation emission in a continuous wave mode. The wavelength is close to the absorption peak of water and, together with a shallow penetration depth of 0.2 mm, this results in a high-energy density leading to rapid vaporization of water and tissue [7, 8]. The side-fire technique is available, but published applications of the thulium:YAG laser are mainly resection and enucleation procedures using front-firing fibers [9]. Due to the high proportion of vaporization during these procedures, the terms vaporesection and vapoenucleation have been introduced into clinical practice [10].
Surgical technique of the ThuVEP procedure
In principle, all transurethral enucleation techniques for the treatment of BPO are based on the surgical descriptions by Hiraoka et al. and Gilling et al. [1, 11]. Briefly, either the beak of the resectoscope is used to bluntly dissect the prostate off the pseudocapsule, and then the source of energy is used to coagulate the bleeding vessels or the source of energy is continuously applied to the layer of enucleation using a 2-lobe or 3-lobe technique [1, 11]. The blunt enucleation technique using the Tm:YAG laser has been introduced as thulium laser enucleation of the prostate (ThuLEP) [10], while the continuous use of the Tm:YAG laser for dissecting off the prostate from the surgical pseudocapsule was named ThuVEP due to the concomitant excellent vaporization capacities of the Tm:YAG laser during enucleation [10]. The ThuVEP technique was described in the initial publication as follows [5]: “The distal resection border close to the prostatic apex was identified and marked with the Tm:YAG laser. After making a Turner-Warwick-like incision at the 5 and 7 o’clock positions down to the surgical capsule, the median lobe was enucleated in a retrograde manner. The lateral lobes were enucleated by dissecting the prostatic adenoma from the peripheral zone at the layer of the surgical capsule. Enucleated tissue was morcellated in the bladder. Residual apical tissue was vaporized as needed using the vaporizing properties of the Tm:YAG laser device” [5].
The excellent physical properties of the Tm:YAG laser have allowed the use of the ThuVEP technique for larger prostates (>80 ml) [12–14], for patients on oral anticoagulant (OA) therapy [15, 16], for patients at high cardiovascular and pulmonary risk [15, 16], or for patients with acute urinary retention [17], respectively.
Intra- and perioperative morbidity
It has been recently shown that ThuVEP is a safe and effective procedure for the treatment of BPO with low perioperative morbidity, short catheterization times, and hospital stay [13, 14]. Treatment of larger volume prostates (≥80 ml) was not associated with higher blood transfusion rates, prolonged catheterization times, or hospitalization stay compared with medium-sized (40–80 ml) and small-sized prostates (<40 ml) [13, 14] (Table 1). Enucleation efficiency (g/min) as well morcellation efficiency increased significantly with increasing prostate size (Table 1) [13, 14]. Table 1 lists the perioperative data from all ThuVEP series that have been published yet [5, 6, 12–23].
The operative time also increases with prostate size in ThuVEP (Table 1). However, there has been no transurethral resection syndrome (TURS) being reported in the literature after ThuVEP due to the use of physiologic saline as irrigant solution (Table 2) [5, 6, 12–23]. Intraoperative complications such as extraperitoneal fluid collection (range 0–1.6 %), superficial bladder injury during morcellation (range 0–2.8 %), malfunction of the Tm:YAG laser (range 0–0.3 %), capsular perforation (range 0–3.2 %), ureteric orifice injury (range 0–1.4 %), and bladder neck false passage (range 0–1.4 %) have been reported, but the incidence of these complications was low (Table 2 ). In addition, most of these complications could be managed conservatively with prolonged catheterization [13]. Table 2 lists all intraoperative complications that have been reported in detail [6, 12–23].
Although high-risk patients on OA therapy have been treated, the rate of postoperative phlebothrombosis (range 0–0.3 %) and myocardial infarction (range 0–0.09 %) was very low. In addition, the perioperative blood transfusion rate was low and did not depend on prostate size (range 1–2.2 %) [13, 14] (Table 2). However, in patients on OA or with bleeding disorders, the blood transfusion rates were 7.1 and 2.6 %, respectively [15, 16].
Indications for immediate perioperative reoperation (range 0–8.9 %) were secondary morcellation (range 0–2.8 %), ureteral stenting (range 0–1.4 %), secondary apical resection (range 0–3.9 %), and coagulation of the prostate fossa (range 0–3.1 %), respectively (Table 2). To note, the perioperative reoperation rates did not depend on prostate size [13, 14]. On the other hand, the highest perioperative reoperation rate (8.9 %) was found in patients on OA during the ThuVEP procedure [16].
Postoperative functional results—late morbidity
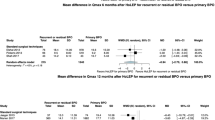
At ≥12-month follow-up, IPSS (≤6.8 vs. ≥18.4), QoL (≤1.8 vs. ≥3.8), Qmax (≥20 vs. ≤10.2 ml/s), and PVR (≤33.5 vs. ≥89.5 ml) improved significantly compared to preoperative assessment [6, 12, 18–21] and continued to do so at 24-month follow-up (Table 3). At 4-years postoperatively, Qmax (20 vs. 7.6 ml/s), PVR (25 vs. 107.5 ml), IPSS (4 vs. 21), and QoL (1 vs. 5) differed significantly from baseline (p < 0.001) [23] (Table 3). The reintervention rates for urethral strictures and bladder neck contractures were ranging from 0 to 3.6 and 0 to 3.6 % at 12-month follow-up, respectively. Table 3 shows the reoperation rates after ThuVEP in series with a follow-up ≥12 months. As expected, the overall reintervention rates (0–2.4 %) in series with a follow-up ≥24 months were low [16, 23], presumably due to peeling off the complete adenoma from the surgical pseudocapsule during ThuVEP.
Postoperative storage symptoms were often reported after transurethral laser treatments of the prostate [2, 3], ranging from 4.3 to 27 % in current ThuVEP series (Table 4). In addition, transient urge and stress incontinence after ThuVEP were reported to occur in up to 7.1 and 17.9 % of the patients [6, 12, 16, 18–21, 23] (Table 4). However, these adverse events usually resolved spontaneously or with conservative treatments (i.e., anti-inflammatory drugs, antibiotic therapy, and pelvic floor exercise). At 12-month follow-up, the incidence of storage symptoms (range 0–4.8 %), urge incontinence (range 0–1.8 %), and stress incontinence (range 0–3.6 %) had significantly decreased [6, 12, 16, 18–21, 23] (Table 4).
Efficacy
PSA and prostate volume decreased significantly from baseline at 12-month follow-up confirming an effective anatomic desobstruction [6, 12, 18–21, 23] (Table 5). The minimum PSA-decrease was 81.0 % (range 81–88 %), and the minimum prostate volume decrease 71.8 % (range 71.8–86 %) at 12-month follow-up, respectively. To note, the series with the lowest prostate volume decrease (71.8 %) was the initial series by Bach et al. [5, 6] which included the learning curve of the ThuVEP procedure.
Learning curve
The shallow learning curve of the HoLEP technique has restricted its use to a limited number of centers worldwide [24]. Reasonable efficiency of HoLEP was found after at least 20–30 procedures [25–27] reaching up to 50 cases in other series [28]. Netsch et al. [21] compared the learning curves of a resident without experience in transurethral prostate surgery (surgeon A) and an experienced endourologist (surgeon B) with those ThuVEP procedures performed by an experienced surgeon in ThuVEP (surgeon C), who served as the mentor for the ThuVEP beginners. As expected, enucleation efficiency (g/min) differed significantly between surgeon A (0.48 ± 0.3), B (0.7 ± 0.36), and C (1.4 ± 0.67; p ≤ 0.001). However, ThuVEP was performed by the ThuVEP beginners with reasonable enucleation and morcellation efficiency after 8–16 procedures (Table 1) [21]. At 12-month follow-up, the functional parameters (IPSS, QoL, Qmax, PVR), PSA, and prostate volume had improved significantly in each surgeon (Table 3). In addition, there were no differences in the incidence of complications among the surgeons during follow-up (Tables 2, 3). Immediate improvement of the functional parameters, reasonable efficiency of enucleation, and morcellation combined with low perioperative morbidity during the initial learning course was found when ThuVEP beginners were closely mentored. These short learning curves were explained by the use of the mentor-based approach and the specific physical properties of the Tm:YAG laser [21]. The energy of the Tm:YAG laser is delivered in a continuous wave mode, which can provide maximum hemostasis and coagulation, to perform a smooth incision or tissue vaporization. This specification allows an uncomplicated correction of the layer of enucleation during ThuVEP or switching from vapoenucleation to vaporesection or pure vaporization, which may facilitate to become adapt with the ThuVEP technique during the initial learning course of the procedure [6, 21, 29].
Sexual dysfunction
The impact of ThuVEP on erectile function (EF) has been demonstrated in one series [22]. Tiburtius et al. evaluated the EF of 72 patients who underwent ThuVEP for the treatment of BPO secondary to LUTS using the EF domain of the International Index of Erectile Function (IIEF-EF). They found a slight but no statistically significant increase of the IIEF-EF domain score at 12-month follow-up (19.5 vs. 20) compared to the preoperative assessment. According to preoperative IIEF-EF score, the 72 patients were classified into subgroup A (IIEF-EF ≥ 19, n = 38) and subgroup B (IIEF-EF < 19, n = 34). Again, a slight nonsignificant increase of the IIEF-EF domain score at 12-month follow-up could be found in subgroup A (25 vs. 26) and B (6 vs. 8). However, data on retrograde ejaculation or IIEF orgasmic function were not presented in this series.
Conclusions
ThuVEP has been shown to be a size-independent, safe, and efficacious procedure for the treatment of BPO secondary to LUTS with low perioperative morbidity and excellent long-outcome regarding micturition improvement and complication rates. However, the ThuVEP series that have been published so far are from few centers of excellence with a maximum LOE of 3b. To the best of our knowledge, no PRT has been published for the ThuVEP procedure so far. Multicentric PRT are however required to investigate ThuVEP in comparison with HoLEP, TURP, and OP to define the current role of ThuVEP in the armamentarium of minimally invasive transurethral surgery of the prostate. To note, the perioperative morbidity of ThuVEP is expected to be lower than in OP. The ThuVEP procedure should therefore be rather compared with HoLEP in large volume prostates.
References
Fraundorfer MR, Gilling PJ (1998) Holmium:YAG laser enucleation of the prostate combined with mechanical morcellation: preliminary results. Eur Urol 33:69–72
Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, Speakman MJ, Stief CG (2010) Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol 58:384–397
Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, McVary K, Novara G, Woo H, Madersbacher S (2014) A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from Benign prostatic obstruction: an update. Eur Urol. pii:S0302-2838(14)00538-7. doi:10.1016/j.eururo.2014.06.017 [Epub ahead of print]
Gilling PJ (2013) Laser enucleation is increasingly becoming the standard of care for treatment of benign prostatic hyperplasia of all sizes. Eur Urol 63:868–869
Bach T, Wendt-Nordahl G, Michel MS, Herrmann TR, Gross AJ (2009) Feasibility and efficacy of Thulium:YAG laser enucleation (VapoEnucleation) of the prostate. World J Urol 27:541–545
Bach T, Netsch C, Haecker A, Michel MS, Herrmann TR, Gross AJ (2010) Thulium:YAG laser enucleation (VapoEnucleation) of the prostate: safety and durability during intermediate-term follow-up. World J Urol 28:39–43
Fried NM, Murray KE (2005) High-power thulium fiber laser ablation of urinary tissues at.1.94 µm. J Endourol 19:25–31
Herrmann TR, Liatsikos EN, Nagele U, Traxer O, Merseburger AS (2011) Guidelines on lasers and technologies. Eur Assoc Urol http://www.uroweb.org/gls/pdf/28%20Laser_LR.pdf
Herrmann TR, Liatsikos EN, Nagele U, Traxer O, Merseburger AS (2012) EAU guidelines panel on lasers, technologies. EAU guidelines on laser technologies. Eur Urol 61:783–795
Bach T, Xia SJ, Yang Y, Mattioli S, Watson GM, Gross AJ, Herrmann TR (2010) Thulium: YAG 2 mum cw laser prostatectomy: where do we stand? World J Urol 28:163–168
Hiraoka Y, Akimoto M (1989) Transurethral enucleation of benign prostatic hyperplasia. J Urol 142:1247–1250
Bach T, Netsch C, Pohlmann L, Herrmann TR, Gross AJ (2011) Thulium:YAG vapoenucleation in large volume prostates. J Urol 186:2323–2327
Gross AJ, Netsch C, Knipper S, Hölzel J, Bach T (2013) Complications and early postoperative outcome in 1080 patients after thulium vapoenucleation of the prostate: results at a single institution. Eur Urol 63:859–867
Netsch C, Tiburtius C, Bach T, Knipper S, Gross AJ (2014) Association of prostate size and perioperative morbidity in thulium:YAG vapoenucleation of the prostate. Urol Int 93:22–28
Hauser S, Rogenhofer S, Ellinger J, Strunk T, Müller SC, Fechner G (2012) Thulium laser (Revolix) vapoenucleation of the prostate is a safe procedure in patients with an increased risk of hemorrhage. Urol Int 88:390–394
Netsch C, Stoehrer M, Brüning M, Gabuev A, Bach T, Herrmann TR, Gross AJ (2014) Safety and effectiveness of thulium vapoenucleation of the prostate (ThuVEP) in patients on anticoagulant therapy. World J Urol 32:165–172
Bach T, Herrmann TRW, Haecker A, Michel MS, Gross AJ (2009) Thulium:yttrium-aluminium-garnet laser prostatectomy in men with refractory urinary retention. BJU Int 104:361–364
Netsch C, Pohlmann L, Herrmann TR, Gross AJ, Bach T (2012) 120-W 2-µm thulium:yttrium-aluminium-garnet vapoenucleation of the prostate: 12-month follow-up. BJU Int 110:96–101
Netsch C, Bach T, Pohlmann L, Herrmann T, Gross AJ (2012) Comparison of 120-200 W 2 μm thulium:yttrium-aluminum-garnet vapoenucleation of the prostate. J Endourol 26:224–229
Netsch C, Bach T, Herrmann TR, Gross AJ (2012) Thulium:YAG vapoenucleation of the prostate in large glands: a prospective comparison using 70- and 120-W 2-µm lasers. Asian J Androl 14:325–329
Netsch C, Bach T, Herrmann TR, Neubauer O, Gross AJ (2013) Evaluation of the learning curve for thulium vapoenucleation of the prostate (ThuVEP) using a mentor-based approach. World J Urol 31:1231–1238
Tiburtius C, Knipper S, Gross AJ, Netsch C (2014) Impact of thulium vapoenucleation of the prostate on erectile function: a prospective analysis of 72 patients at 12-month follow-up. Urology 83:175–180
Netsch C, Engbert A, Bach T, Gross AJ Long-term outcome following thulium vapoenucleation of the prostate. World J Urol 2014 Feb 16 [Epub ahead of print]
Naspro R, Bachmann A, Gilling P, Kuntz R, Madersbacher S, Montorsi F, Reich O, Stief C, Vavassori I (2009) A review of recent evidence (2006–2008) for 532-nm photoselective laser vaporisation and holmium laser enucleation of the prostate. Eur Urol 55:1345–1357
Moody JA, Lingeman JE (2001) Holmium laser enucleation for prostate adenoma greater than 100 gm.: comparison to open prostatectomy. J Urol 165:459–462
Kuntz RM, Lehrich K (2002) Transurethral holmium laser enucleation versus transvesical open enucleation for prostate adenoma greater than 100 gm.: a randomized prospective trial of 120 patients. J Urol 168:1465–1469
El-Hakim A, Elhilali MM (2002) Holmium laser enucleation of the prostate can be taught: the first learning experience. BJU Int 90:863–869
Shah HN, Mahajan AP, Sodha HS, Hegde S, Mohile PD, Bansal MB (2007) Prospective evaluation of the learning curve for holmium laser enucleation of the prostate. J Urol 177:1468–1474
Bach T, Huck N, Wezel F, Häcker A, Gross AJ, Michel MS (2010) 70 vs 120 W thulium:yttrium-aluminium-garnet 2 microm continuous-wave laser for the treatment of benign prostatic hyperplasia: a systematic ex vivo evaluation. BJU Int 106:368–372
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
All included human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the presented studies. Details that might disclose the identity of the subjects under study are omitted. The corresponding author takes on the above responsibilities.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Netsch, C., Bach, T., Herrmann, T.R.W. et al. Update on the current evidence for Tm:YAG vapoenucleation of the prostate 2014. World J Urol 33, 517–524 (2015). https://doi.org/10.1007/s00345-014-1417-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-014-1417-z