Abstract
Purpose
The purpose of the study was to review the existing literature on holmium:yttrium–aluminum–garnet laser lithotripsy regarding lithotripter settings and laser fibers.
Methods
An online search of current and past peer-reviewed literature on holmium laser lithotripsy was performed on several databases, including PubMed, SciElo, and Google Scholar. Relevant studies and original articles about lithotripter settings and laser fibers were examined, and the most important information is summarized and presented here.
Results
We examine how the choice of lithotripter settings and laser fibers influences the performance of holmium laser lithotripsy. Traditional laser lithotripter settings are analyzed, including pulse energy, pulse frequency, and power levels, as well as newly developed long-pulse modes. The impact of these settings on ablation volume, fragment size, and retropulsion is also examined. Advantages of small- and large-diameter laser fibers are discussed, and controversies are highlighted. Additionally, the influence of the laser fiber is examined, specifically the fiber tip preparation and the lithotripter settings’ influence on tip degradation.
Conclusions
Many technical factors influence the performance of holmium laser lithotripsy. Knowing and understanding these controllable parameters allows the urologist to perform a laser lithotripsy procedure safely, efficiently, and with few complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Review
More than half a century has passed since the construction of the first working laser emitter [1], then the world’s first urological laser procedure [2], and the introduction of the first commercial laser lithotripter in the 1980s [3].
The current and widespread use of holmium laser lithotripsy of urinary stones has produced many debates [4, 5]. The best laser lithotripter settings and the most appropriate laser fibers to achieve the best lithotripsy performance are still being refined [6, 7]; hence, a review of the existing literature on lithotripter settings and laser fibers for holmium laser lithotripsy is in order.
To have a better idea of the wide-ranging field of holmium laser lithotripsy and the role of urologists in it, we performed a search on Medline (on July 14, 2014) for the expression “laser lithotripsy” with or without urology-related terms, starting from the first articles published in 1985 until 2013. A total of 1,037 articles were found on laser lithotripsy, and 768 (74.1 %) of the articles had a urological background.
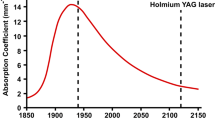
Figure 1 shows the evolution of laser lithotripsy articles that were related to urology and other specialty fields. During the period examined, urology has always been at the center of laser lithotripsy development: since the first medical laser lithotripsy papers appeared in 1985, urology-related applications have accounted for at least half of the articles published on lithotripsy [8–11]. The first urological reports and clinical series on laser lithotripsy appeared almost simultaneously with the launch of the first commercial laser lithotripter in 1988, and with the increase in urological laser lithotripsy in the mid-1990s, urological applications in the literature quickly overshadowed the use of laser lithotripsy in all other medical fields, such as gastroenterology, general surgery, or ENT, to treat, for example, biliary, pancreatic, or salivary stones [3, 12–14]. Currently, laser lithotripsy is established primarily as a urological specialty, with 85–90 % of the articles published in the last 10 years authored by urology-affiliated investigators (Fig. 1). Holmium laser lithotripters were developed several years after the first references to laser lithotripsy. The presence of holmium lasers increased gradually at the turn of the century, and these lasers became highly associated with lithotripsy [15–18]. In contrast to other lasers, holmium laser lithotripters can efficiently fragment any type of urinary stone, and their wavelength of 2,100 nm is almost completely absorbed by water within 0.4 mm of the laser fiber tip, making the Ho:YAG one of the safest lasers to use in an endourological setting [19–21]. The efficacy and safety of the Ho:YAG laser led it to be one of the urologists’ most popular tools for lithotripsy and other urological applications [22].
Laser lithotripter settings
Existing holmium laser lithotripters allow the urologist to control the main parameters, i.e., pulse energy and pulse frequency, and consequently control the total power output, which results from the product of these two parameters: Total Power (W) = Pulse energy (J) × Pulse frequency (Hz). By adjusting these parameters, the urologist decides the energy intensity that is delivered at the tip of the laser fiber to ablate the stone.
Studies have shown that increased pulse energy increased the ablation volume of stones tested in elementary experiments [23–25] and in more elaborate, automated studies [26]. Using different experimental approaches, whether increasing total power [6] or keeping the same total power [26, 27], when the pulse energy rose so did the ablation volume of these stones.
Increased pulse frequency and, consequently, increased total power are expected to increase ablation volume. Some laser lithotripter manufacturers claim that high-frequency settings and high-frequency lithotripters are more ablative [28]; however, experimental results have not verified these claims. Several studies did not measure any significant increase in ablation volume with an increase in pulse frequency [6, 29]. In a more recent study where total power was kept constant, low frequency using high-pulse energy (LoFr–HiPE) settings showed a statistically significant favorable difference over high frequency using low-pulse energy (HiFr–LoPE) settings. Besides showing a directly proportional increase in ablation volume as pulse energy rises, that study also showed how at the same power levels, LoFr–HiPE settings were up to six times more ablative than HiFr–LoPE settings (Fig. 2). In fact, comparison of LoFr–HiPE settings with others using high frequency with significantly higher total power levels showed that even at very high-power settings, these were surpassed by LoFr–HiPE using lower total power settings [26]. Hence, pulse energy was the most important factor that determined ablation volume, with pulse frequency and total power playing a less important role.
Comparison of the results of different lithotripter settings using the same total power level (6 W) and the same laser fiber (200 µm fiber core). a Uses a high-frequency and low-pulse energy (HiFr–LoPE) at 30 Hz × 0.2 J, while b employs a low frequency using high-pulse energy (LoFr–HiPE) at 5 Hz × 1.2 J
More recently, long-pulse lithotripsy has become available. In newer lithotripter models, the urologist can choose different pulse durations, i.e., the traditional short-pulse mode and the new long-pulse mode [30, 31]. Other laser lithotripter settings remain the same, with the same pulse frequency, the same pulse energy, the same power level, and therefore, the same amount of energy delivered per unit of time. In the short-pulse mode, the energy delivered by a single laser pulse occurs during a certain period of time, while in long-pulse mode, that same amount of energy is distributed over a longer period of time. We have compared short-pulse mode with long-pulse mode (180–330 vs. 650–1,215 µs) at different pulse frequencies and pulse energies (HiFr–LoPE at 20 Hz × 0.5 J vs. LoFr–HiPE at 5 Hz × 2.0 J) and using different stone materials (artificial stones made of plaster of Paris vs. BegoStone). Figure 3 shows that the short-pulse mode was significantly more ablative than the long-pulse mode (p < 0.0001): short-pulse mode ablated 25.0 and 9.9 % more on average than long-pulse mode at LoFr–HiPE and HiFr–LoPE settings, respectively. Additionally, in long-pulse mode, LoFr–HiPE settings ablated significantly more than HiFr–LoPE settings. In that same study, we found harder stone material to be more difficult to ablate than softer stone material no matter what the pulse duration was, corroborating our previous studies [26, 32, 33]. Some of these relationships have also been verified by other authors such as Wezel et al. [27].
Comparison of the traditional short-pulse mode with the recently developed long-pulse mode of new laser lithotripters (in this case of a Rocamed™-MH 01-ROCA FTS 30 laser lithotripter). Regardless of laser settings or stone material, the traditional short-pulse mode is significantly more ablative than the long-pulse mode
Debate continues about the fragment size resulting from one laser lithotripter setting or another. Some argue that low-pulse energy, like HiFr–LoPE settings, produces smaller stone fragments (the so-called “dusting effect”) than high-pulse energy, such as LoFr–HiPE settings [5, 6, 34]; however, most of these studies used irregular or handheld approaches. By contrast, automated and reproducible testing systems, similar to the one we use, failed to retrieve any measurable fragments in any of the studies to date. Fragment size may be less related to laser lithotripter settings and more dependent on the surgical technique employed, i.e., how the surgeon approaches the stone with the laser, and whether the stone is repeatedly perforated, chipped, or fragmented, in comparison with worked on at the surface, by “dancing” or “painting” it with the laser [35, 36]. This remains to be investigated. Nevertheless, whichever laser lithotripter setting or ablation technique is used, surgeons must pay attention to the resulting stone fragment size. Numerous large fragments may significantly increase the operating time, require the use of an expensive stone-removal device or of a specific laser lithotripsy technique, such as the “popcorn effect,” to reduce the stone burden [26, 29].
Laser lithotripter settings also affect retropulsion. Retropulsion is known to reduce lithotripsy efficacy, increase operating time and, sometimes, making ureteral calculi inaccessible by pushing them into the renal pelvis [37]. Higher pulse energy levels, as well as the traditional short-pulse mode, increase retropulsion [37–40]. In situations where retropulsion needs to be minimized, lowering the pulse energy or changing to long-pulse mode would decrease the retropulsion effect but would also affect ablation efficiency negatively. When calculi are only slightly influenced or completely unaffected by retropulsion, due to their size, location, being fixed or impacted, more efficient LoFr–HiPE settings can be safely used to accelerate the procedure [26].
Laser fibers
The laser fiber also plays a fundamental role in the lithotripsy procedure. Several components and properties of the laser fiber, such as its diameter, the preparation or shape of its tip, or even its degradation, affect the direct ablation of the calculi and the intervening instruments, e.g., the ureterorenoscopes.
Contradictory reports have emerged concerning fiber diameter and lithotripsy performance, where some authors claim that larger-diameter fibers ablate more than smaller-diameter fibers [38], while others claim that larger fibers ablate less than smaller fibers [24]. Some researchers found no relationship between fiber size and ablation volume [27, 40]. Our previous research showed that larger-diameter fibers do indeed create wider ablation fissures (p < 0.00001), while smaller-diameter fibers generate deeper ablation fissures (p < 0.00001), but neither surpassed the other in terms of ablation volume (p = 0.81) [26]. There is only one particular condition in which large fibers may be less ablative, that is, if very low-pulse energies are employed (e.g., 0.2 J), the energy density may be too low to exceed the ablation threshold. Therefore, a larger-diameter fiber with a larger fiber tip surface area may be significantly less ablative than a smaller-diameter fiber [26, 39]. In addition, larger fibers also increase the retropulsion effect when compared to smaller fibers [37].
Larger laser fibers have another limitation when considering the setting that they are most frequently used in, i.e., inserted inside the small working channels of ureterorenoscopes. Larger laser fibers affect the degree of scope deflection negatively and limit the range of a flexible scope and its ability to reach difficult intrarenal locations, like lower calices [4, 41]. Additionally, larger laser fibers inside narrow working channels influence irrigation rates negatively, which can impair the surgeons’ visualization of structures and, therefore, influence operating time [41, 42].
A recent and awarded abstract presentation casted some serious doubt on the reliability of the laser fibers’ advertised diameters [43–45]. Multiple laser fibers from different manufacturers were measured, and none of the tested fibers matched the advertised diameter. Some fibers were more than double as thick as advertised, and fibers from different manufacturers advertised with the same diameter were in fact significantly different. Ambiguous information has also arisen from industry representatives of the laser fibers that were evaluated; hence, the authors concluded that most information conveyed to urologists regarding laser fiber diameter may be incorrect [45]. Few authors noticed this fiber diameter discrepancy and even less foresaw its severe implications [46, 47]. Considering the previously described influence that laser fiber diameter exerts on the lithotripsy procedure, this misinformation about laser fiber diameter has a critical impact.
Similarly to other working tools and materials, laser fibers do also wear off. During laser emission, the laser fiber tip degrades because of the “burn-back effect” [46, 48, 49]. High-pulse energy and small-diameter laser fibers are also known to increase the burn-back of the fiber [48]. During our research, we confirmed that high-pulse energy settings are more deleterious to the fiber tip than low-pulse energy settings. Additionally, we found that harder stone material promotes more fiber tip degradation by opacification and burn-back of the fiber tip [33]. When comparing the effect of pulse length on the fiber, damage to the laser fiber tip is considerably less evident if long-pulse mode is used instead of short-pulse mode (Fig. 4) [32].
Fiber tip degradation using short-pulse or long-pulse mode. Both modes show more tip degradation with higher pulse energy settings, and with harder stone material, regardless of lithotripter settings [33]. The long-pulse mode seems to spare the cladding and the fiber tip, showing less cladding degradation as well as less fiber tip opacification
An overview of the previous laser lithotripter settings and laser fiber-related evidence is presented and summarized in Table 1.
Another important issue regarding the laser fiber tip concerns its preparation before use. Current practice is to cleave the laser fiber tip with specialized tools and strip several millimeters from the terminal portion of the polymer coating. This preparation ensures the reusability of the laser fiber and prevents any possible performance degradation from previous laser emission, which urologists believe results in better lithotripsy performance [48, 50, 51]. We recently performed a study analyzing the benefits of stripping the laser fiber or leaving the laser fiber-coated, and compared the difference between cleaving the laser fiber with specialized ceramic scissors and using simple metal scissors. Results were recently presented [32] and published [33], and showed that stripping the laser fiber reduces ablation efficiency significantly (p < 0.00001), and no differences were found between metal and specialized ceramic scissors, as long as the fiber tip remained coated. These startling results raise many doubts about the current and widespread practice of laser fiber tip preparation.
One abstract presentation at the 2014 meeting of the American Urological Association by Vassantachart et al. [52] examined the energy output at the tip of laser fibers that were prepared with different cleaving techniques. The authors showed that energy transmission at the fiber tip was best when the fiber tip was new or when special cleaving tools were used. The lowest energy transmission occurred when suture scissors were used to cleave the laser fiber. Unfortunately, this study did not validate the findings of lithotripsy studies using real stones. We performed a similar study analyzing laser light dispersion patterns of new fibers and fibers prepared with metal (suture) scissors, and examined these patterns before and after lithotripsy. As expected, and in accordance with our previous experiments, the light dispersion patterns of different fibers after lithotripsy were almost undistinguishable from one another (Fig. 5), further putting into question the importance of specialized and time-consuming fiber tip preparation.
In summary, there are many controllable factors influencing the outcome of laser lithotripsy procedures, but some are more relevant than others. Pulse energy is one of the key elements that affect ablation and procedure speed, especially if the total power remains at the same level. On the contrary, higher power levels and high frequency lithotripsy are not necessarily associated with a better ablation performance. Recently developed long-pulse settings are significantly less ablative than traditional short-pulse lithotripter settings, but also cause less fiber tip degradation. So far, no reliable study has proven that any particular lithotripter setting is better than another with respect to the avoidance of large stone fragment generation. Concerning laser fibers, most of the information regarding their advertised diameter seems to be incorrect. Although small-diameter fibers ablate as much as their large-diameter counterparts, they are more prone to fiber tip degradation. However, this disadvantage is largely compensated for by better irrigation, better scope deflection, and less retropulsion, which lead to less bothersome procedures with fewer complications. Current fiber tip preparation methods, including stripping and cleaving with specialized tools, are redundant and sometimes counterproductive, and reduce ablation efficacy. Further research using reproducible testing methods is needed to increase our understanding of laser lithotripsy.
References
Maiman TH (1960) Stimulated optical radiation in ruby. Nature 187(4736):493–494
Parsons RL, Campbell JL, Thomley MW (1968) Carcinoma of the penis treated by the ruby laser. J Urol 100(1):38–39
U.S. Corporate news: news from candela corporation. laser medicine and surgery news and advances (1988) 6(5):24–5
Kuo RL, Aslan P, Zhong P et al (1998) Impact of holmium laser settings and fiber diameter on stone fragmentation and endoscope deflection. J Endourol 12(6):523–527
Spore SS, Teichman JM, Corbin NS et al (1999) Holmium: YAG lithotripsy: optimal power settings. J Endourol 13(8):559–566
Sea J, Jonat LM, Chew BH et al (2012) Optimal power settings for holmium:YAG lithotripsy. J Urol 187(3):914–919
Patel AP, Knudsen BE (2014) Optimizing use of the holmium:YAG laser for surgical management of urinary lithiasis. Curr Urol Rep 15(4):397
Hofstetter A (1985) Laser–science fiction or a new dimension in medicine? Urologe A 24(6):310–312
Li AA (1985) Physical methods in the treatment of patients with kidney and ureteral calculi. Vopr Kurortol Fizioter Lech Fiz Kult 4:65–68
Schmidt-Kloiber H, Reichel E, Schoffmann H (1985) Laserinduced shock-wave lithotripsy (LISL). Biomed Tech (Berl) 30(7–8):173–181
Zhang QL, Fujita R, Satake Y (1985) Laser-beam lithotripsy for bile duct stone via percutaneous-transhepatic cholangioscopy. Chin Med J (Engl) 98(9):638–642
Coptcoat MJ, Ison KT, Watson G et al (1988) Lasertripsy for ureteric stones in 120 cases: lessons learned. Br J Urol 61(6):487–489
Hofmann R, Hartung R (1988) Use of pulsed Nd:YAG laser in the ureter. Urol Clin N Am 15(3):369–375
Ritchey M, Patterson DE, Kelalis PP et al (1988) A case of pediatric ureteroscopic lasertripsy. J Urol 139(6):1272–1274
Adkins WC, Dulabon DA, Chorazy ZJ et al (1994) Consider Ho:YAG for low-cost, effective laser lithotripsy. Clin Laser Mon 12(9):139–141
Denstedt JD, Razvi HA, Sales JL et al (1995) Preliminary experience with holmium: YAG laser lithotripsy. J Endourol 9(3):255–258
Matsuoka K, Iida S, Nakanami M et al (1995) Holmium: yttrium–aluminum–garnet laser for endoscopic lithotripsy. Urology 45(6):947–952
Erhard MJ, Bagley DH (1995) Urologic applications of the holmium laser: preliminary experience. J Endourol 9(5):383–386
Leveillee RJ, Lobik L (2003) Intracorporeal lithotripsy: which modality is best? Curr Opin Urol 13(3):249–253
Bader MJ, Gratzke C, Hecht V et al (2011) Impact of collateral damage to endourologic tools during laser lithotripsy—in vitro comparison of three different clinical laser systems. J Endourol 25(4):667–672
Floratos DL, La de Rosette JJ (1999) Lasers in urology. BJU Int 84(2):204–211
Vicente Rodríguez JJ, Fernández González I, Hernández Fernández C et al (2006) Láser en urología. Actas Urológicas Españolas 30:879–895
Teichman JM, Vassar GJ, Glickman RD (1998) Holmium:yttrium–aluminum–garnet lithotripsy efficiency varies with stone composition. Urology 52(3):392–397
Vassar GJ, Teichman JM, Glickman RD (1998) Holmium:YAG lithotripsy efficiency varies with energy density. J Urol 160(2):471–476
Jelinkova H, Köhler O, Miyagi M et al (2009) Comparison of Ho:YAG and Er:YAG lasers for lithotripsy. Photon Ther Diagn V 7161(1):71611H
Kronenberg P, Traxer O (2014) In vitro fragmentation efficiency of holmium: yttrium–aluminum–garnet (YAG) laser lithotripsy: a comprehensive study encompassing different frequencies, pulse energies, total power levels and laser fibre diameters. BJU Int 114(2):261–267
Wezel F, Häcker A, Gross AJ et al (2010) Effect of pulse energy, frequency and length on holmium:yttrium–aluminum–garnet laser fragmentation efficiency in non-floating artificial urinary calculi. J Endourol 24(7):1135–1140
Lumenis (2013) VersaPulse PowerSuite Brochure; PB-1106750 Rev B 2013 [cited 2014 Jun 19]. http://www.surgical.lumenis.com/pdf/PB-1106750_rB_VPPS_P20v_br_LowRes%20(1).pdf
Chawla SN, Chang MF, Chang A et al (2008) Effectiveness of high-frequency holmium:YAG laser stone fragmentation: the “popcorn effect”. J Endourol 22(4):645–650
Electro Medical Systems (2012) Swiss Laserclast Brochure; FA-398 [cited 2014 Jun 19]. http://www.ems-company.com/media/PDF%20NEW/FA-398_EN_Ed_08-2012_LaserClast%20Brochure_single.pdf
Rocamed (2013) MH01 Laser Lithotripter Brochure; V.Uk.2 [cited 2014 Jun 19]. http://www.rocamed-urology.com/images/stories/doc/br.uk.v2.laser.pdf
Kronenberg P, Traxer O (2014) V-10 Strippers, scissors and laser fiber tips. Video presentation at the 4th international meeting challenges in endourology, Paris [cited 2014 Jun 19]
Kronenberg P, Traxer O (2014) Are we all doing it wrong?—Influence of stripping and cleaving methods of laser fibers on laser lithotripsy performance. J Urol in press; accepted 2014 Jul 28; published online 2014 Aug 04. doi:10.1016/j.juro.2014.07.110
Corbin NS, Teichman JM, Nguyen T et al (2000) Laser lithotripsy and cyanide. J Endourol 14(2):169–173
Al-Kandari AM, Desai M, Shokeir AA et al (2013) Difficult cases in endourology. Springer, London
Hecht SL, Wolf JS (2013) JR. techniques for holmium laser lithotripsy of intrarenal calculi. Urology 81(2):442–445
Kronenberg P, Traxer O (2013) V1718 laser fibers, pulse energy and retropulsion-what we can see and what we can’t. J Urol 189(4):e707
Kang HW, Lee H, Teichman JMH et al (2006) Dependence of calculus retropulsion on pulse duration during Ho: YAG laser lithotripsy. Lasers Surg Med 38(8):762–772
Blackmon RL, Irby PB, Fried NM (2011) Comparison of holmium:YAG and thulium fiber laser lithotripsy: ablation thresholds, ablation rates, and retropulsion effects. J Biomed Opt 16(7):71403
Lee H, Ryan RT, Kim J et al (2004) Dependence of calculus retropulsion dynamics on fiber size and radiant exposure during Ho:YAG lithotripsy. J Biomech Eng 126(4):506–515
Pasqui F, Dubosq F, Tchala K et al (2004) Impact on active scope deflection and irrigation flow of all endoscopic working tools during flexible ureteroscopy. Eur Urol 45(1):58–64
Bach T, Geavlete B, Herrmann TRW et al (2008) Working tools in flexible ureterorenoscopy–influence on flow and deflection: what does matter? J Endourol 22(8):1639–1643
Kronenberg P, Traxer O (2013) E60 the truth about laser fiber diameters. Eur Urol Suppl 12(3):50
European Association of Urology (2013) Information conveyed to urologists regarding laser fiber diameter is incorrect. ScienceDaily 2013 Sep 17 [cited 2014 Jul 17]. http://www.sciencedaily.com/releases/2013/09/130917124821.htm
Kronenberg P, Traxer O (2014) The truth about laser fiber diameters. Urology in press; accepted 2014 Aug 18
Khemees TA, Shore DM, Antiporda M et al (2013) Evaluation of a new 240-μm single-use holmium:YAG optical fiber for flexible ureteroscopy. J Endourol 27(4):475–479
Monga M (2013) Ureteroscopy: indications, instrumentation & technique. Totowa, NJ: Humana Press; 2013. (Curr Clin Urol)
Mues AC, Teichman JMH, Knudsen BE (2009) Quantification of holmium:yttrium aluminum garnet optical tip degradation. J Endourol 23(9):1425–1428
Blackmon RL, Irby PB, Fried NM (2010) Thulium fiber laser lithotripsy using tapered fibers. Lasers Surg Med 42(1):45–50
Bagley DH, Das A (2001) Endourologic use of the holmium laser. Teton NewMedia, Jackson
Knudsen BE, Pedro R, Hinck B et al (2011) Durability of reusable holmium:YAG laser fibers: a multicenter study. J Urol 185(1):160–163
Vassantachart J, Lightfoot M, Maldonado J et al (2014) PD7-11 laser fiber cleaving techniques–the effect upon energy output and tip morphology. J Urol 191(4 Supplement):e187–e188
Robinson M, Teichman JMH (2013) 1063 laser lithotripsy retropulsion varies with stone mass. Eur Urol Suppl 12(1):e1063
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
The manuscript does not contain clinical studies or patient data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kronenberg, P., Traxer, O. Update on lasers in urology 2014: current assessment on holmium:yttrium–aluminum–garnet (Ho:YAG) laser lithotripter settings and laser fibers. World J Urol 33, 463–469 (2015). https://doi.org/10.1007/s00345-014-1395-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-014-1395-1